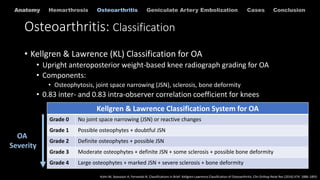
This document discusses geniculate artery embolization (GAE) for the treatment of knee hemarthrosis and osteoarthritis. GAE involves selectively embolizing the geniculate arteries that supply blood to the hypervascular synovium in the knee. This reduces synovial blood flow and angiogenesis, decreasing inflammation and pain. The technique involves accessing the femoral artery and selectively catheterizing the geniculate arteries under fluoroscopy. Particles or coils are then used for embolization. Studies have found GAE to be an effective minimally invasive treatment option for recurrent hemarthrosis and symptomatic osteoarthritis.