This document provides information on Ankylosing Spondylitis (AS), including:
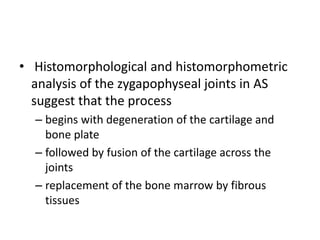
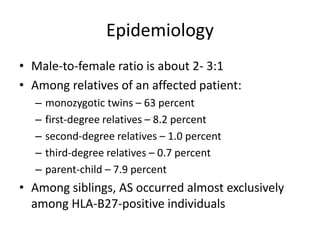
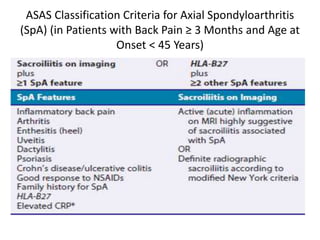
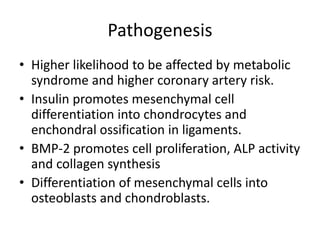
- It is an inflammatory arthritis affecting the spine and sacroiliac joints, causing stiffness and fusion of the joints. HLA-B27 gene and TNF play a role in its pathogenesis.
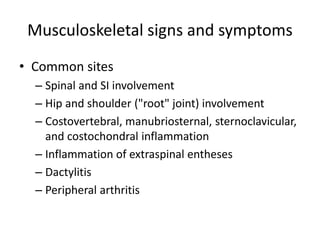
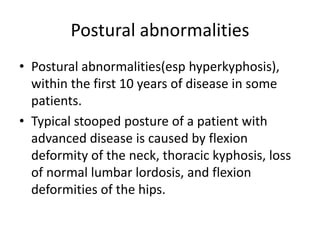
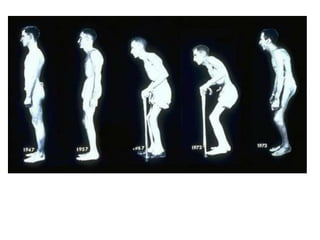
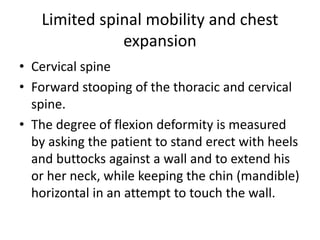
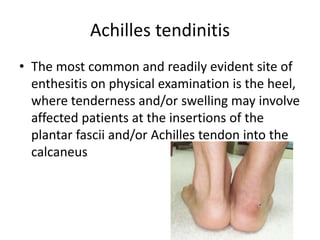
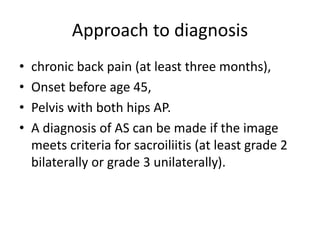
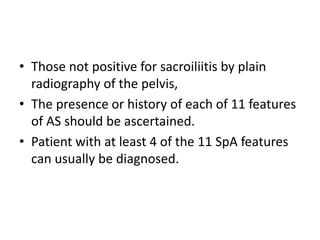
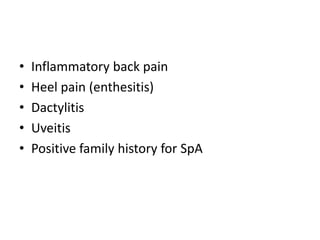
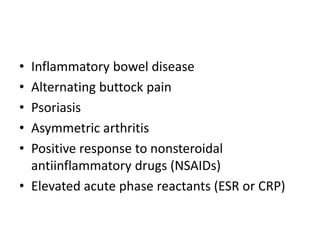
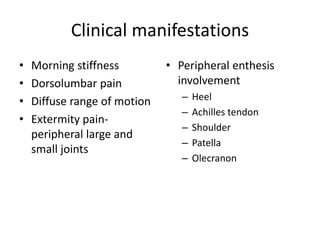
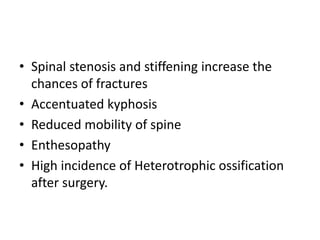
- Signs and symptoms include back pain, limited spinal mobility, chest expansion and peripheral joint involvement. Imaging shows bone erosion and formation in affected areas.
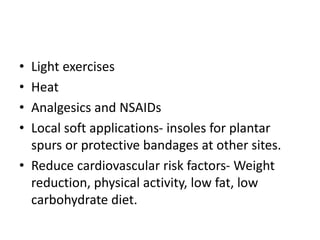
- Treatment involves exercise, NSAIDs, and biologics targeting TNF. Surgery may be needed in advanced cases to correct deformities.