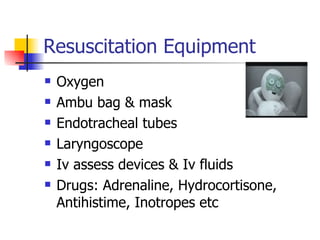
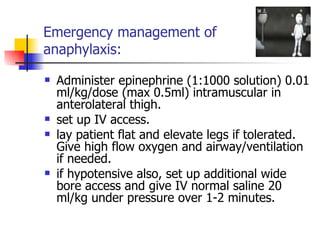
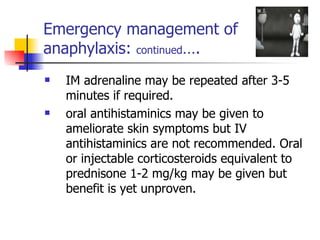
This document discusses adverse events following vaccination (AEFV), including definitions, classifications, common reactions, emergency management, controversies, and legal issues. It emphasizes that vaccines are largely safe, but serious adverse outcomes are usually due to programmatic or human errors. It concludes that vaccines should only be used as recommended and medical staff must be prepared to handle any adverse events.