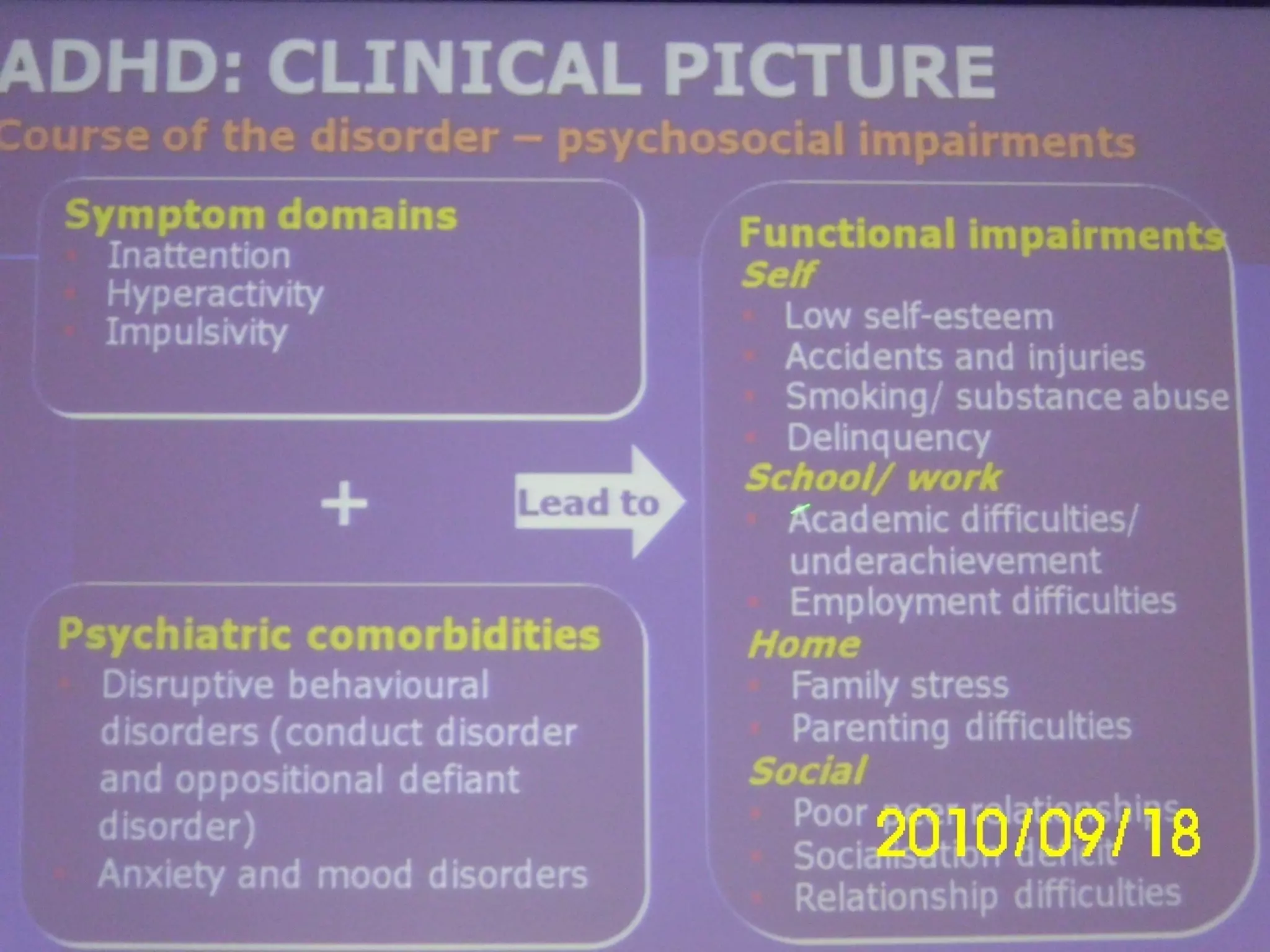
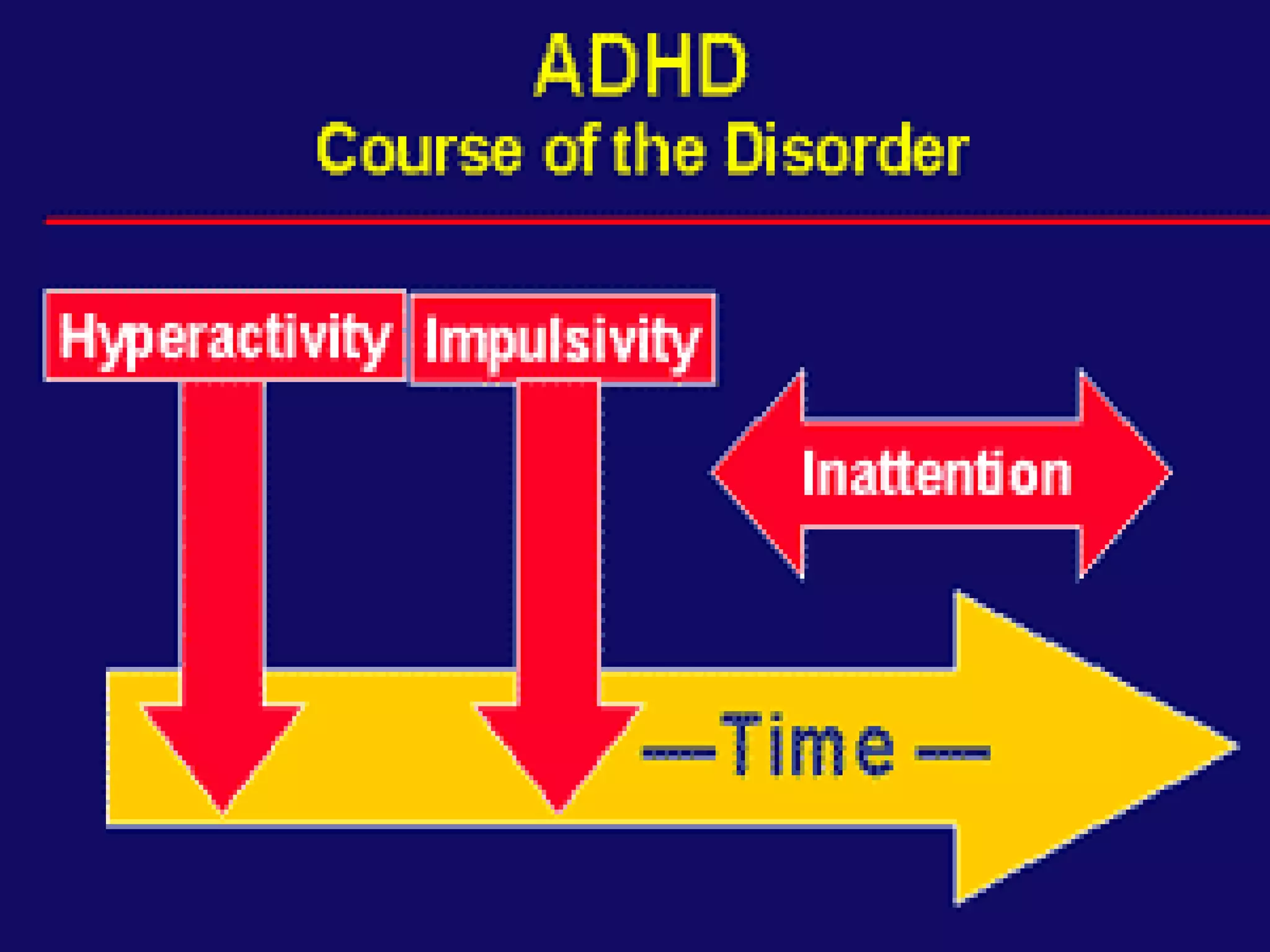
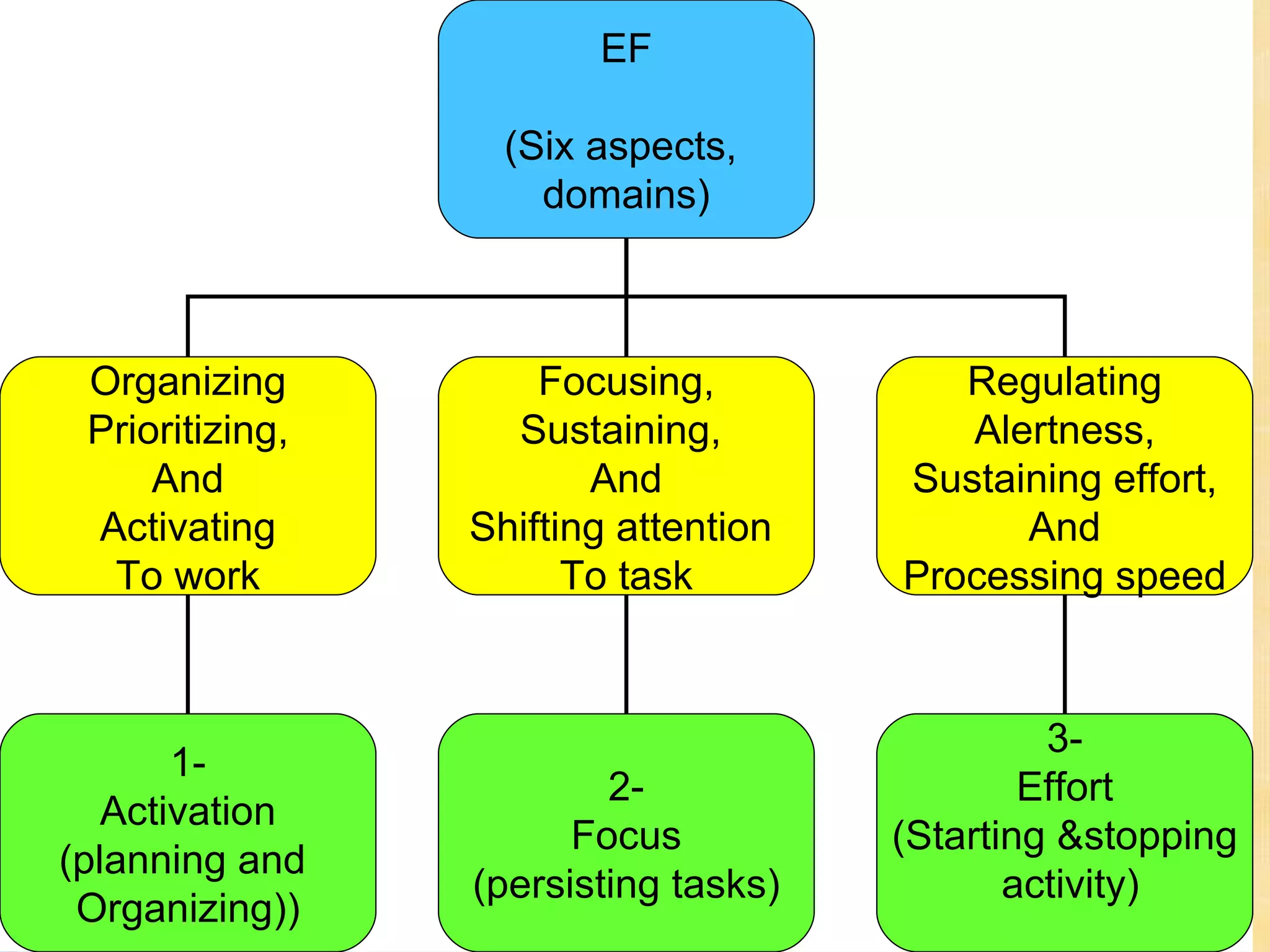
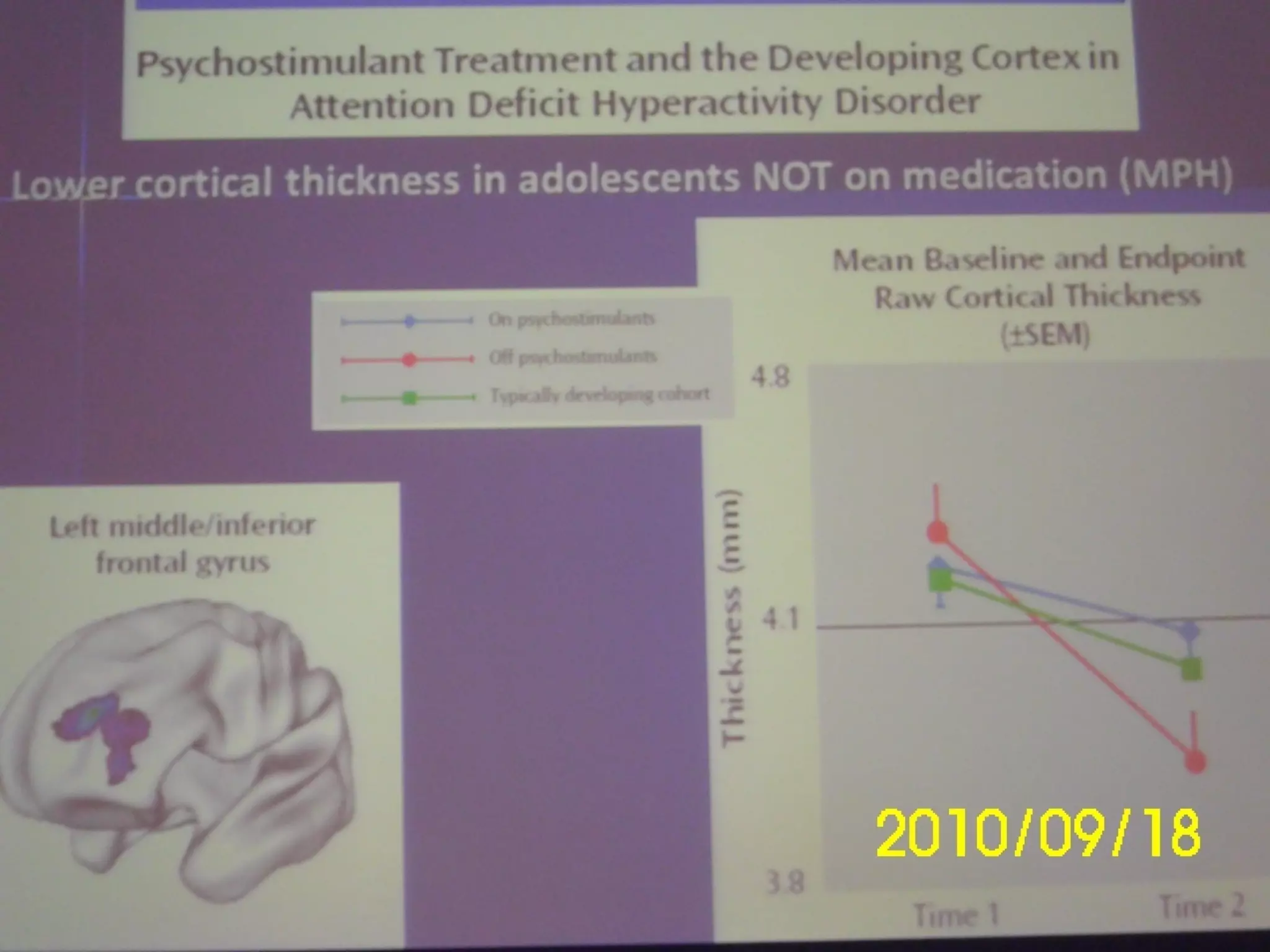
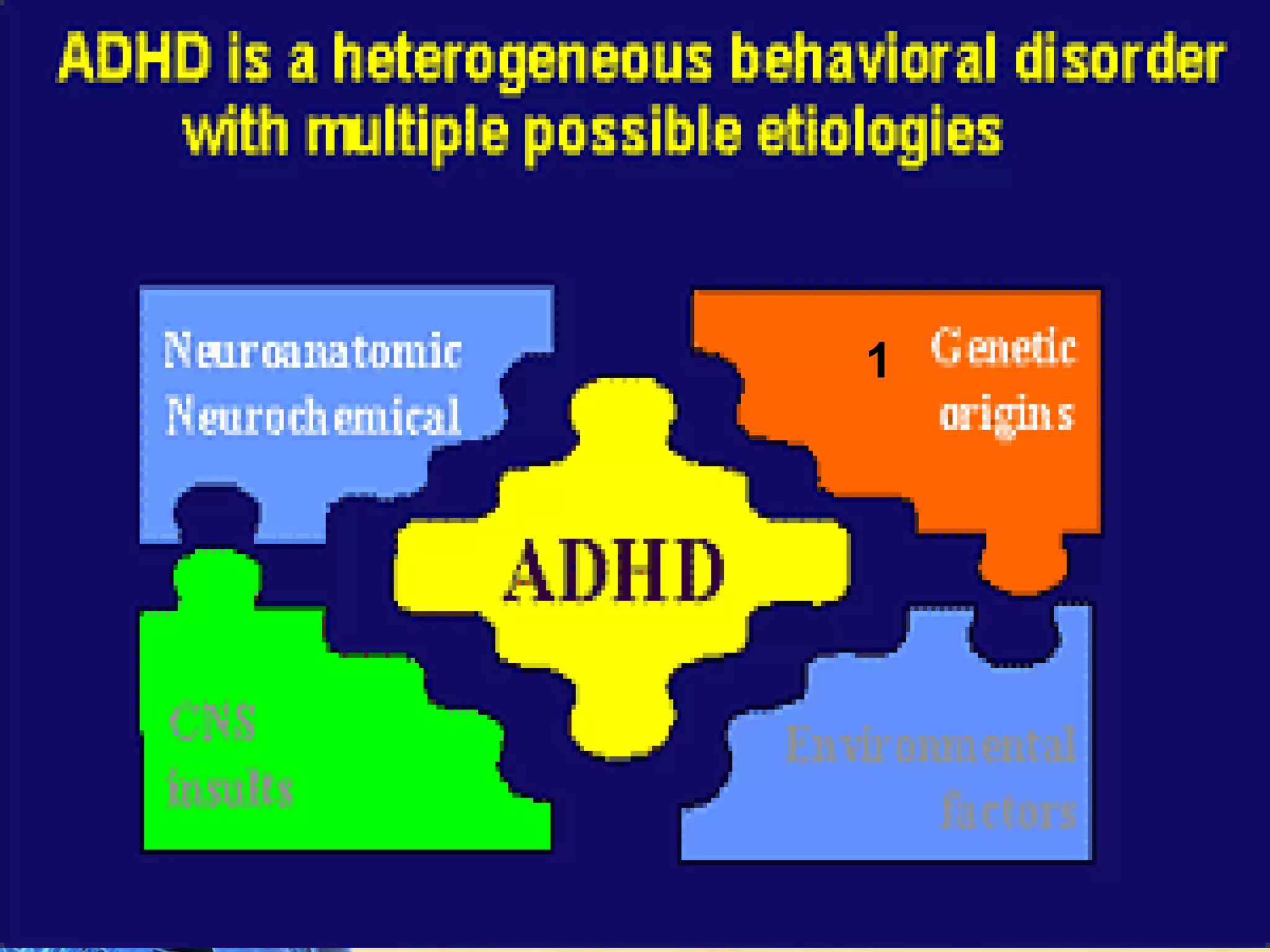
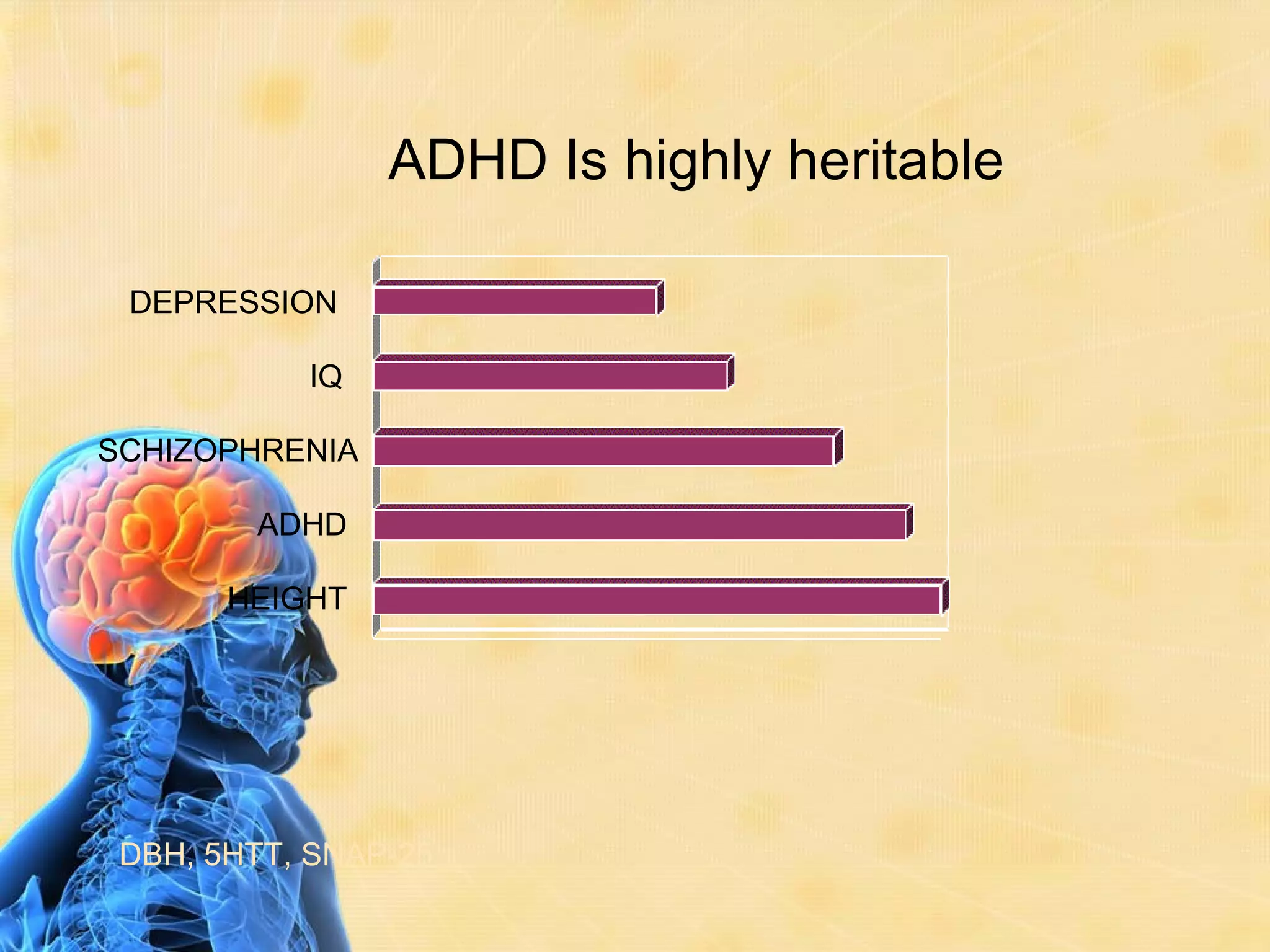
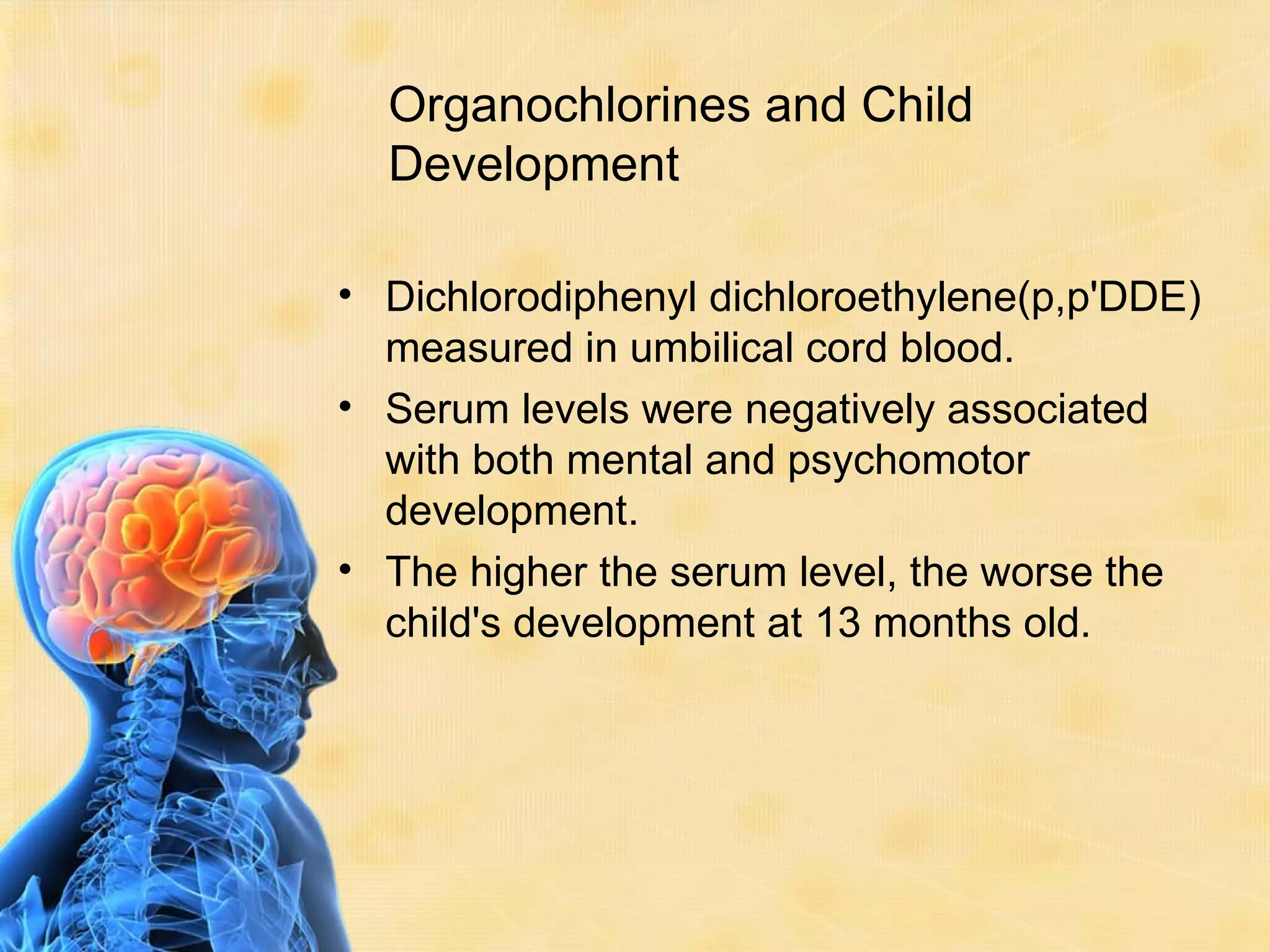
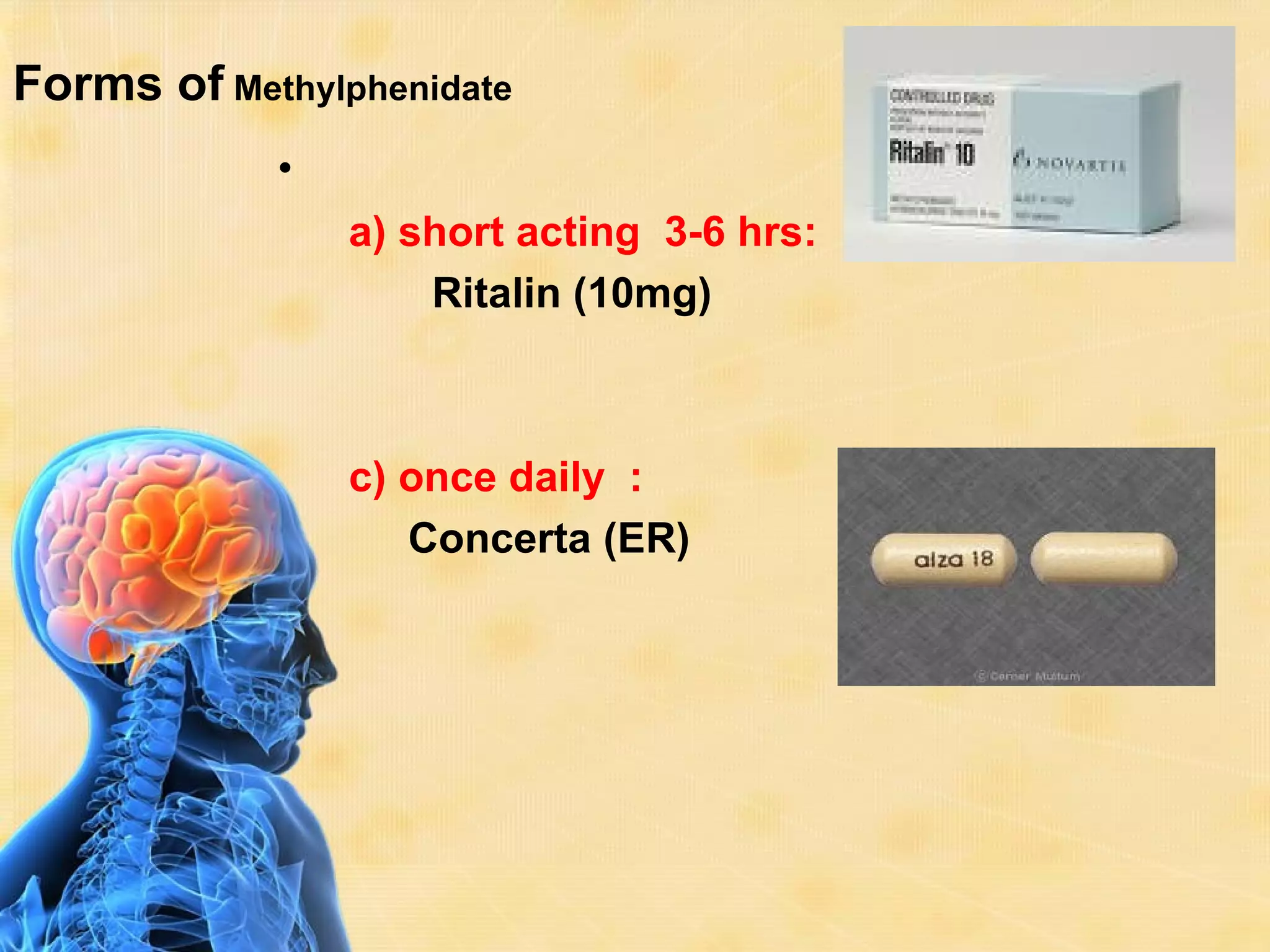
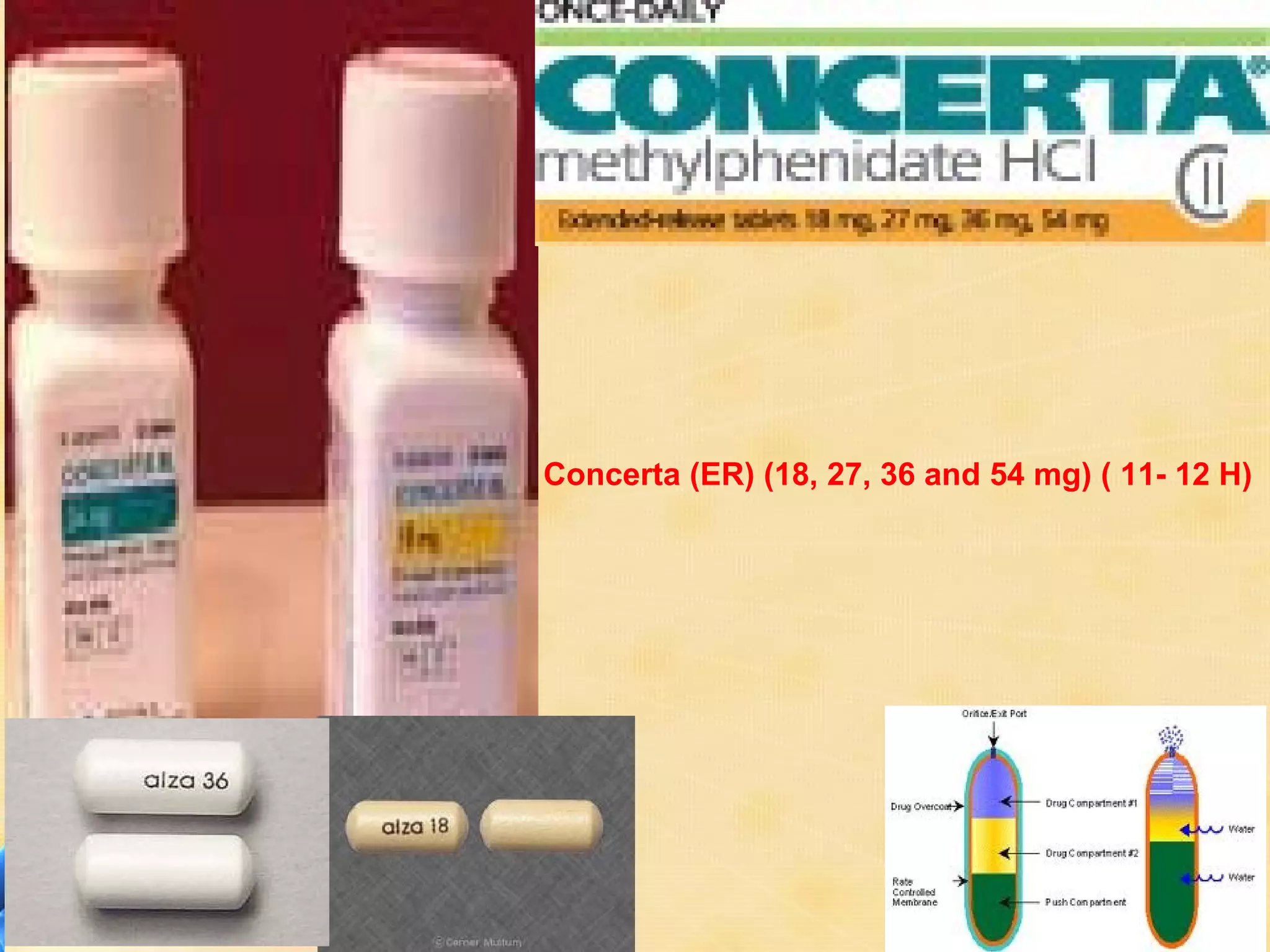
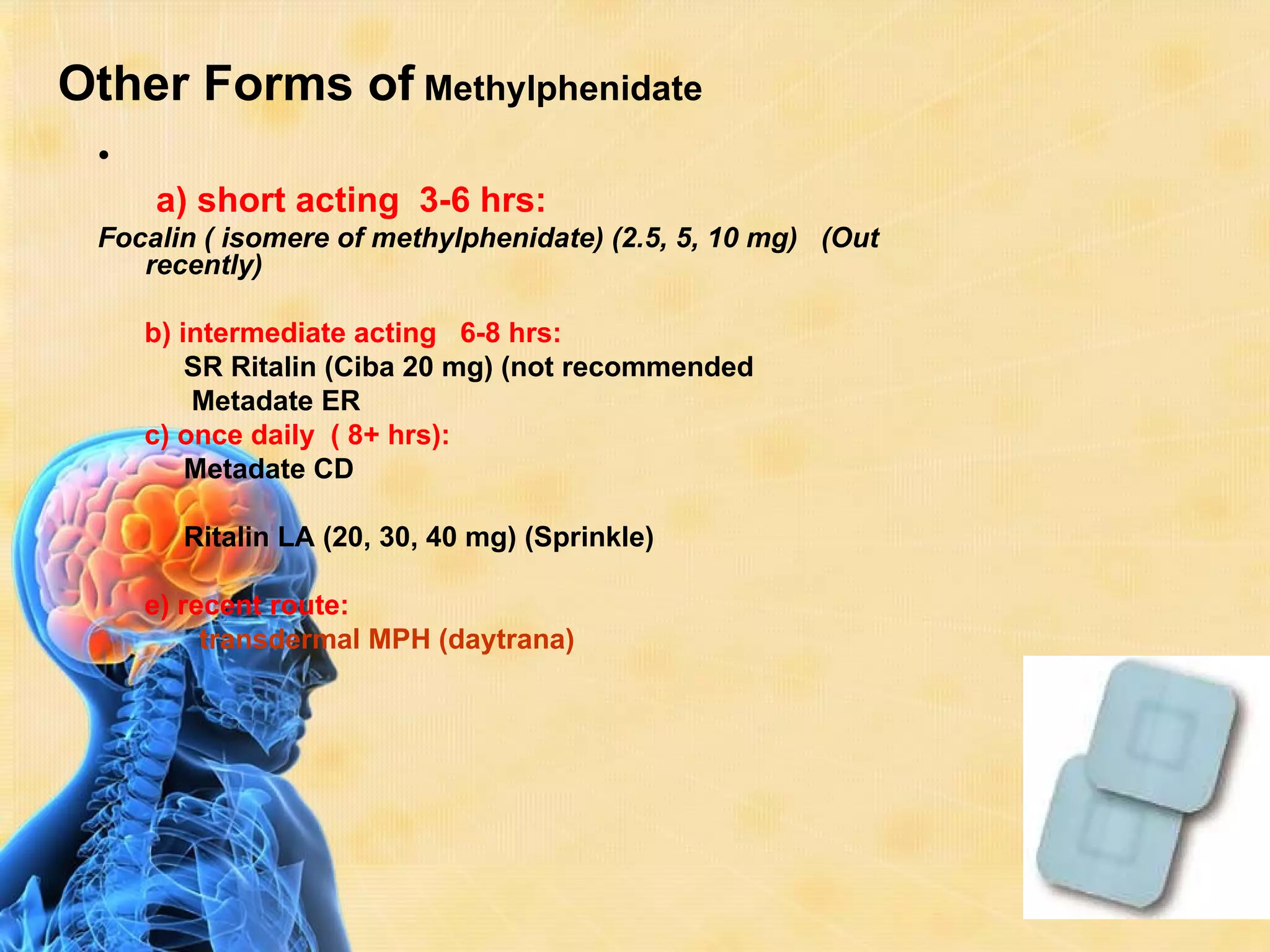
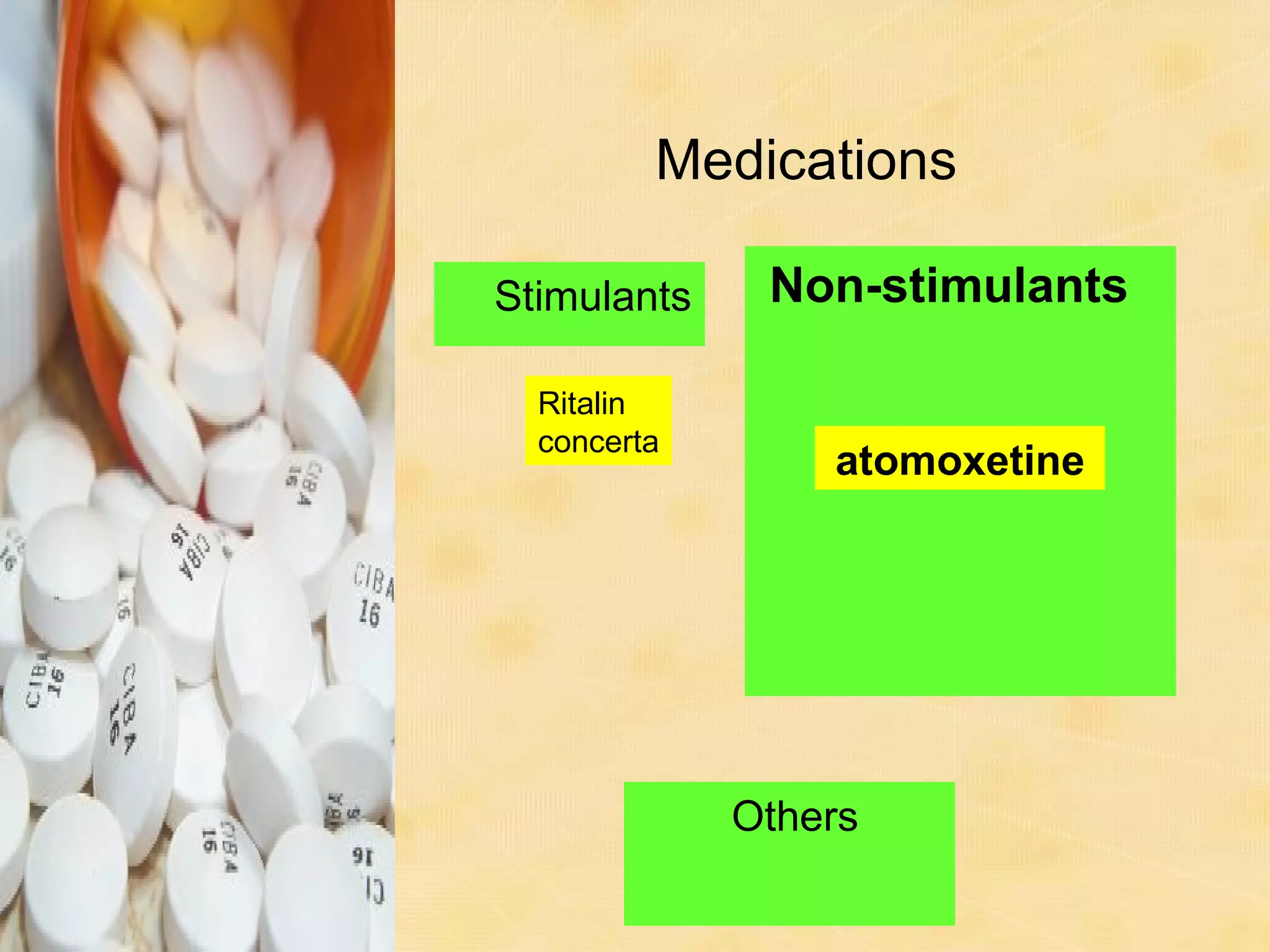
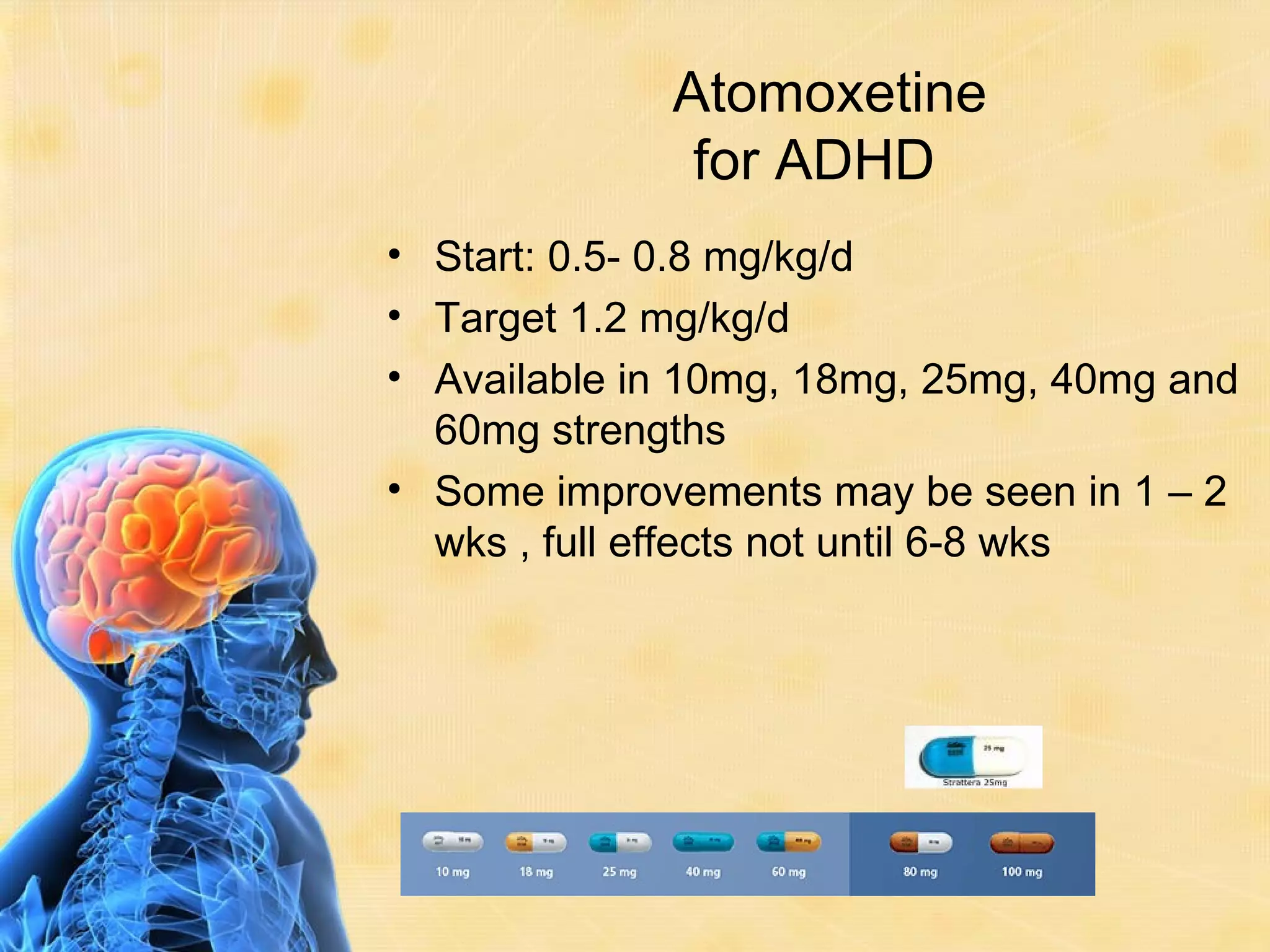
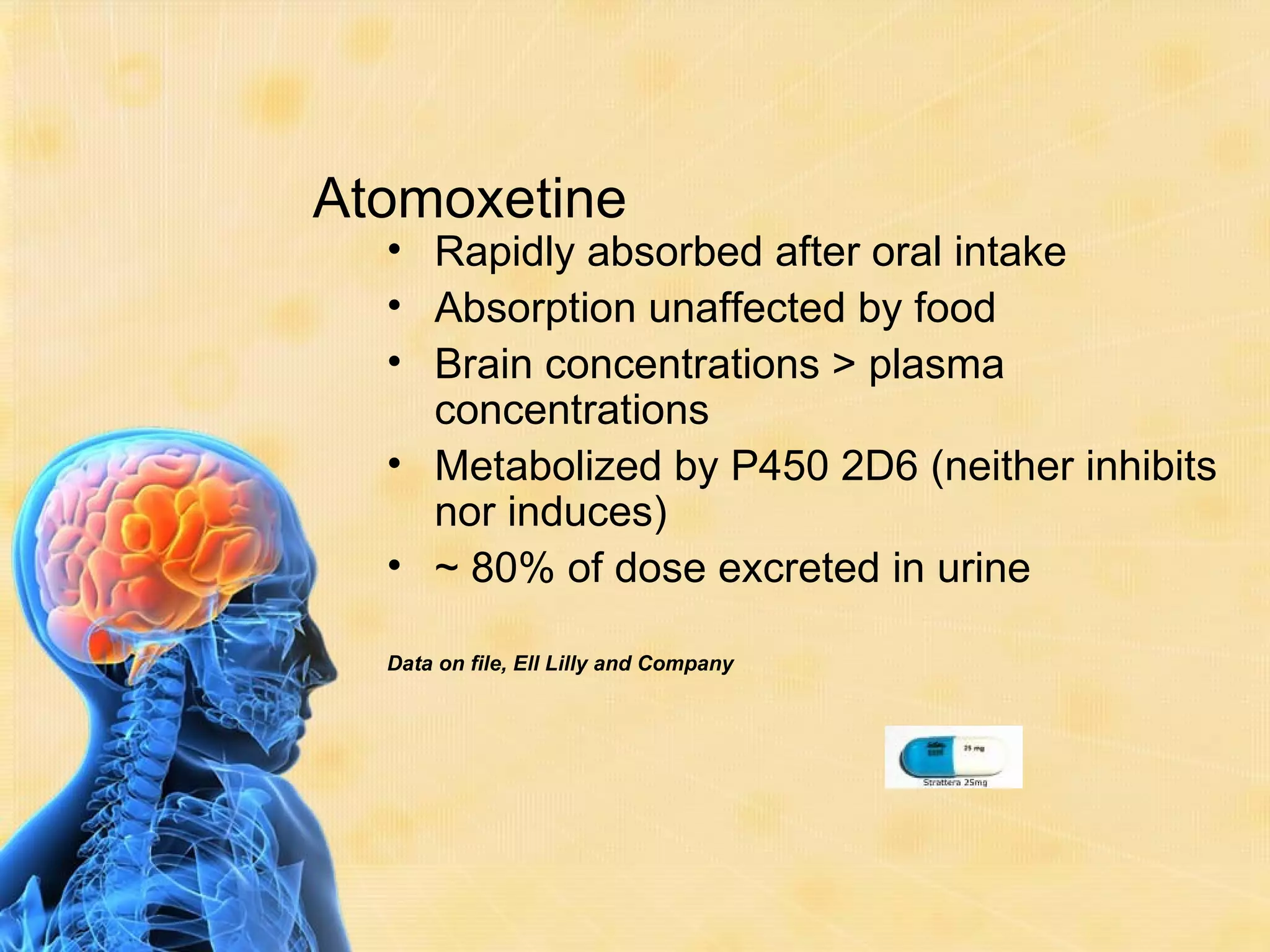
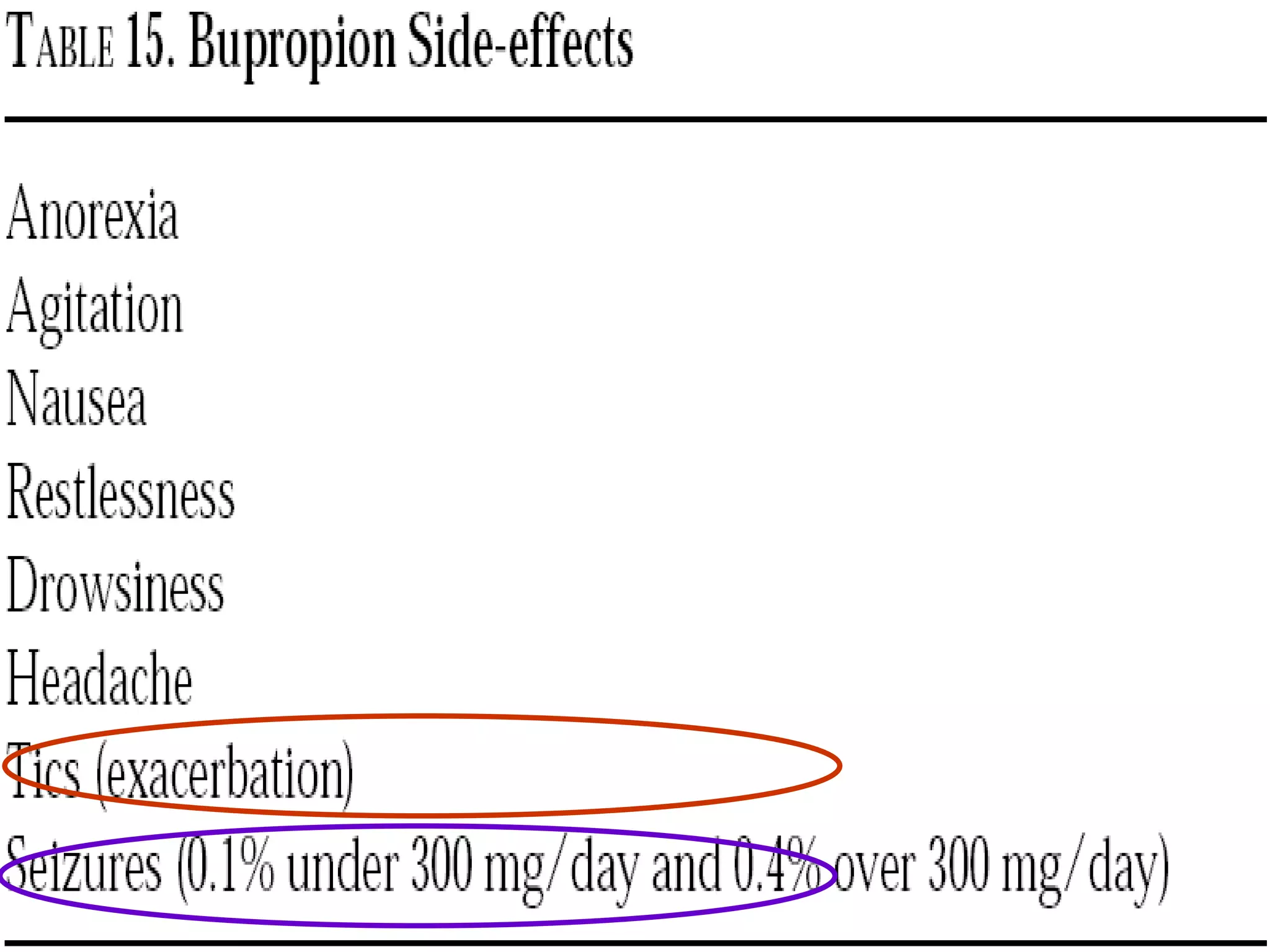
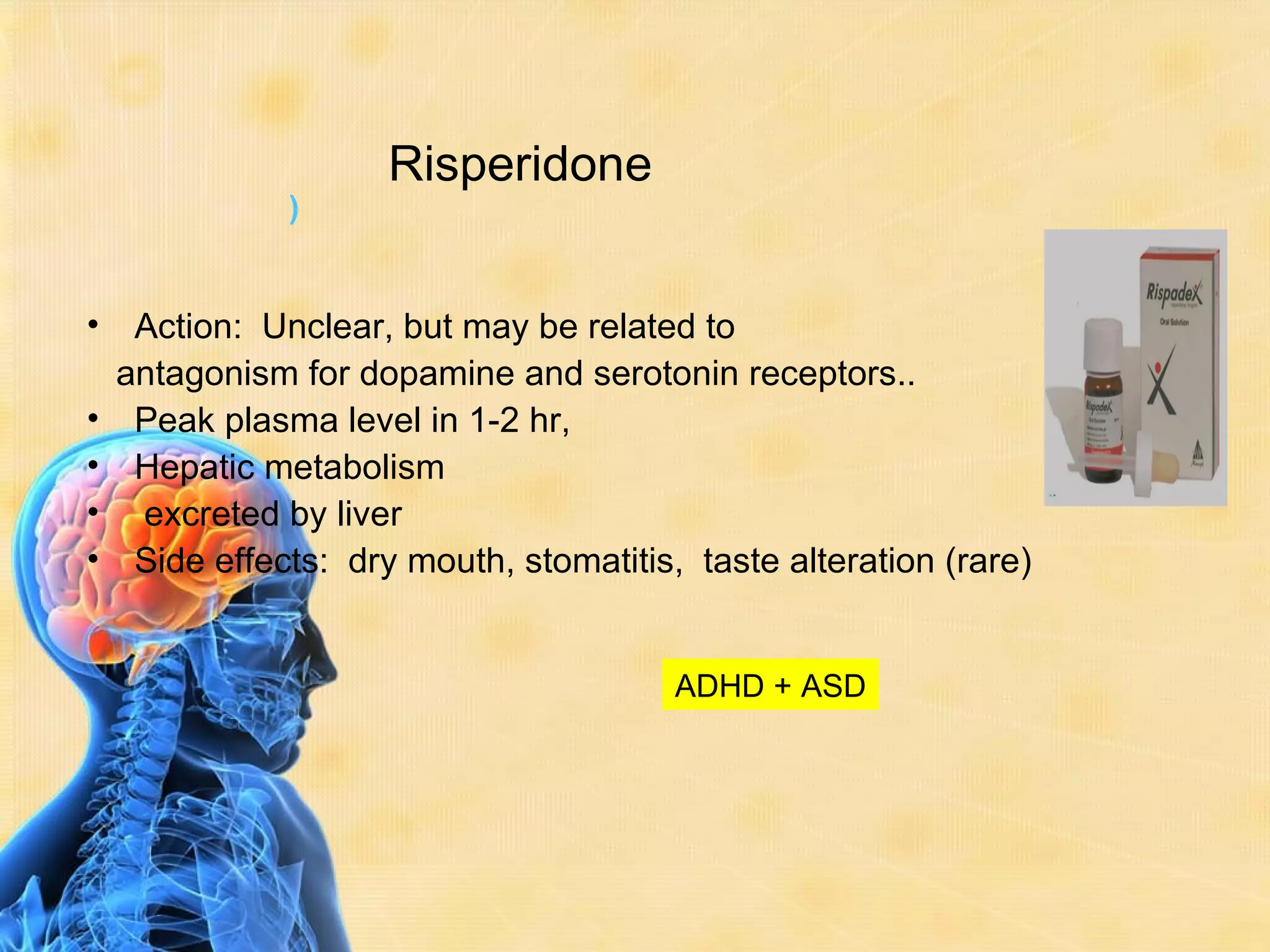
This document discusses guidelines for ADHD. It provides a brief history of how ADHD has been conceptualized over time, from defects in moral character to its current classification in the DSM-5 as a neurodevelopmental disorder. The document also discusses prevalence rates, symptoms, diagnosis, comorbidities, pathogenesis involving dopamine and norepinephrine systems, and multimodal treatment approaches including medication, behavioral modifications, and family counseling.