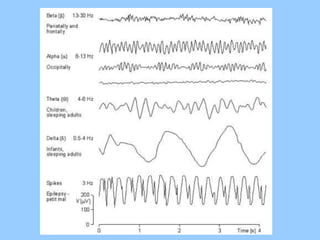
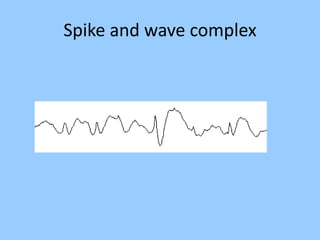
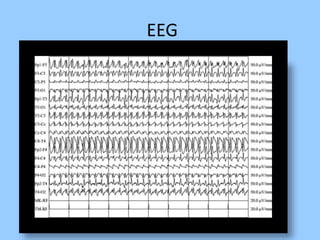
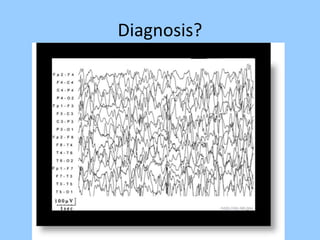
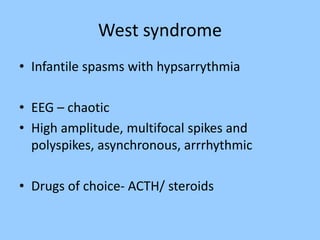
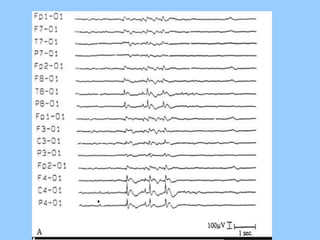
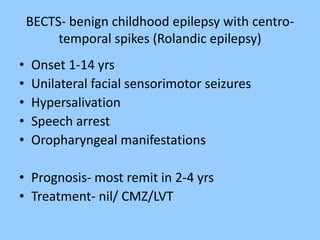
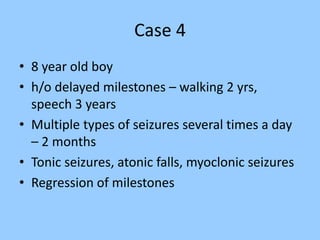
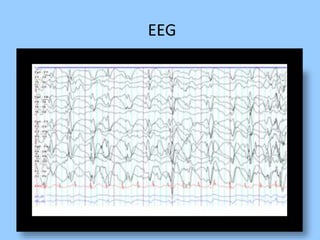
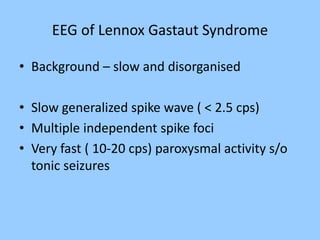
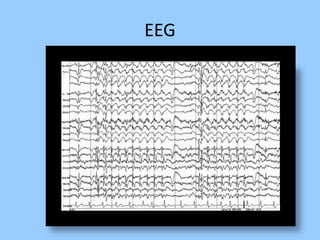
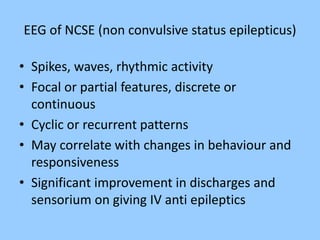
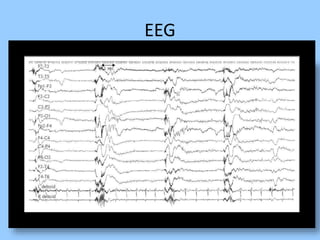
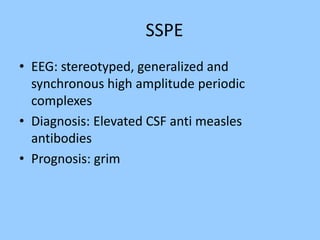
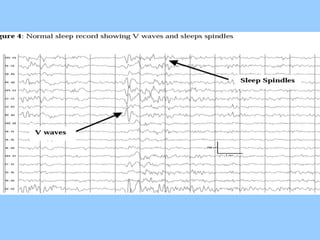
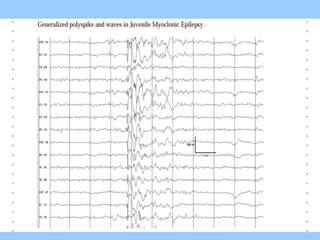
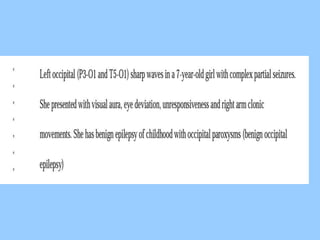
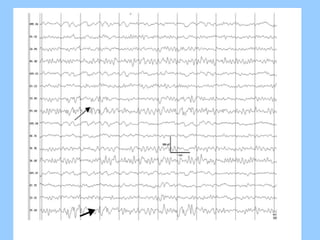
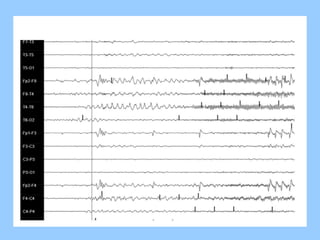
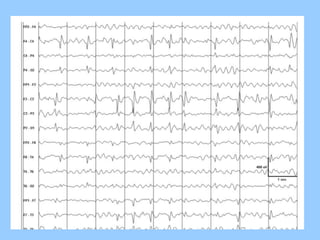
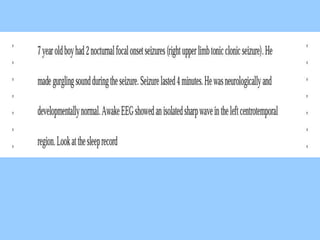
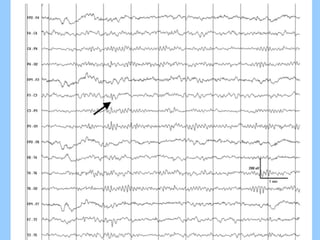
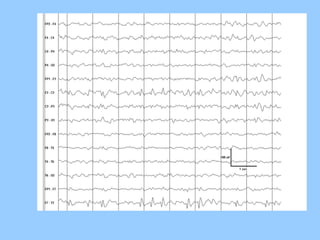
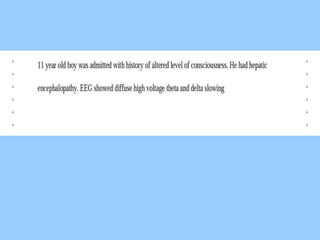
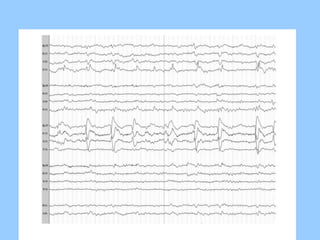
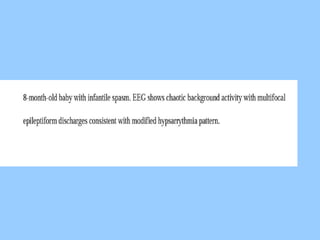
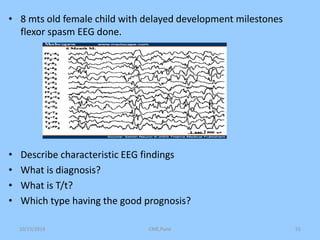
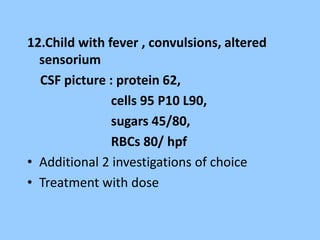
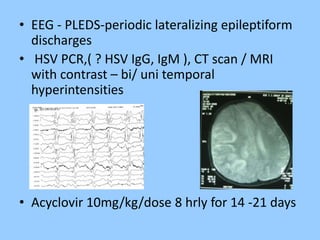
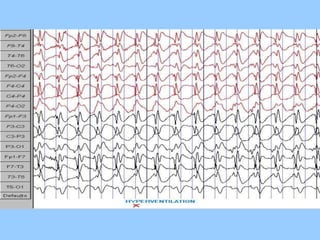
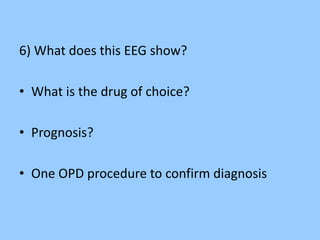
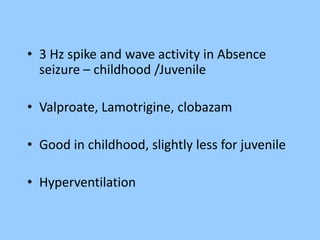
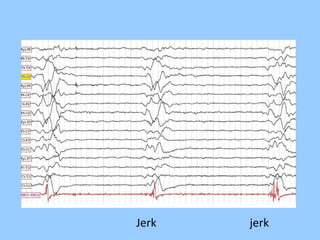
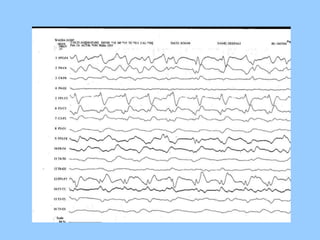
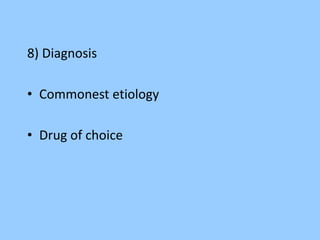
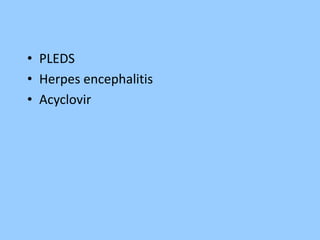
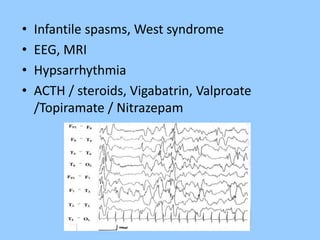
1. The document discusses EEG patterns and findings in various neurological conditions seen in children. It includes descriptions of normal EEG findings as well as abnormal patterns seen in conditions like absence seizures, West syndrome, benign childhood epilepsy with centrotemporal spikes, Lennox-Gastaut syndrome, non-convulsive status epilepticus, subacute sclerosing panencephalitis, and herpes encephalitis.
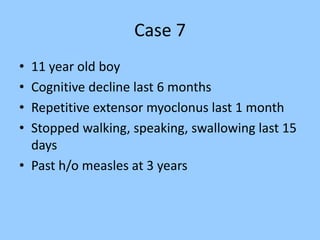
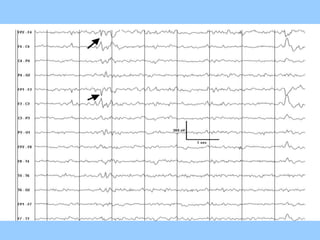
2. Case studies are presented with clinical histories and EEG findings to illustrate different pathologies. Treatment options are also mentioned for many of the conditions.
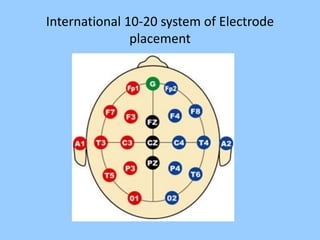
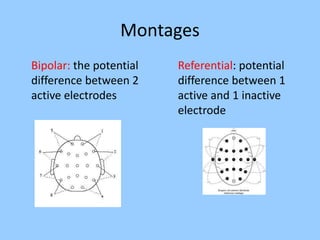
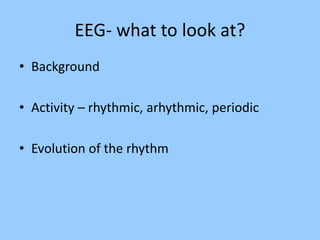
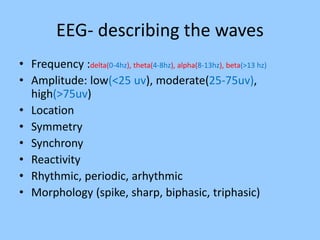
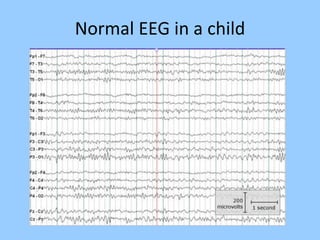
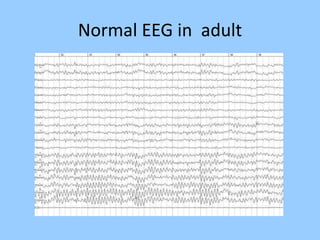
3. International standards for EEG electrode placement and recording parameters are reviewed. Characteristics of different EEG waves, amplitudes, and patterns are described.






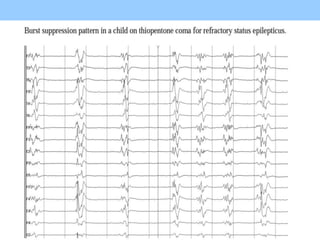
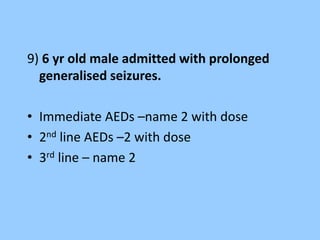
![• Lorazepam [0.05mg/kg],
• Diazepam [0.3mg/kg],
• midazolam[ 0.2mg/kg]
• Phenytoin[ 20mg/kg],
• phenobarb[20/kg]
• Midazolam drip,
• propofol,
• thiopentol](https://image.slidesharecdn.com/eeg-141015043102-conversion-gate01/85/Eeg-in-pediatric-DNB-PEDIATRIC-69-320.jpg)
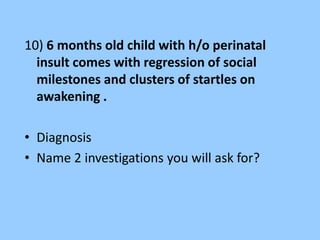
![• Station No : A term newborn who required resuscitation at
birth with a 5 minute APGAR of 5 is admitted in NICU. The
neonate had seizures in first 12 hrs of life
• Identify the findings-[1]
• What is the significance of this finding- [1/2]
• Name of the staging system other than Sarnat and Sarnat and
give its component- [1]](https://image.slidesharecdn.com/eeg-141015043102-conversion-gate01/85/Eeg-in-pediatric-DNB-PEDIATRIC-72-320.jpg)