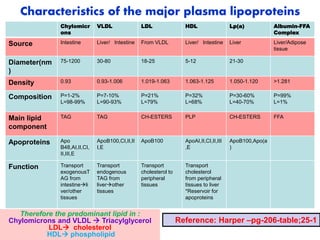
Lipoproteins are complexes of lipids and proteins that transport lipids through the bloodstream. There are four main types of plasma lipoproteins - chylomicrons, VLDL, LDL, and HDL - which differ in size, density, and lipid/protein composition. Chylomicrons carry dietary lipids from the intestine to other tissues, VLDL transports endogenous lipids from the liver, LDL carries cholesterol, and HDL transports cholesterol from tissues to the liver for processing or excretion. The metabolism and interactions between these lipoproteins, such as the transfer of lipids between them, are tightly regulated and essential for maintaining lipid homeostasis.














![Lipoprotein (a) [Lp(a) or Little ‘a’] – Deadly
Cholesterol
Structure: Lipoprotein (a) [Lp(a)] is structurally LDL-like particle synthesized
by the liver that along with apoB100 contain the very large glycoprotein
apolipoprotein (a) [apo(a)] that is covalently linked to apoB100 by disulfide
bonds.
Epidemiology: In 40% population, there is no detectable level of Lp(a) in
serum. In 20% of population, the Lp(a) concentration in blood is more than
30 mg/dL; and these persons are susceptible for heart attack at a younger
age.
Clinical significance: Lp(a) is associated with heart attacks at the age of 30
or 40 years. Indians have a higher level of Lp(a) than Western populations –
Deadly Cholesterol.
Dietary trans-fatty acids from high temperature fast-processed food
increase the level of Lp(a).
Lp(a) levels increase in patients with diabetic nephropathy. Estrogen
decreases both LDL and Lp(a) levels.](https://image.slidesharecdn.com/8-lipoproteinmetabolism-220919233423-b291b286/85/8-LIPOPROTEIN-METABOLISM-ppt-19-320.jpg)
![Lipoprotein (a) [Lp(a) or Little ‘a’] –
Deadly Cholesterol…. cont
Mechanism of action:
Lp(a) competitively inhibits plasminogen
activation into plasmin, and fibrinolysis
by competing with plasminogen
activators. This predisposes to embolism,
thrombosis and increased risk of
coronary heart disease.
Lp(a) also binds to macrophages via a
high-affinity receptor at sites of vascular
injury that promotes foam cell
formation and the deposition of
cholesterol in atherosclerotic plaques
causing a high risk of premature
coronary artery disease and stroke.
Nicotinic acid reduces serum
Lp(a) level.](https://image.slidesharecdn.com/8-lipoproteinmetabolism-220919233423-b291b286/85/8-LIPOPROTEIN-METABOLISM-ppt-20-320.jpg)
