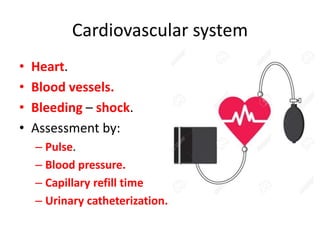
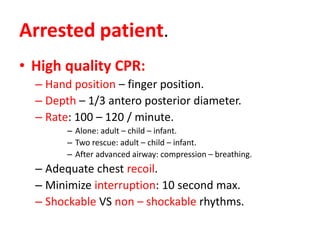
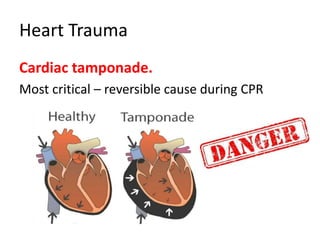
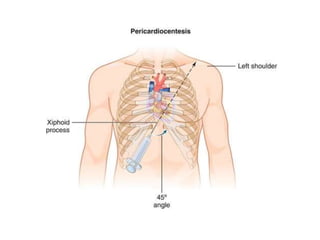
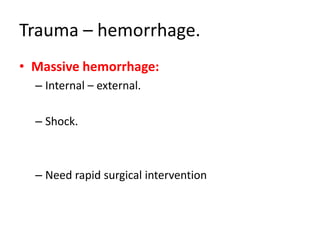
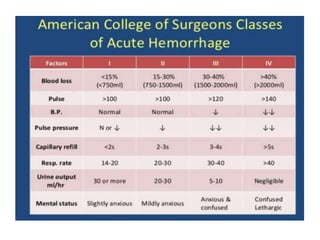
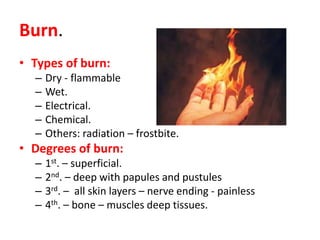
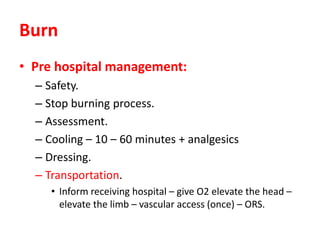
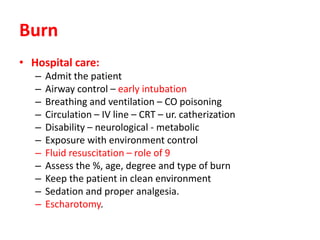
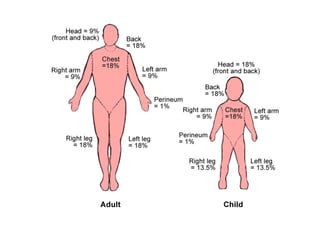
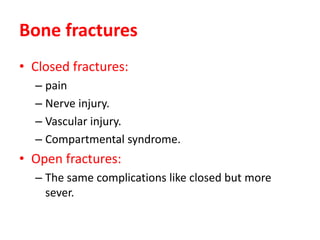
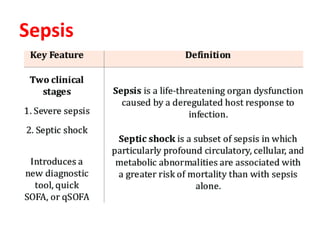
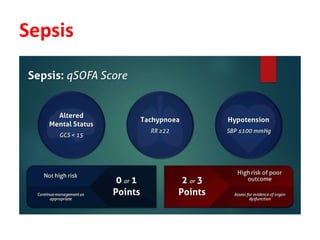
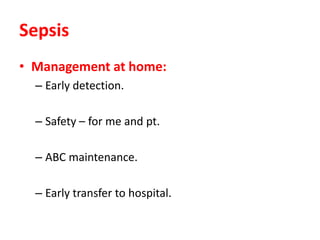
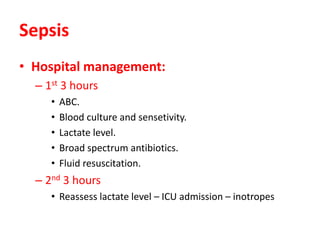
This document outlines emergency management protocols for various medical situations, including CPR techniques, trauma care for hemorrhage and burns, and management of sepsis. Key topics include high-quality CPR practices, assessment of circulation issues, types and degrees of burns, and the importance of early detection and intervention. It emphasizes the need for precise evaluation and timely transfer to hospitals to optimize patient outcomes.