1) The document discusses a project called HTAIm (Health Technology Assessment and Implementation) which aims to support better decisions in healthcare through evaluating health technologies.
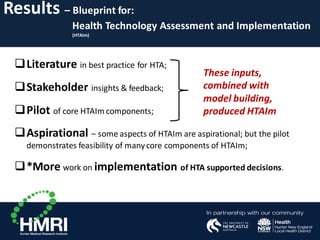
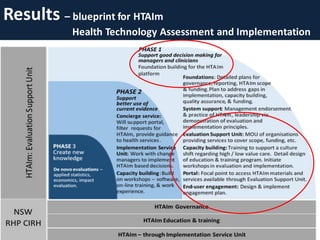
2) HTAIm was designed through literature reviews, stakeholder consultations, and iterative model building. It provides a blueprint for conducting health technology assessments that consider local context.
3) Case studies show HTAIm can identify low-value care and reduce costs, such as through an aged care emergency program that avoided ambulance transfers and ED presentations, saving $920,000 annually.