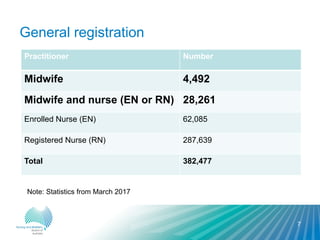
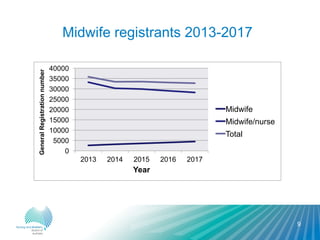
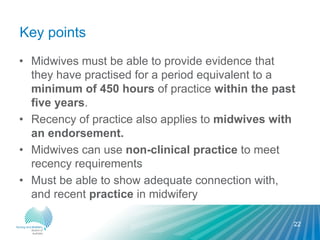
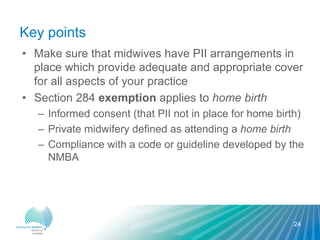
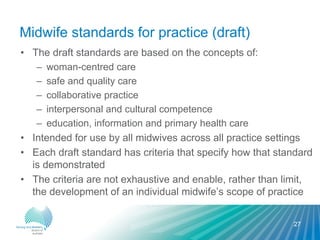
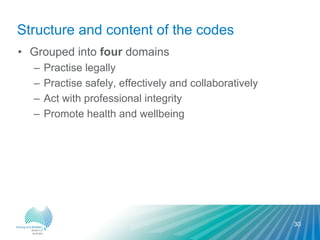
The document provides an overview of the regulation of midwifery in Australia. It discusses the Nursing and Midwifery Board of Australia (NMBA) which sets standards and guidelines for midwives. It notes there are over 4,000 registered midwives in Australia. The professional requirements for midwives include maintaining registration, meeting registration standards, and following the standards for practice, codes and guidelines to ensure safe and competent care.