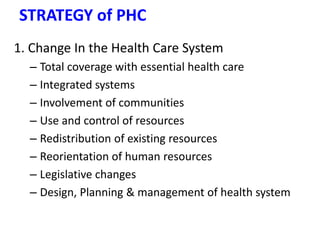
This document provides an overview of primary health care (PHC), including its definition, historical development, principles, strategies, and implementation in Ethiopia. The key points are:
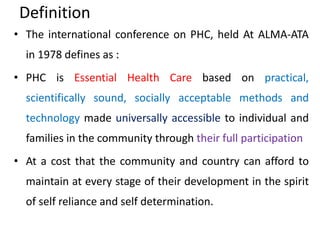
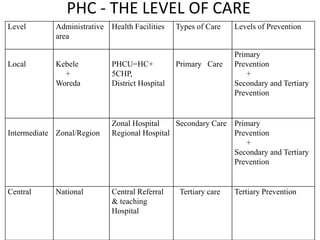
- PHC aims to provide essential health care universally and affordably through community participation. It forms the first level of contact with the health system and emphasizes prevention.
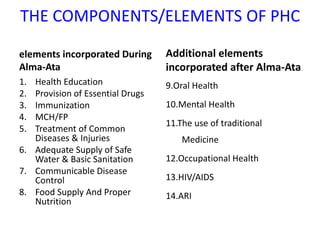
- Approaches to PHC evolved from disease-focused vertical programs in the 1950s-70s to the comprehensive PHC model endorsed at Alma-Ata in 1978, focusing on health promotion, prevention and inter-sectoral collaboration.
- Ethiopia adopted PHC in the 1980s but faced challenges with implementation including lack of infrastructure, resources and inter-