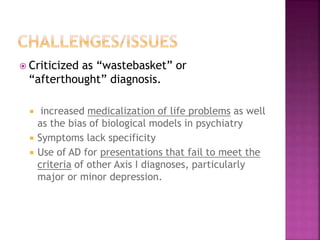
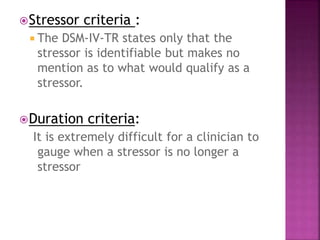
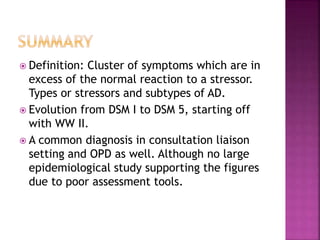
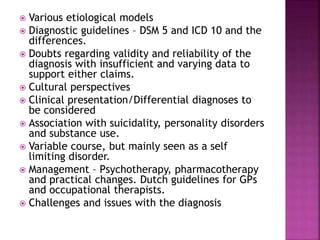
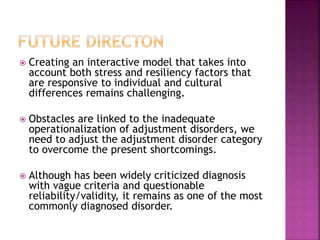
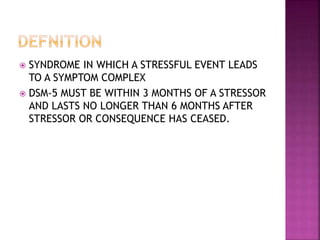
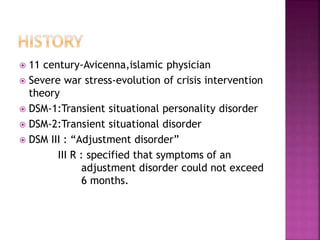
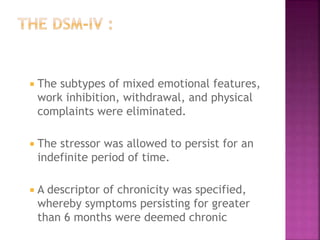
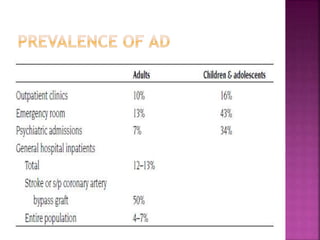
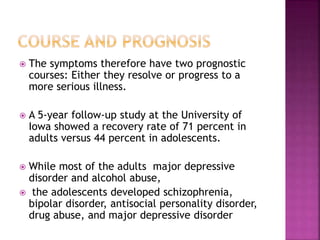
The document discusses adjustment disorder, including its definition as a stress-related symptom complex occurring within 3 months of a stressor. It outlines the evolution of the diagnosis from the 11th century to DSM-5 and reviews epidemiology, diagnostic guidelines, clinical presentation, course/prognosis, management, and challenges regarding the diagnosis. While criticized as vague, adjustment disorder remains one of the most commonly diagnosed disorders, especially in consultation-liaison settings. Improving operationalization of the diagnosis is needed to address its shortcomings.



![ Ego enhancing therapy was found to be
useful during periods of transition in older
patients. This approach promotes the coping
strategy and helps the patient acknowledge
the stressors. [Frankel]
“Mirror therapy”, a therapy including
psychocorporeal, cognitive, and
neurolinguistics components, was effective in
patients with adjustment disorder secondary
to myocardial infarction
Other studies have demonstrated efficacy for
Kava-Kava and Ginkgo Biloba.](https://image.slidesharecdn.com/adjustmentdisorder-230814165135-0a1cff75/85/Adjustment-disorder-in-Psychiatry-41-320.jpg)
![ The basic pharmacological management of
adjustment disorder consists of symptomatic
treatment of insomnia, anxiety and panic
attacks.
Agents commonly used : benzodiazepines and
antidepressants.
Nguyen [80] in 2006 explored the differences in
treating Adjustment Disorder with Anxiety with
etifoxine (a nonbenzodiazepine anxiolytic drug)
and lorazepam.
A pilot study of cancer patients with anxious and
depressed mood found trazodone superior to a
benzodiazepine](https://image.slidesharecdn.com/adjustmentdisorder-230814165135-0a1cff75/85/Adjustment-disorder-in-Psychiatry-42-320.jpg)
![ It is a shared opinion that currently,
psychotherapy remains the treatment of
choice for adjustment disorders.
Maina et al. [68] in 1999 effectiveness of
brief dynamic psychotherapy and brief
supportive psychotherapy in the treatment of
minor depressive episodes.
Interpersonal psychotherapy :](https://image.slidesharecdn.com/adjustmentdisorder-230814165135-0a1cff75/85/Adjustment-disorder-in-Psychiatry-43-320.jpg)