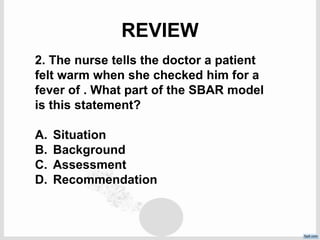
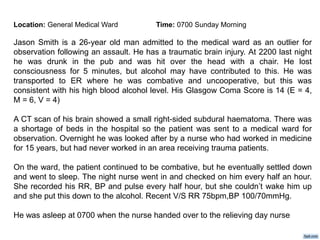
The patient is a 26-year-old man admitted to the medical ward for observation following a traumatic brain injury from being hit in the head with a chair at a pub. A CT scan showed a small right-sided subdural hematoma. Overnight the patient was combative but settled down and slept. The night nurse checked his vitals every 30 minutes but could not wake him. His most recent vitals showed a respiratory rate of 75, blood pressure of 100/70. He remained asleep at the start of the day shift.