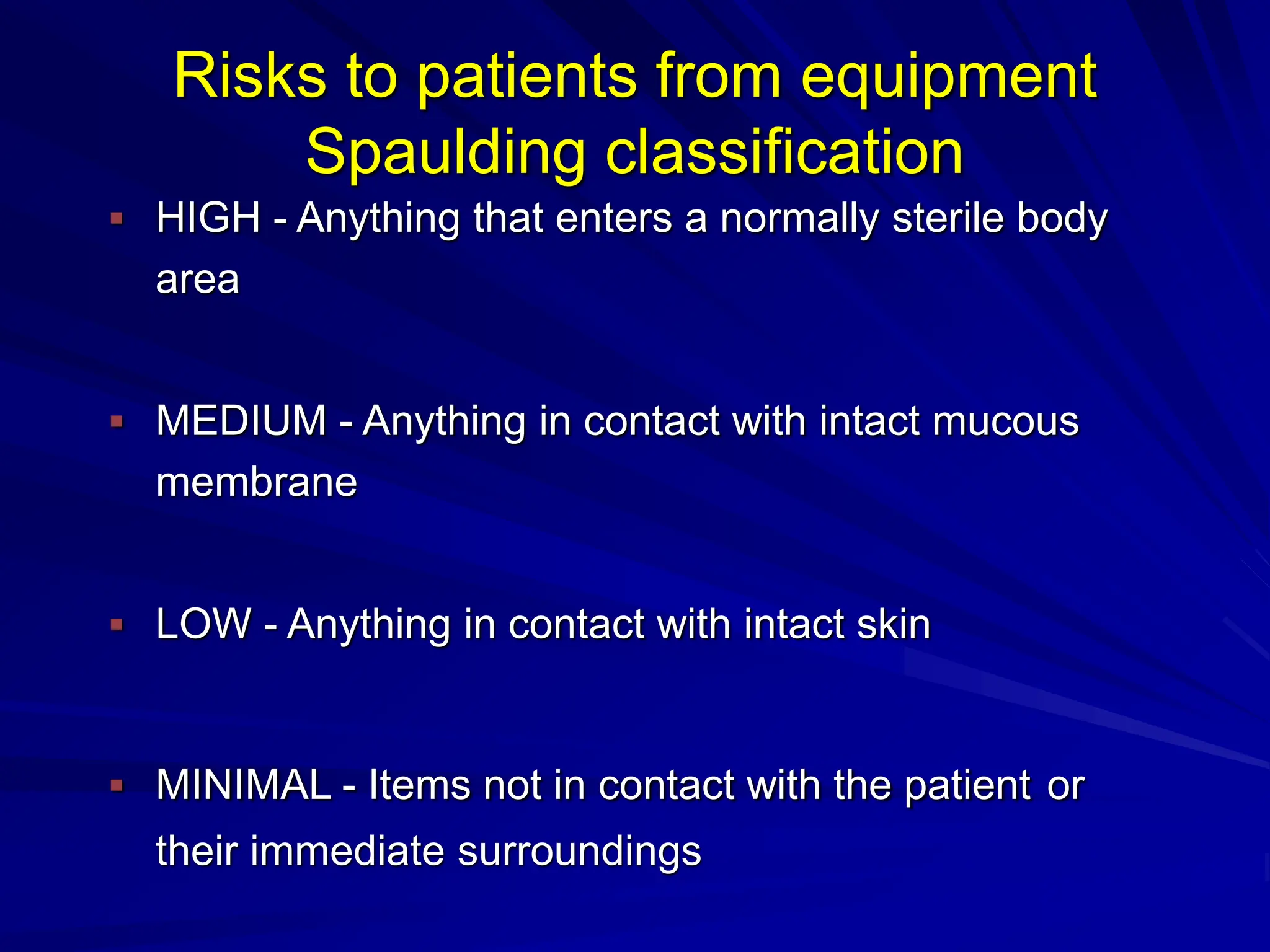
The document outlines the principles of standard precautions in healthcare to ensure the safety of patients and healthcare workers, focusing on hand hygiene, personal protective equipment, instrument reprocessing, aseptic techniques, environmental cleaning, and waste management. Standard precautions are necessary for infection control applicable to all patients in any healthcare setting. It highlights effective cleaning practices and waste management strategies to mitigate infection risks and maintain a safe healthcare environment.