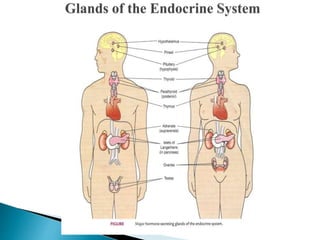
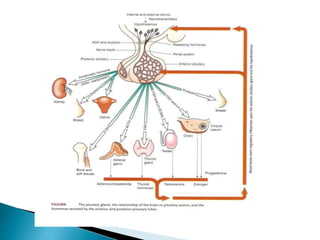
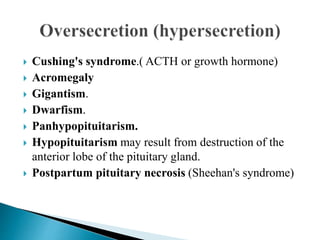
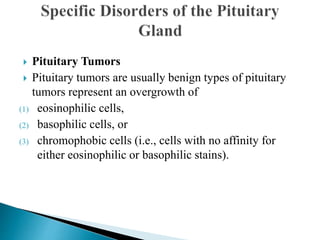
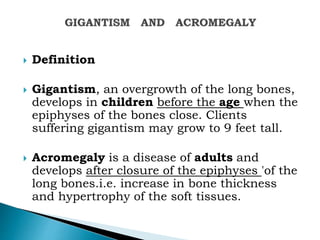
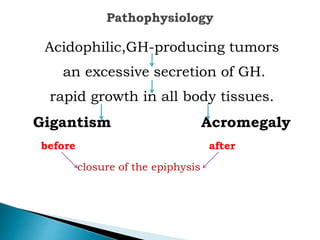
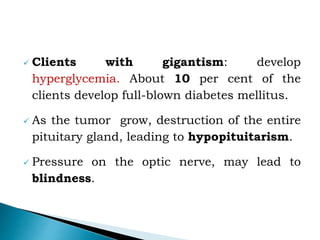
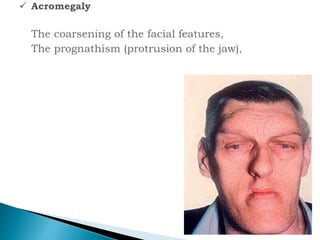
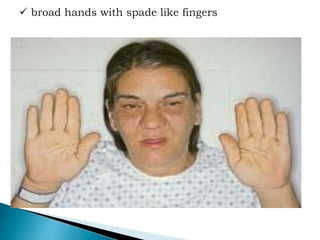
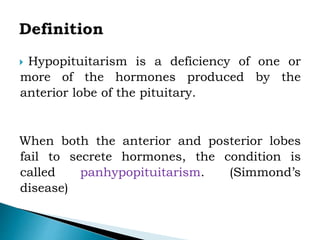
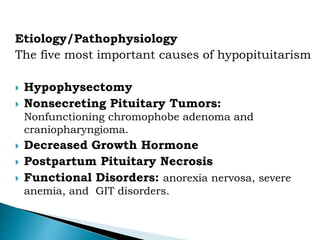
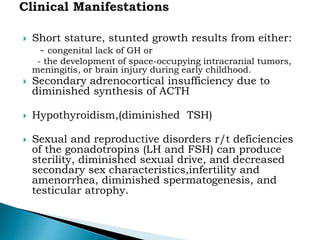
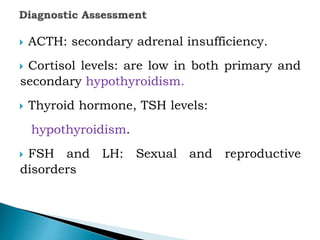
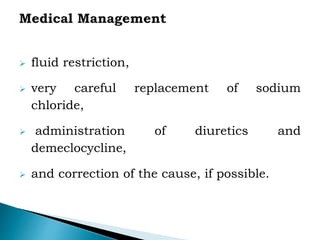
The document discusses the endocrine system and various endocrine disorders. It provides an overview of the pituitary gland and hormones it secretes including ACTH, TSH, growth hormone, and others. Specific endocrine disorders covered include Cushing's syndrome, acromegaly, gigantism, hypopituitarism, diabetes insipidus, and syndrome of inappropriate antidiuretic hormone secretion. Treatment options are discussed for each condition along with nursing considerations.