1. The kidneys perform several important functions including regulating fluid balance, electrolyte and acid-base homeostasis, and producing hormones like renin and erythropoietin.
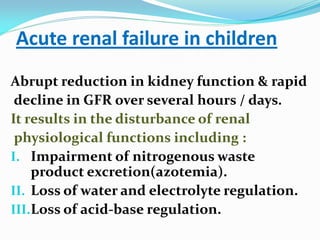
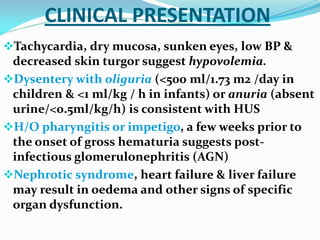
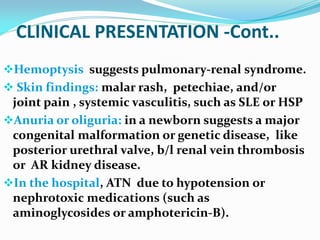
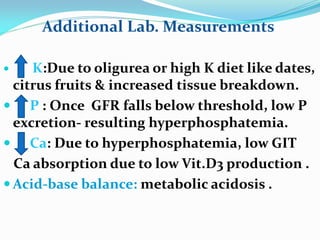
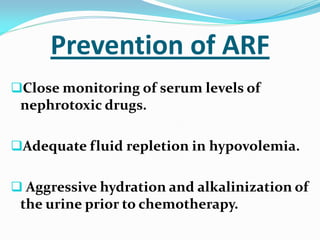
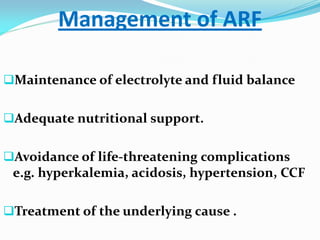
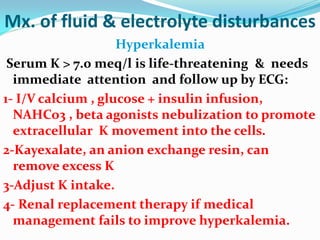
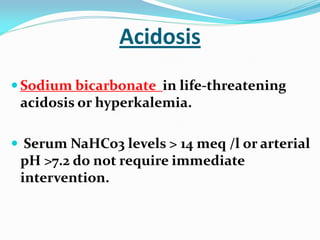
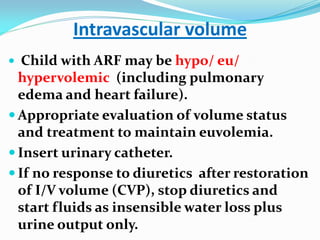
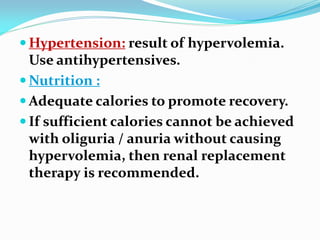
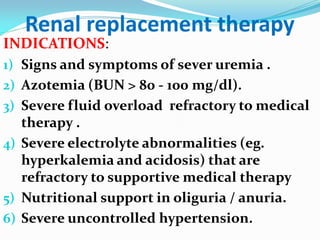
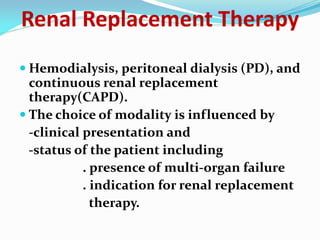
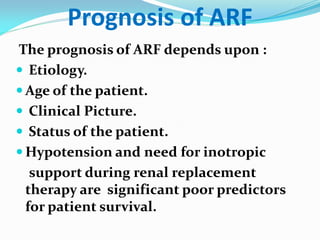
2. Acute renal failure in children results in impaired waste excretion, water and electrolyte dysregulation, and loss of acid-base control over hours to days.
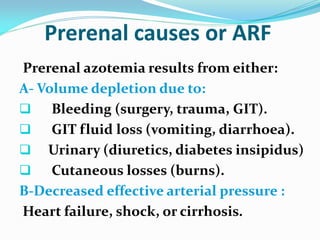
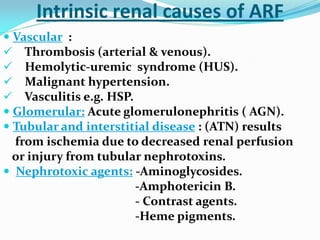
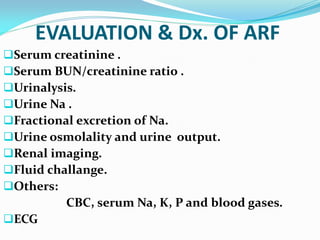
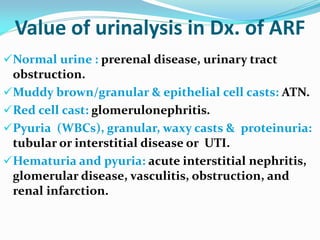
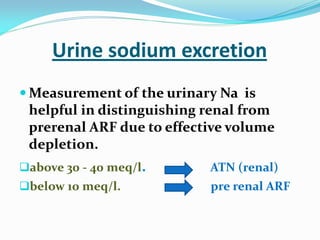
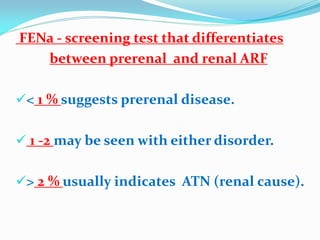
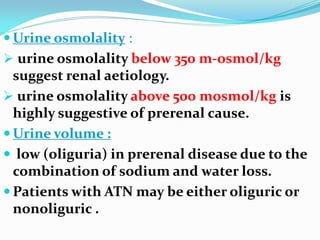
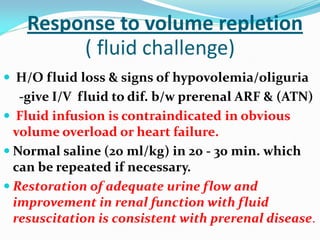
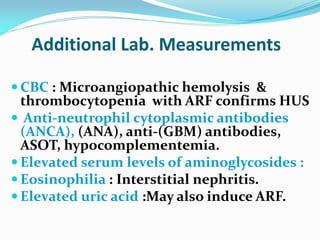
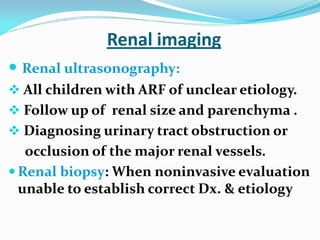
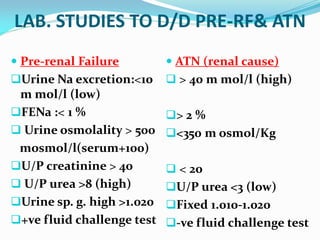
3. Causes include prerenal issues like dehydration, decreased blood pressure, or intrinsic renal problems such as glomerulonephritis, tubular injury, or nephrotoxins; evaluation involves lab tests, imaging, and assessing response to fluid resuscitation.