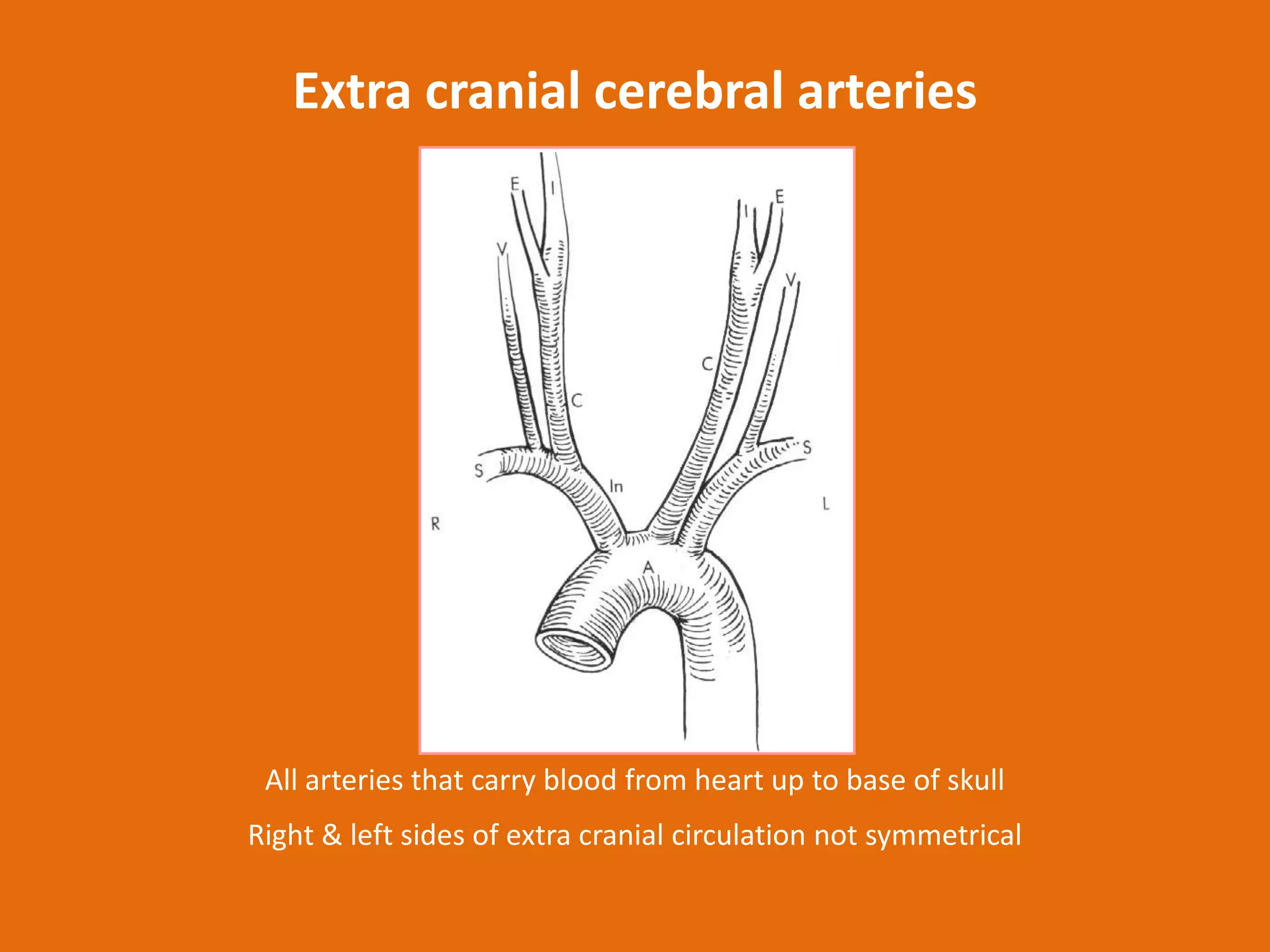
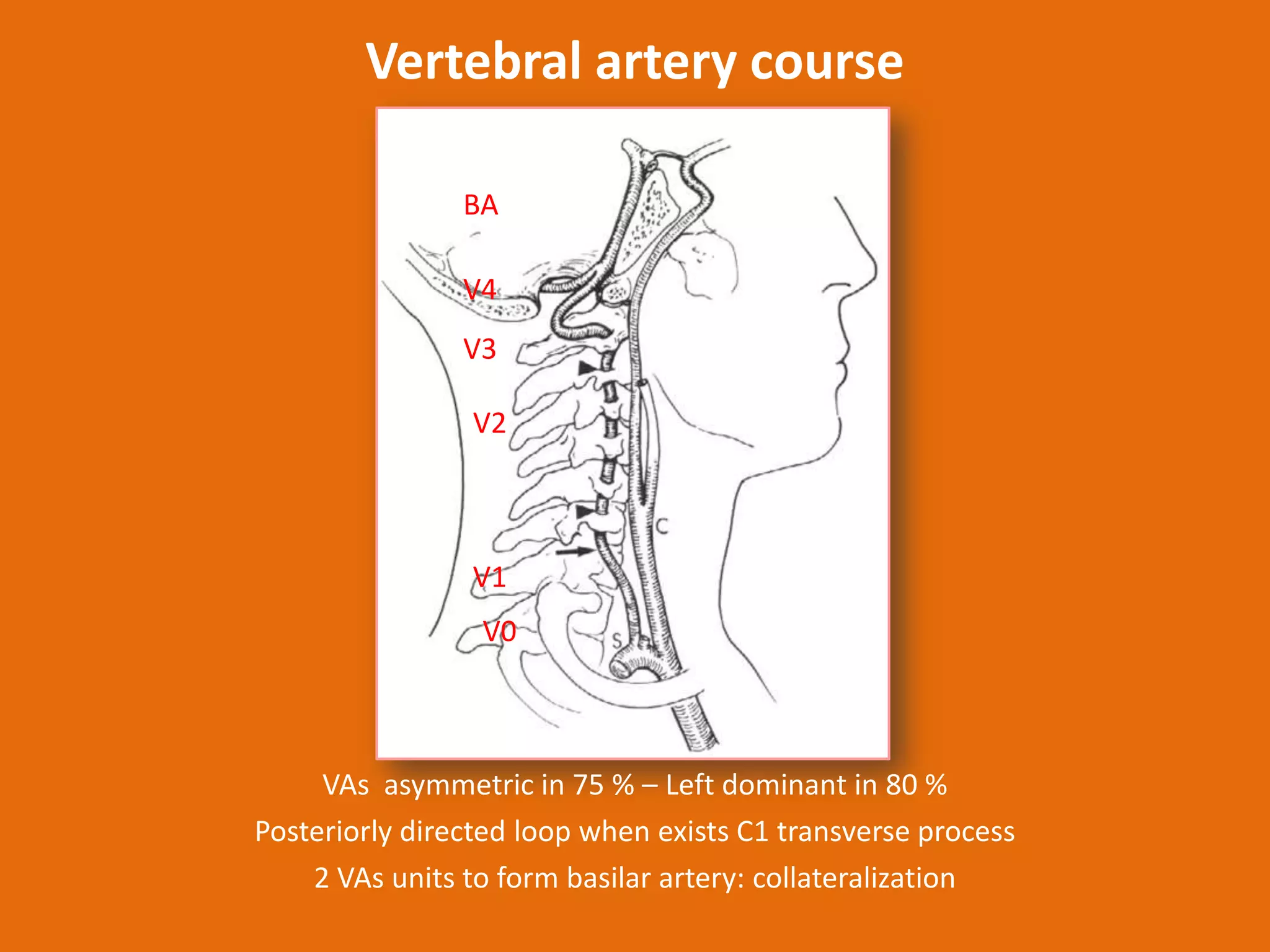
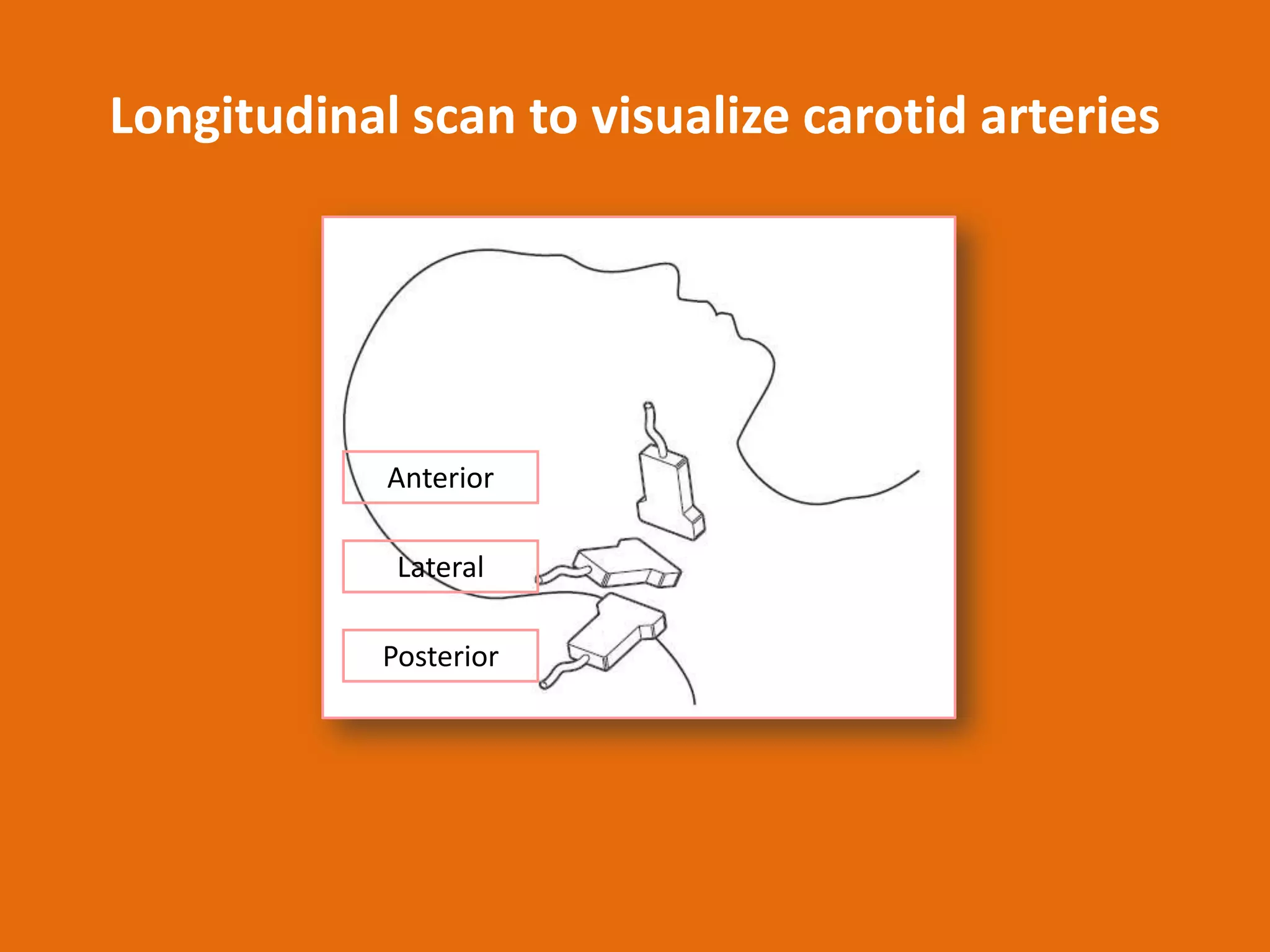
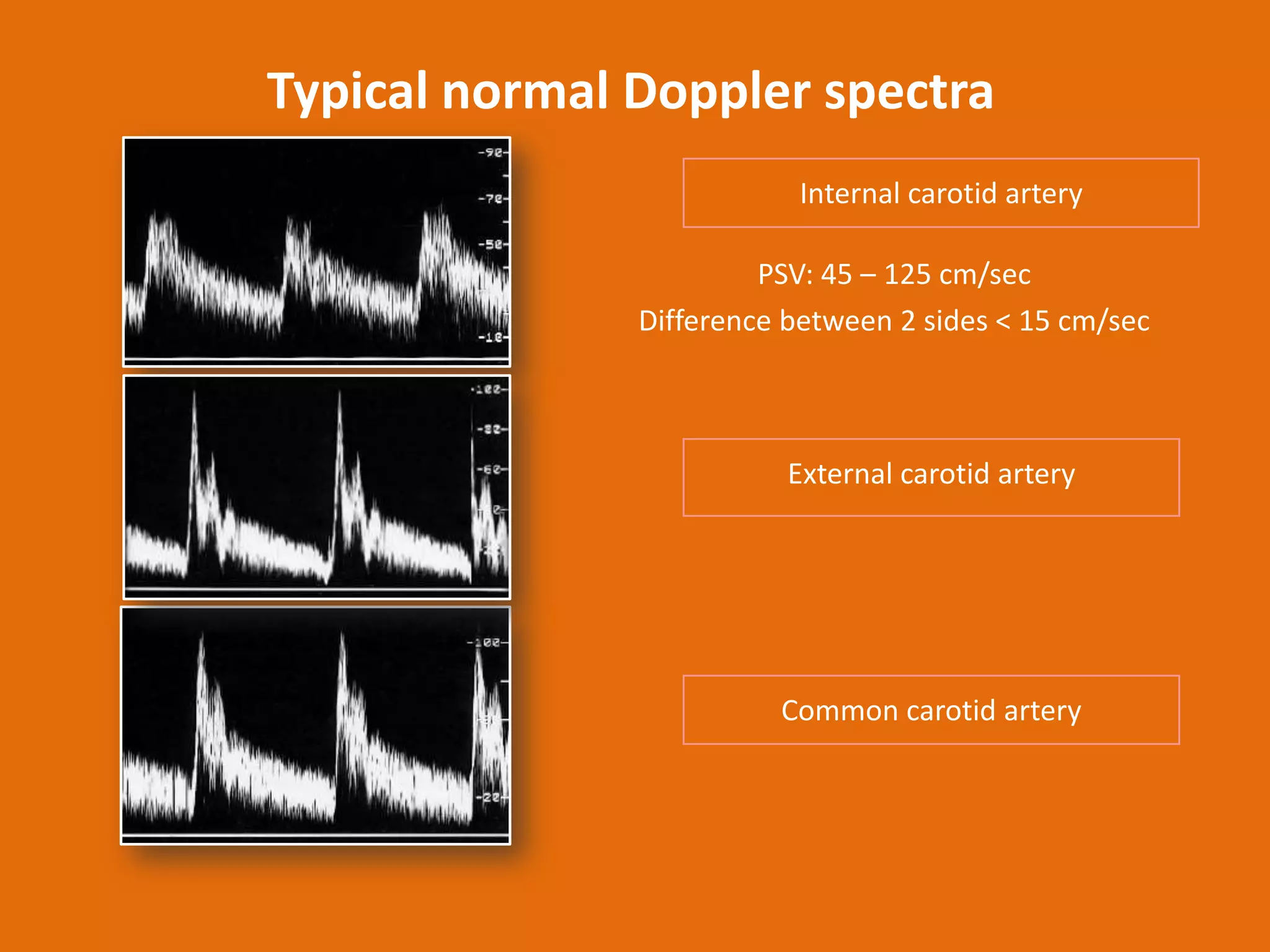
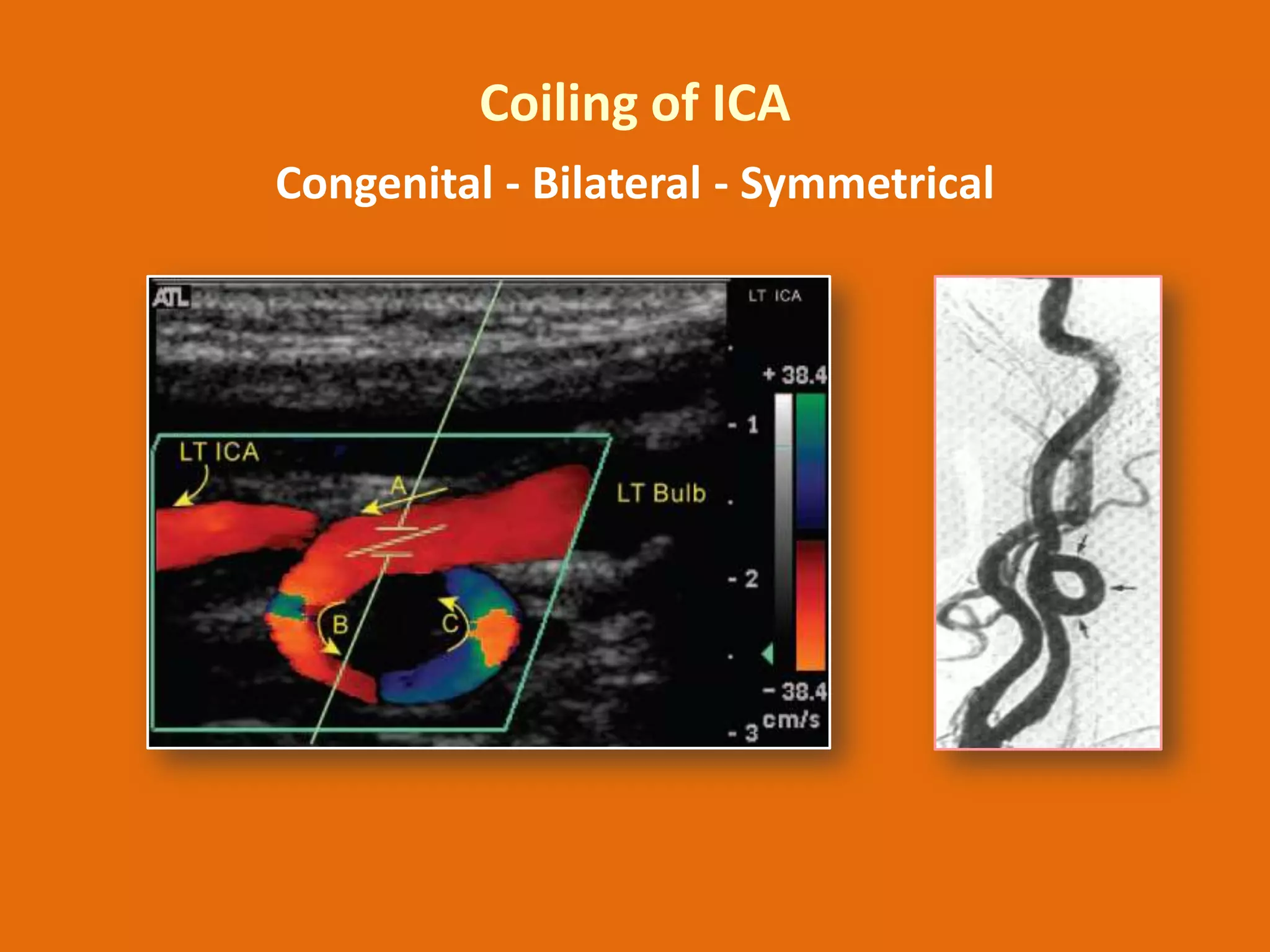
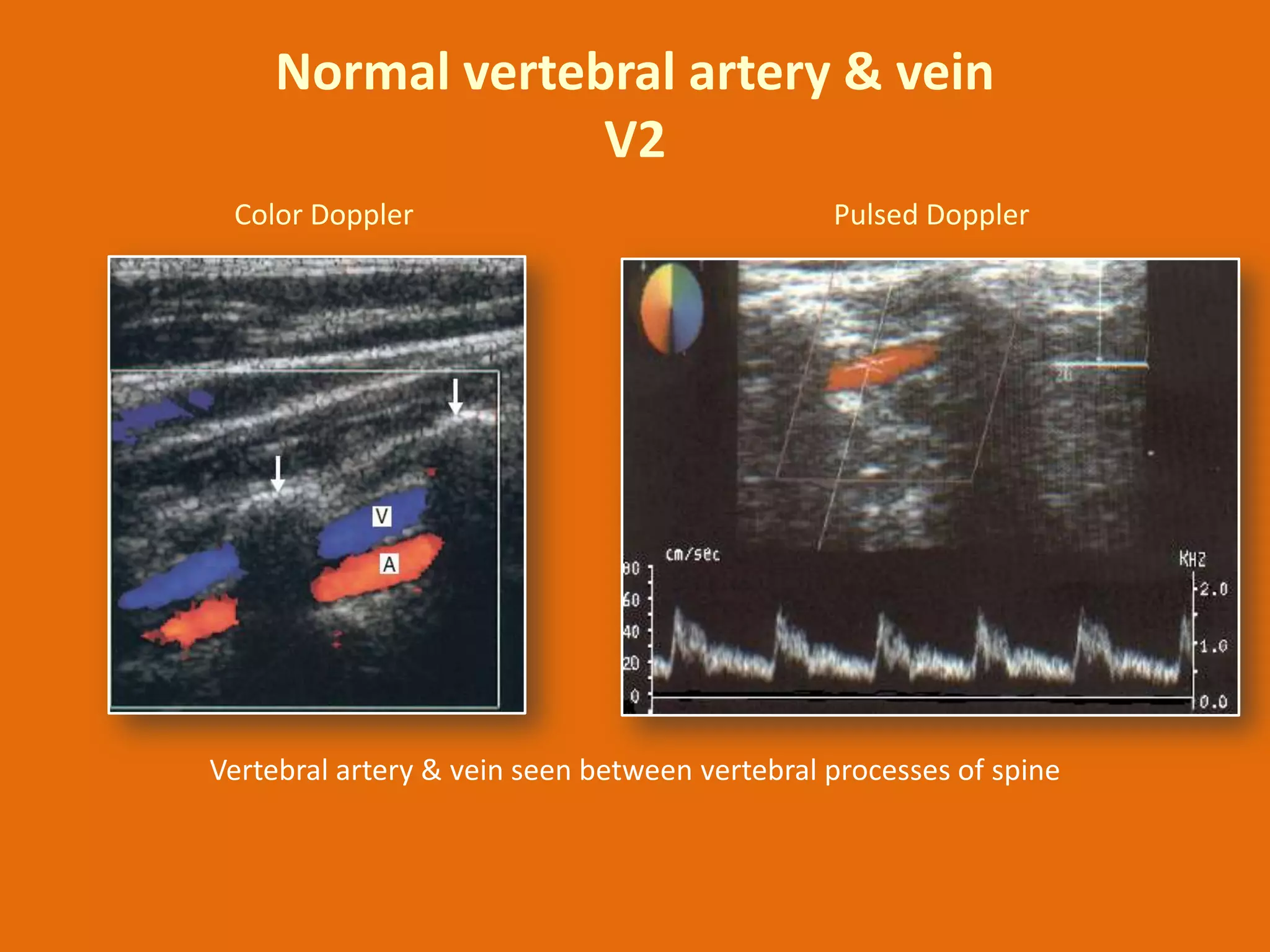
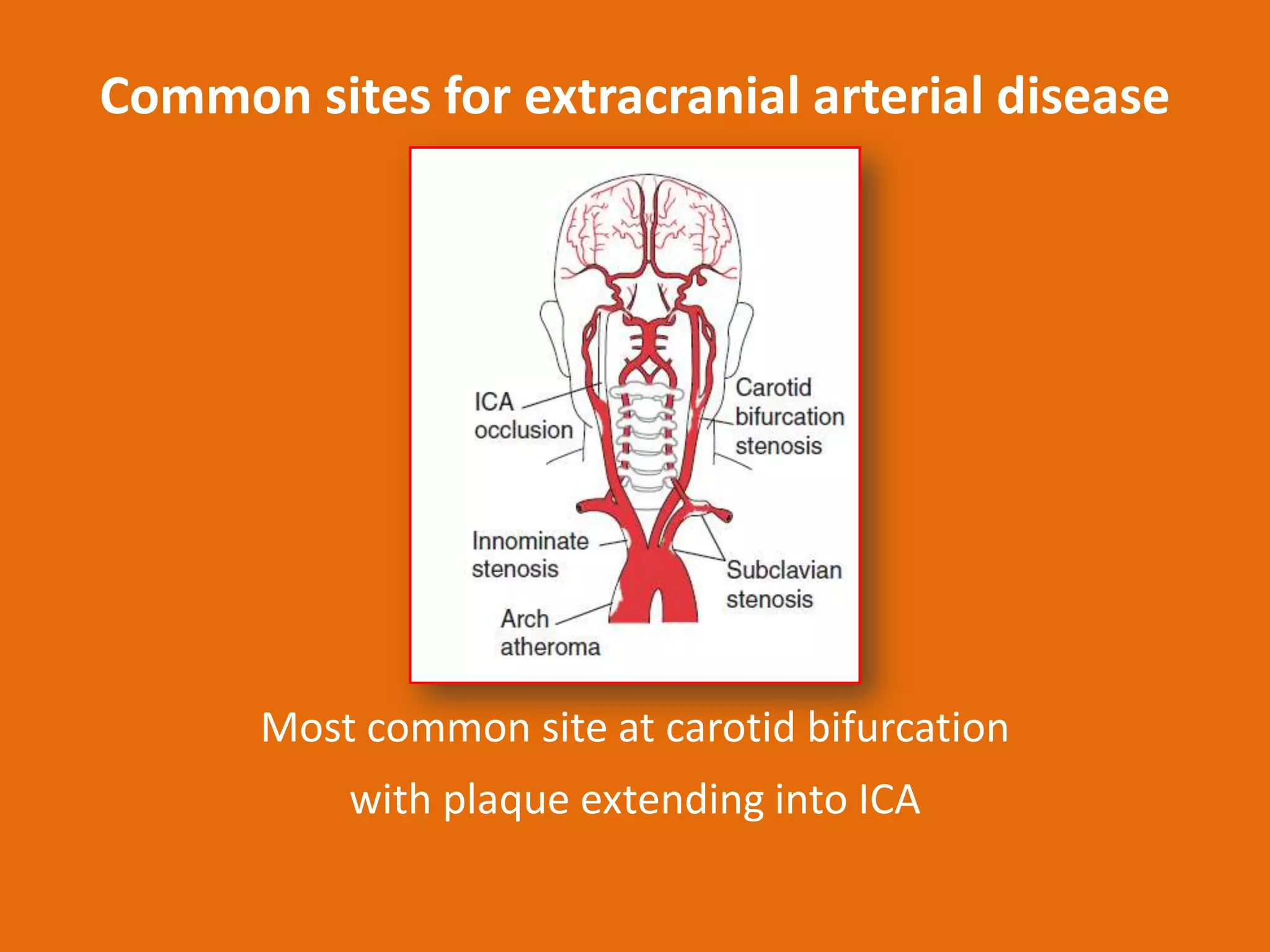
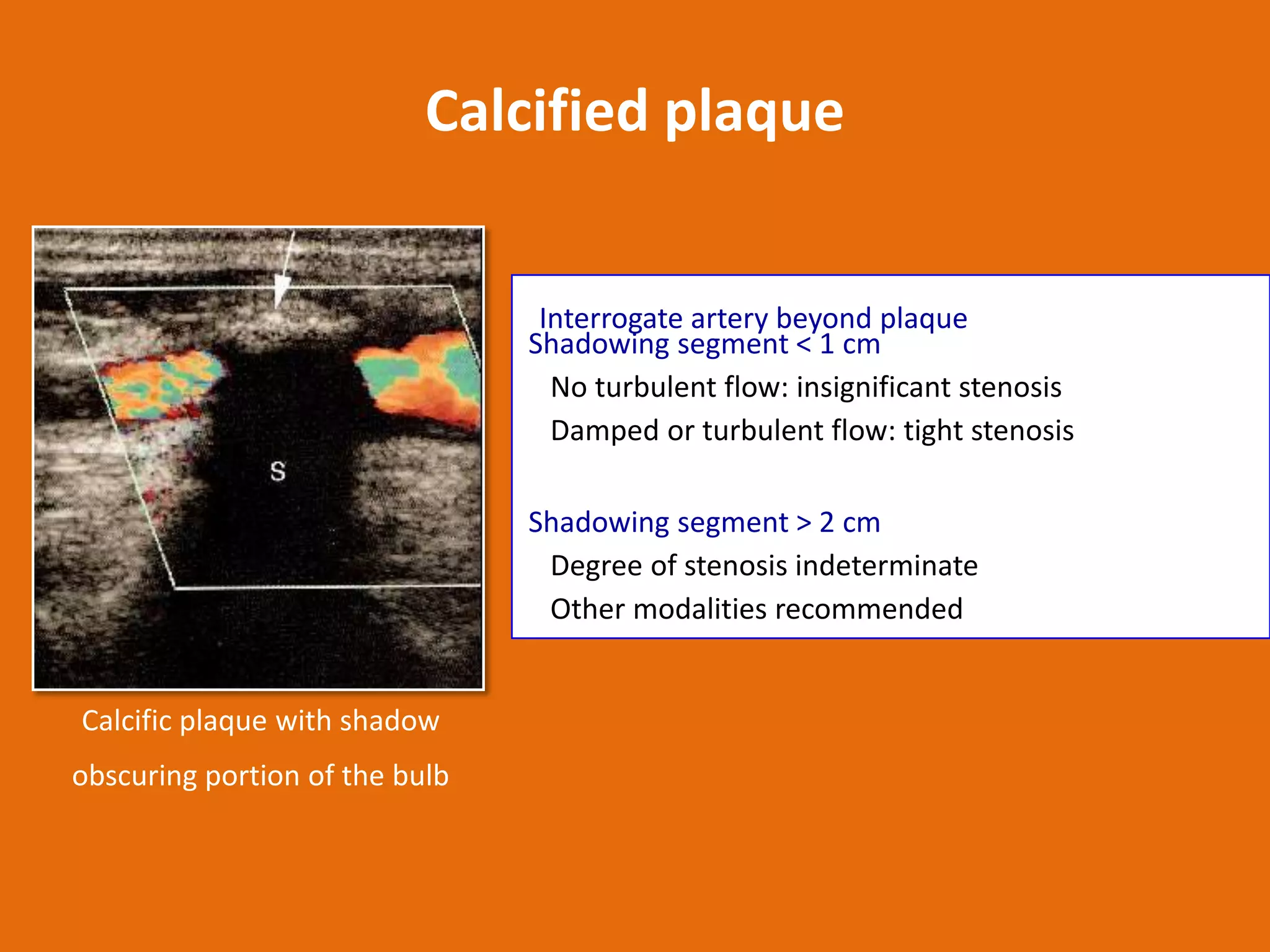
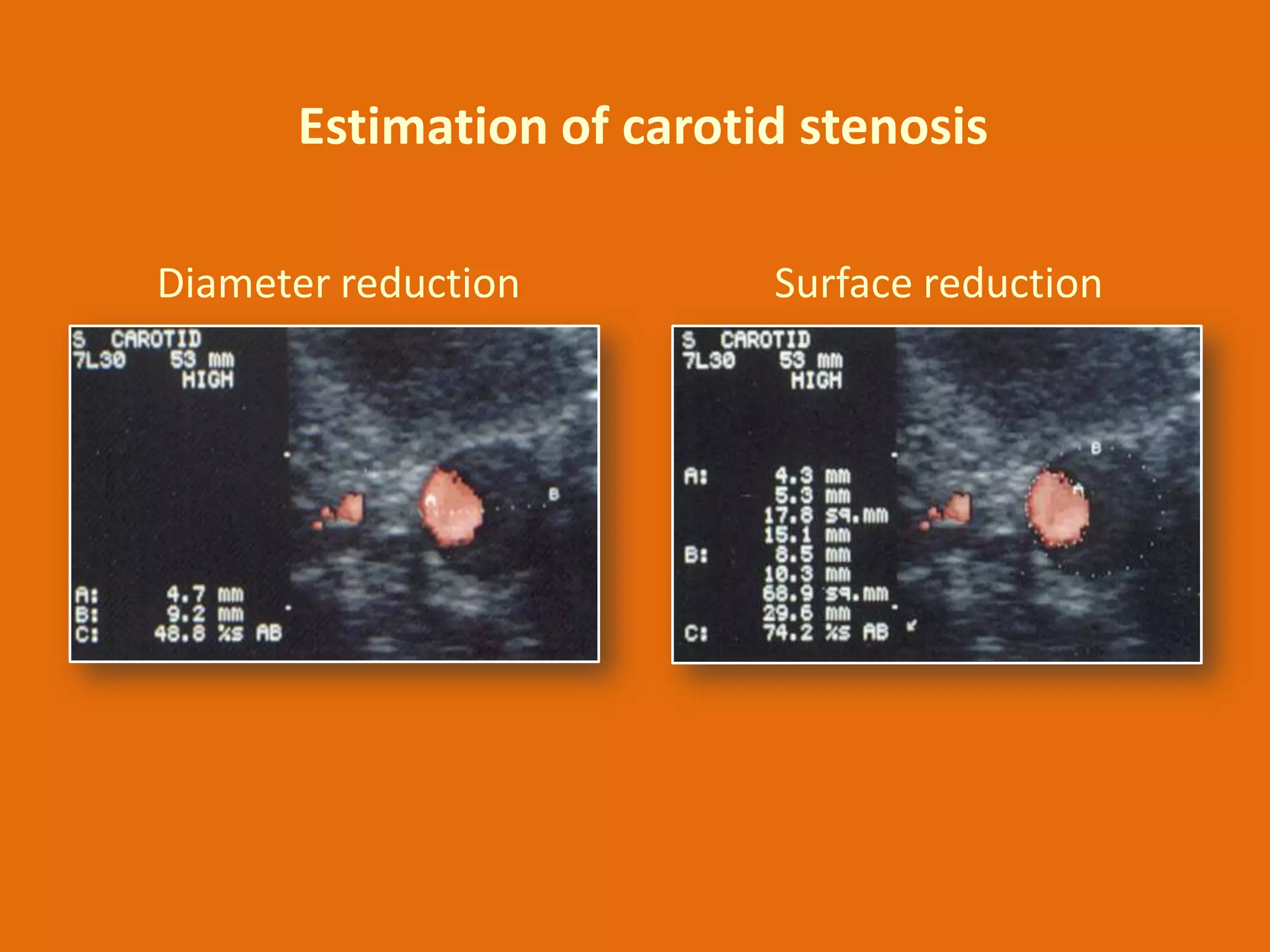
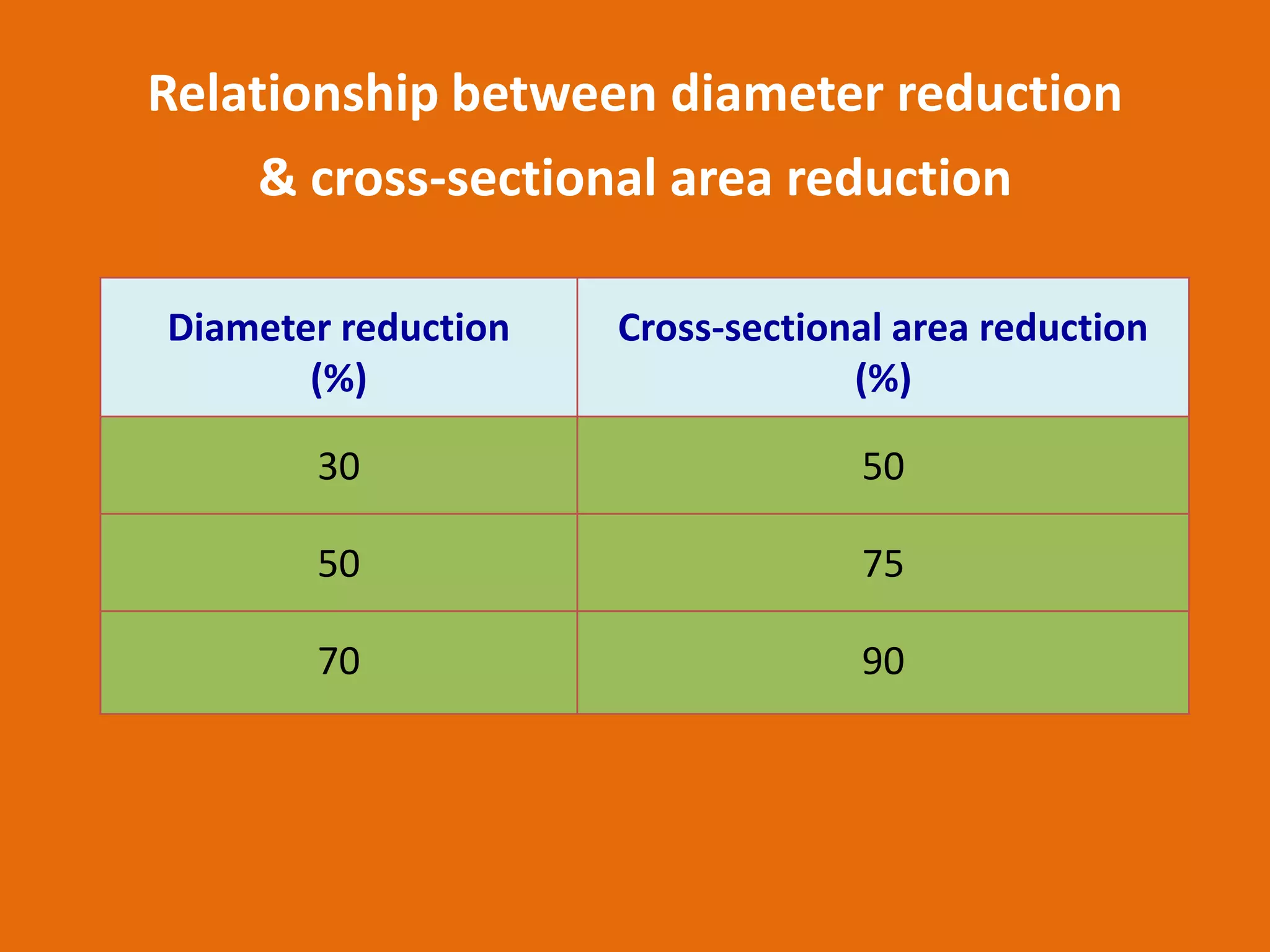
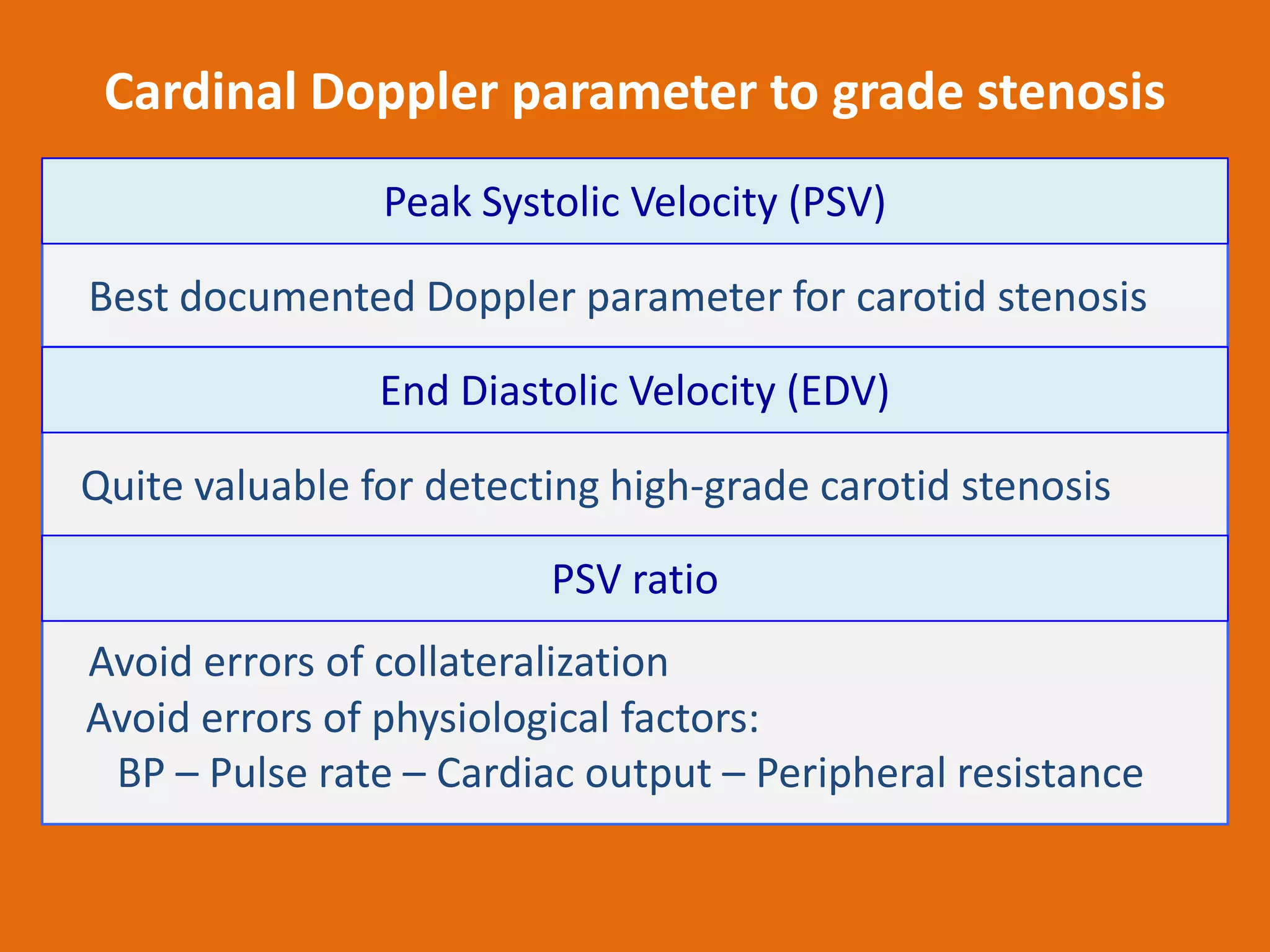
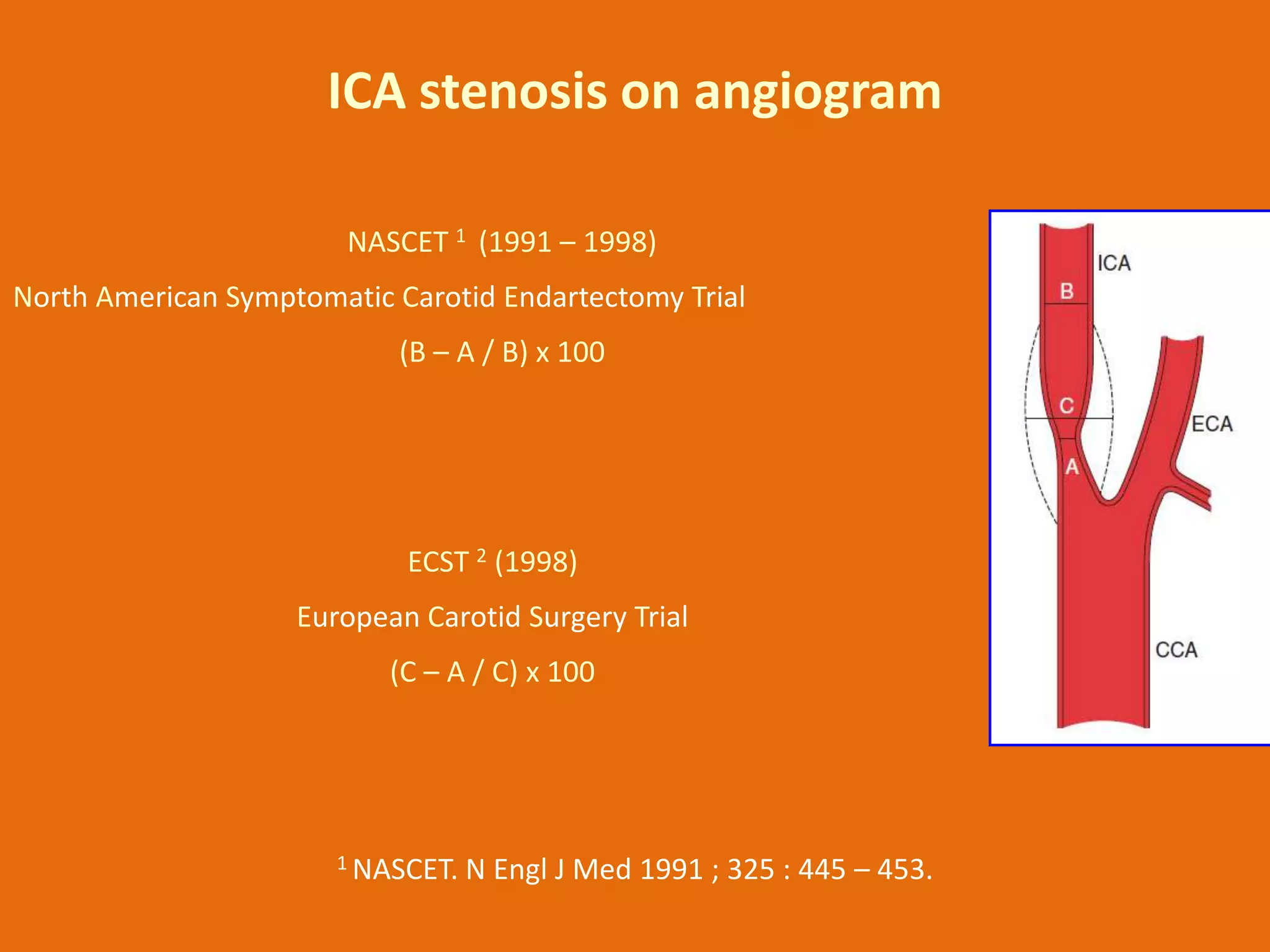
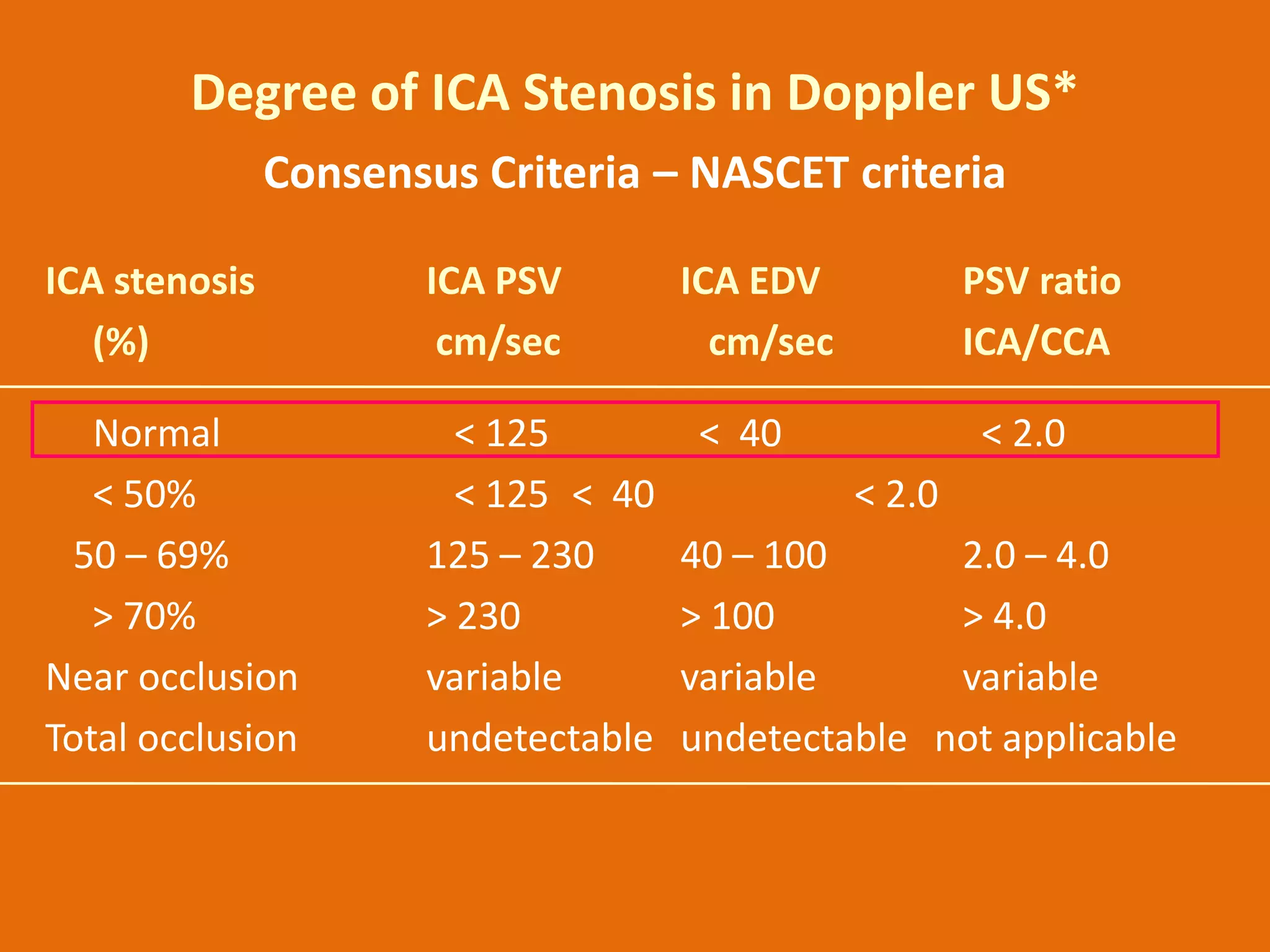
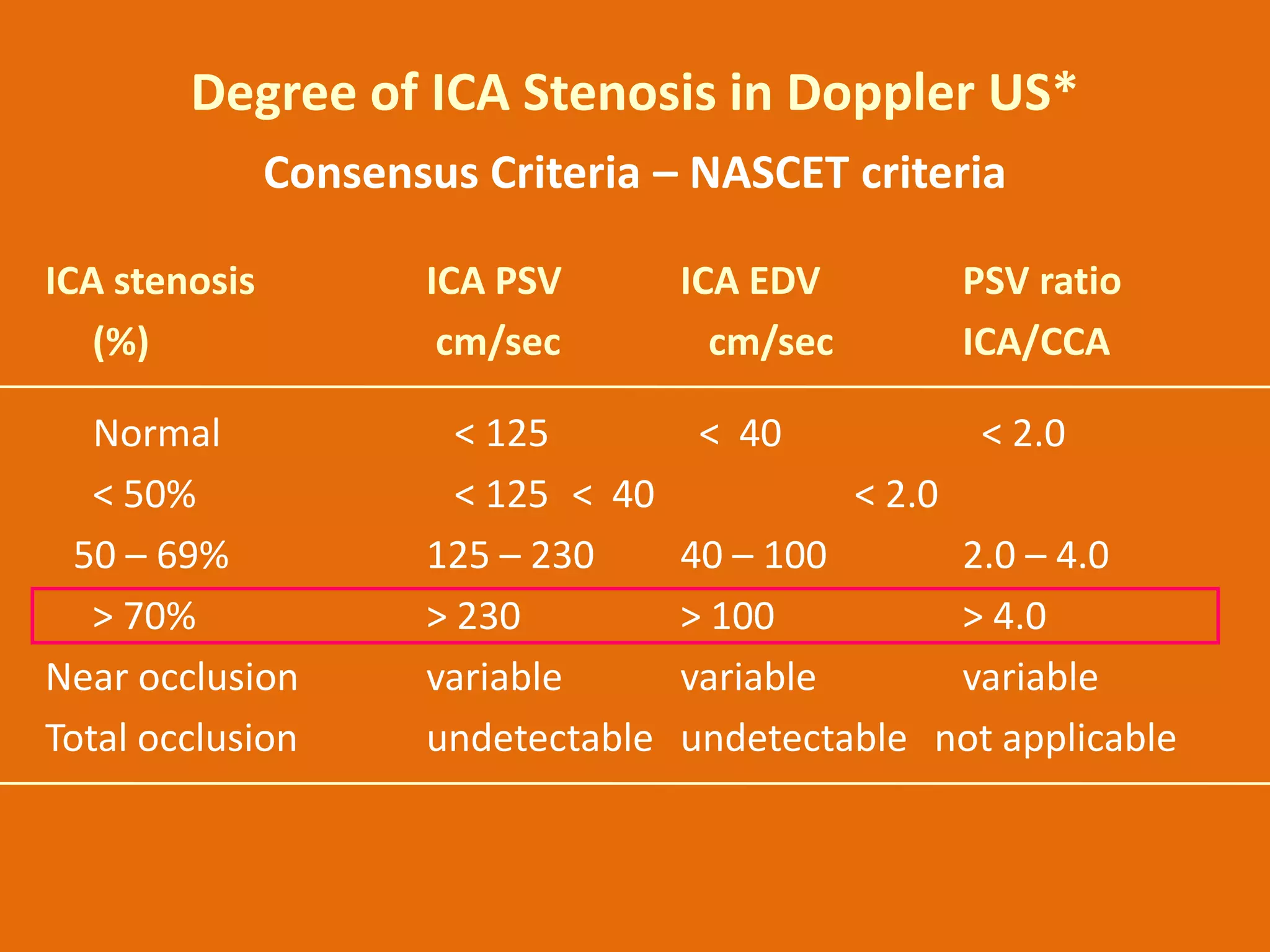
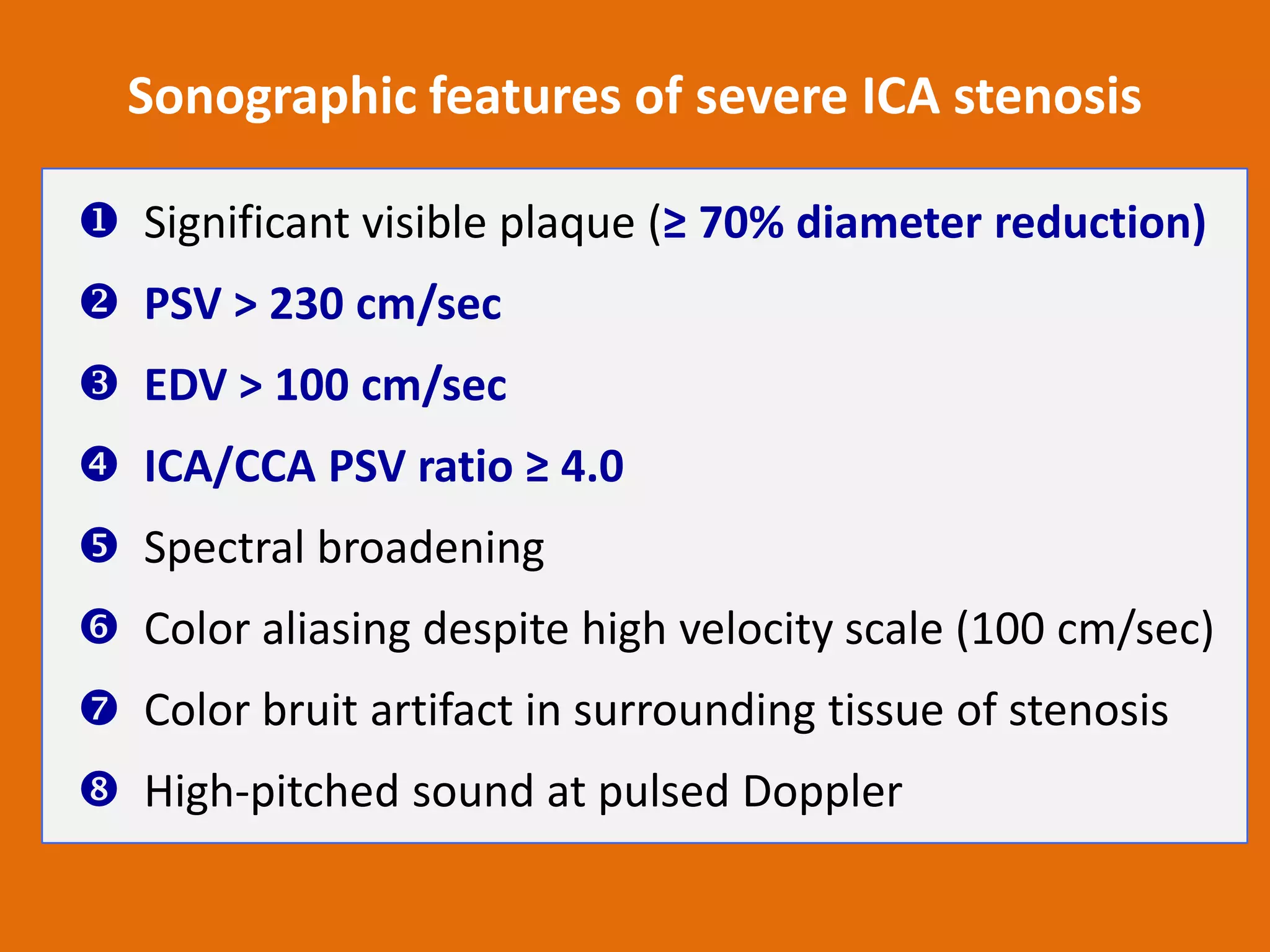
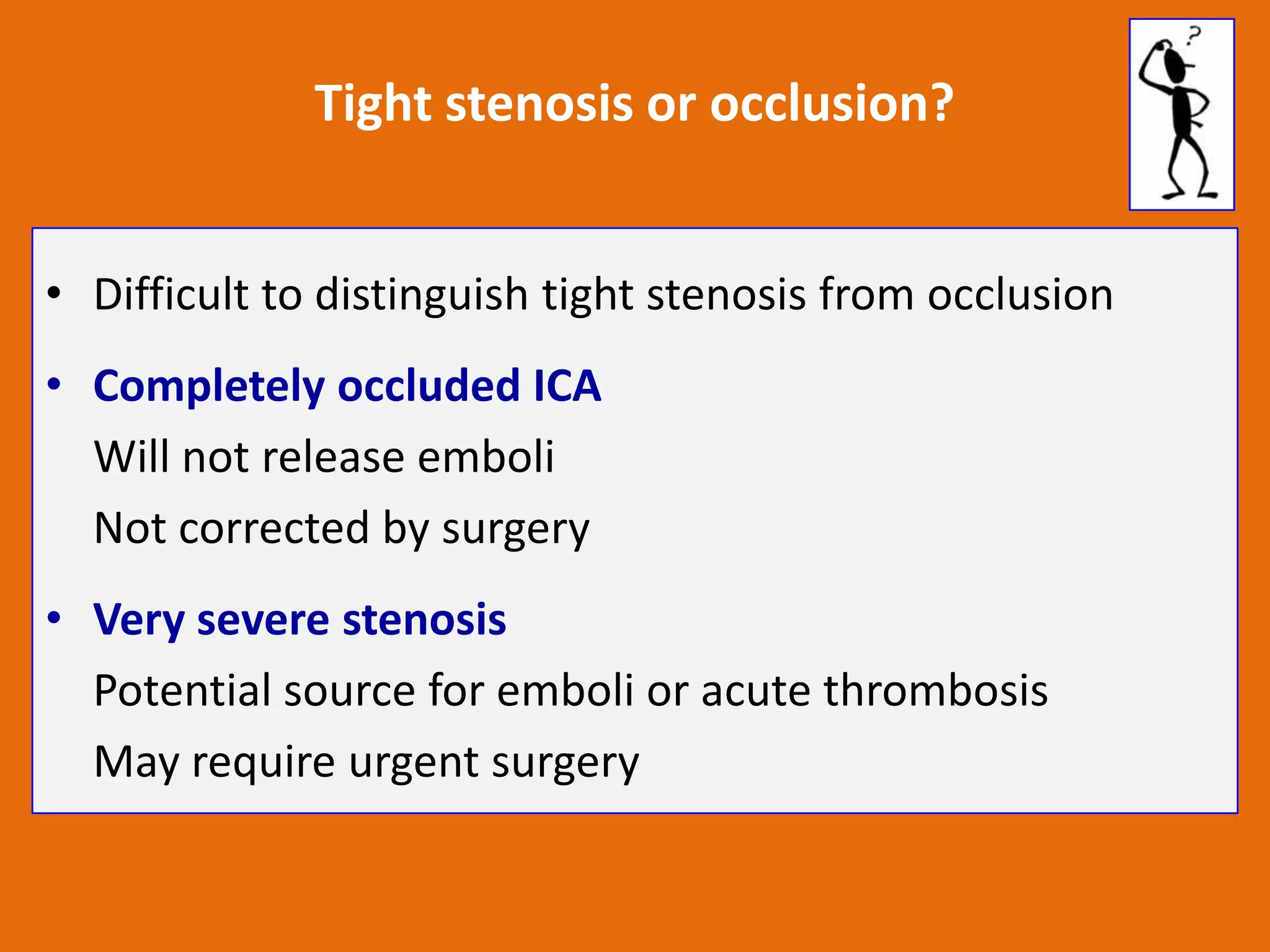
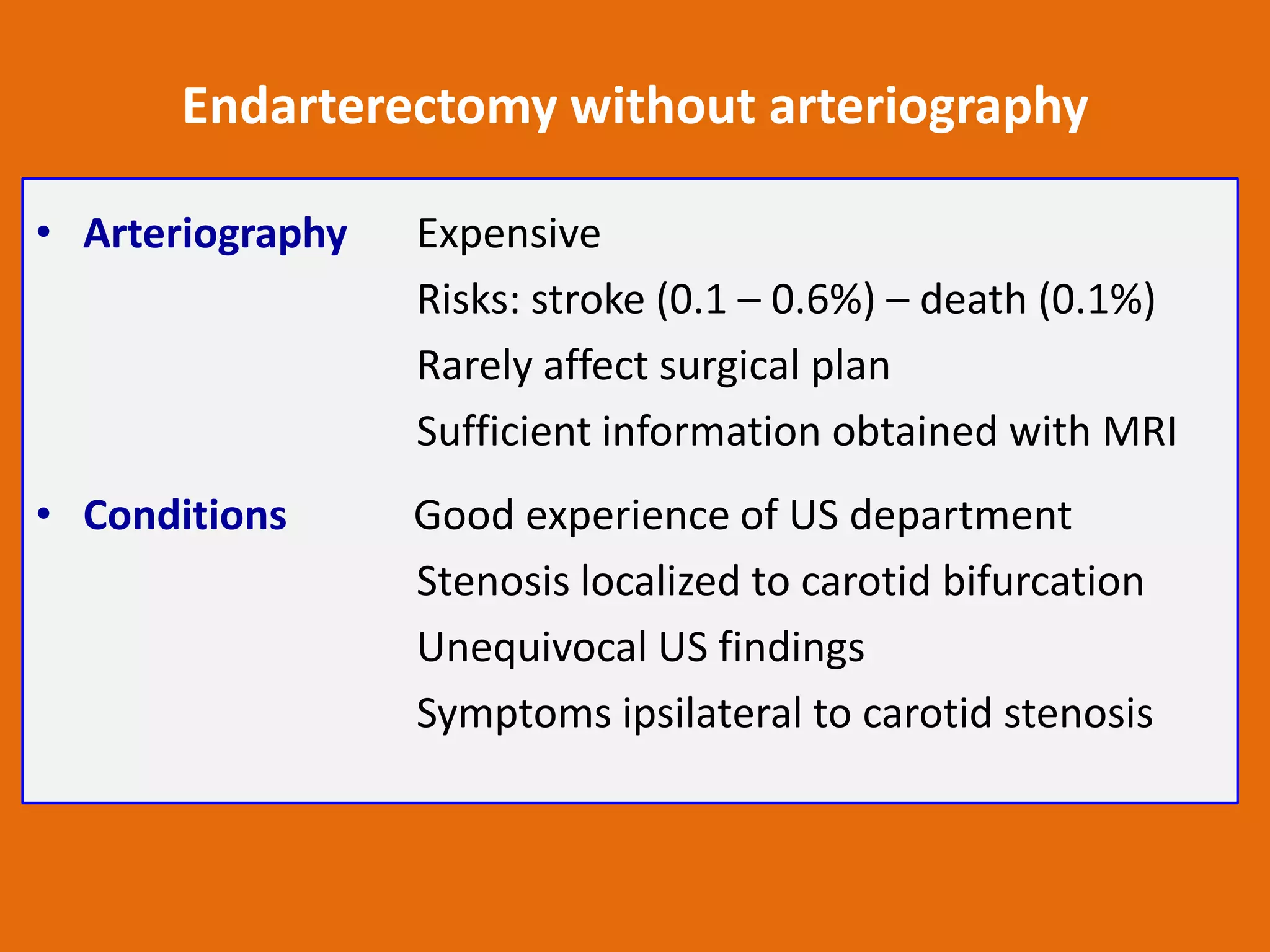
This document discusses carotid Doppler ultrasound. It begins by outlining the anatomy of the carotid arteries and normal Doppler findings. It then discusses causes of carotid artery disease including atherosclerosis. Extra-carotid diseases that can affect the carotid arteries are also mentioned. The document provides detailed guidance on performing and interpreting carotid Doppler ultrasound scans including evaluating the intima-media thickness, flow patterns, spectral analysis, and grading stenosis. Imaging features of normal and diseased arteries are presented along with tips for accurate evaluation.