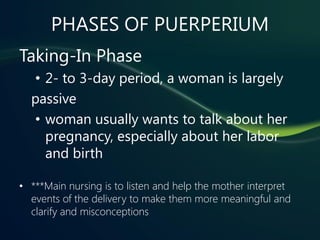
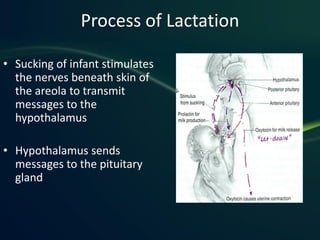
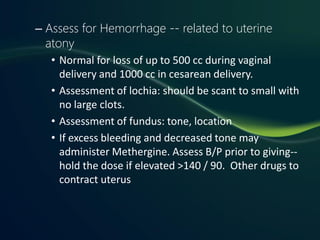
The postpartum period lasts 6 weeks after childbirth. During this time, the body undergoes both retrogressive and progressive changes. Psychologically, most women experience the taking-in, taking-hold, and letting-go phases as they adjust to their new role as parents. Nursing care focuses on assessment and support of the physiological changes like uterine involution and lactation. Pain management, nutrition, and ensuring adequate rest are also priorities in the postpartum period.