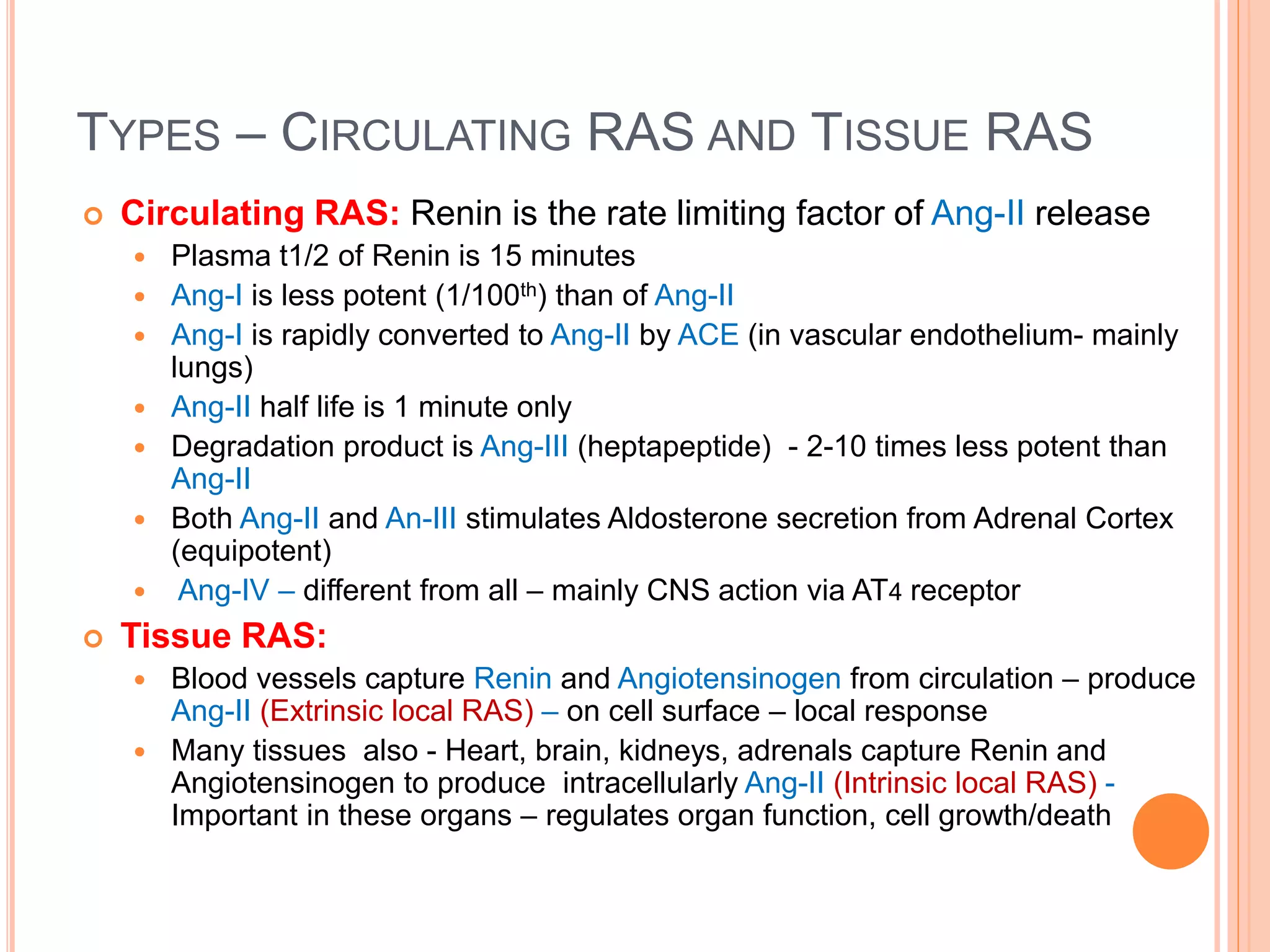
The document discusses the renin-angiotensin system (RAS) and drugs that affect it. RAS regulates blood pressure and electrolyte balance through the actions of angiotensin II, which is produced from renin and angiotensin converting enzyme. Angiotensin II causes vasoconstriction, sodium retention, and other effects. Drugs like ACE inhibitors and angiotensin receptor blockers inhibit parts of the RAS pathway to lower blood pressure. Captopril is an ACE inhibitor that blocks the conversion of angiotensin I to angiotensin II, reducing vasoconstriction and sodium retention.