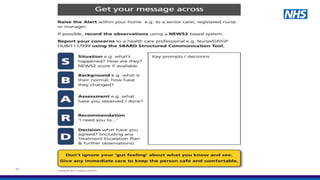
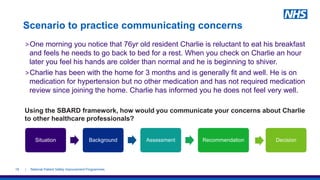
This document provides an overview of a training session on recognizing early signs of patient deterioration and effectively communicating concerns. The objectives are to ensure care staff can quickly identify any illness or cause of deterioration, appropriately respond and escalate concerns using a structured communication method (SBARD), and get the right help. Soft signs that may indicate a patient is unwell and examples are discussed. The ReSPECT process for documenting emergency treatment preferences is also reviewed.