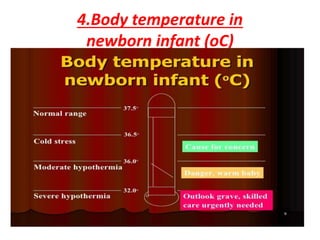
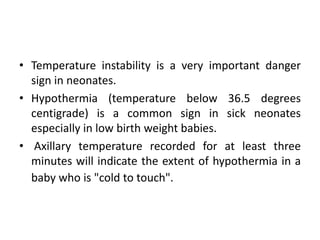
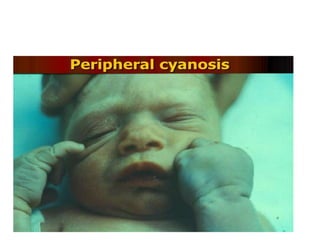
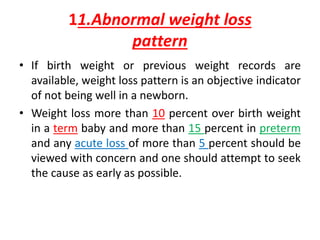
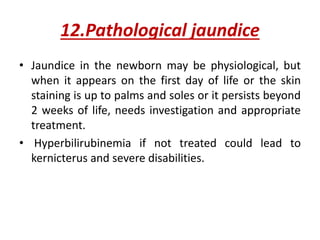
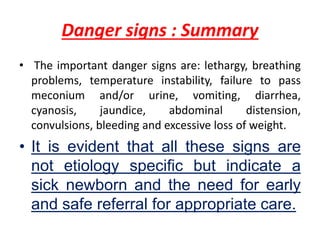
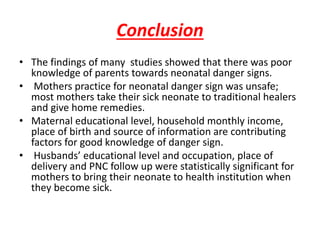
This document discusses important danger signs in newborns that indicate a high risk of morbidity or mortality. It outlines several key danger signs such as lethargy, breathing difficulties, temperature instability, failure to urinate or pass meconium, vomiting, diarrhea, cyanosis and jaundice. The document emphasizes that newborns presenting with any of these non-specific signs should be carefully assessed and referred to a healthcare facility for appropriate care and intervention if needed, as newborns are most vulnerable in the first month of life. Early recognition of danger signs and treatment is crucial to improving newborn survival rates.