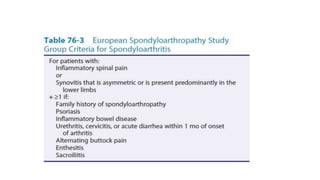
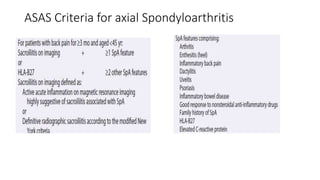
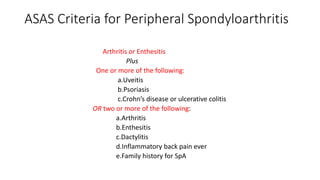
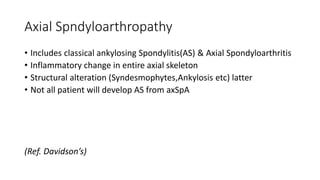
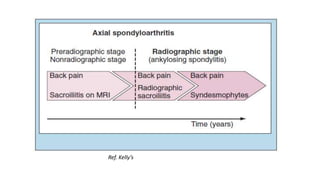
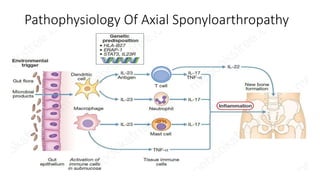
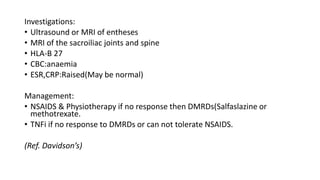
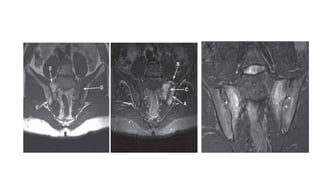
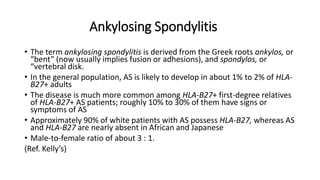
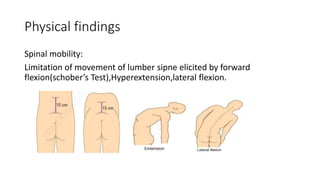
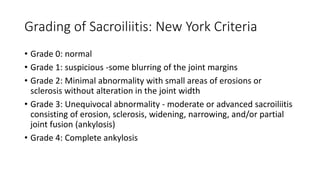
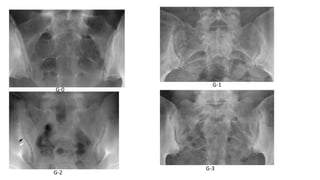
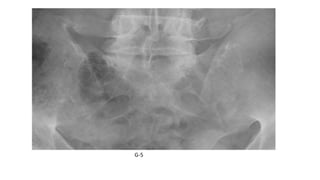
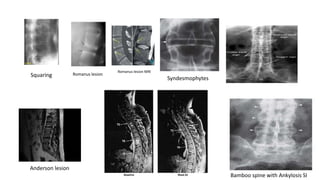
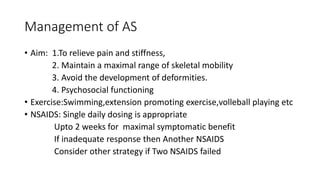
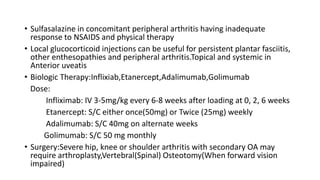
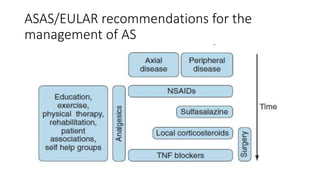
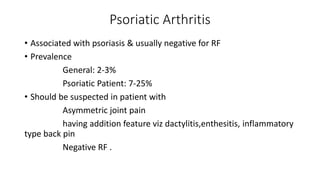
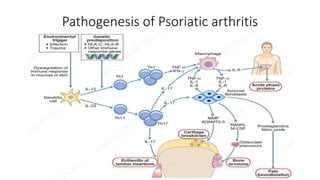
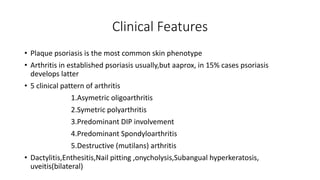
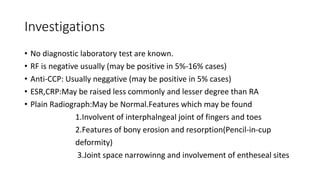
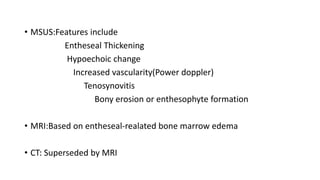
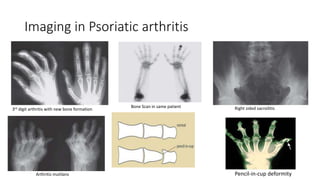
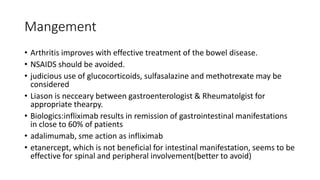
Spondyloarthropathies (SpAs) are a group of related inflammatory musculoskeletal diseases characterized by their overlap in clinical features and a shared association with HLA-B27. This document outlines the various types of SpAs, including axial spondyloarthritis, ankylosing spondylitis, and psoriatic arthritis, along with diagnostic criteria, clinical features, and management strategies. It also discusses the pathophysiology and investigations required for diagnosis and treatment, emphasizing the importance of a multidisciplinary approach involving rheumatologists and gastroenterologists for related conditions.