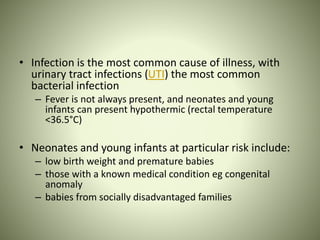
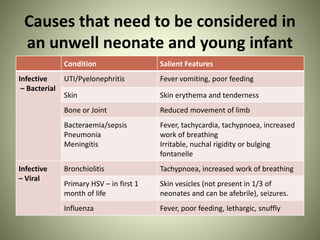
- A neonate presenting as unwell requires prompt assessment and consideration of serious illnesses like sepsis, congenital heart disease, and metabolic disturbances.
- A structured evaluation of vital signs, history, and physical exam can help identify concerning symptoms suggesting an underlying illness and guide appropriate management and investigations.
- Initial management should include empiric antibiotics, fluid resuscitation if needed, and treatment targeted to the suspected condition while consulting pediatric specialists. Ongoing monitoring is needed until the neonate's condition is stabilized.