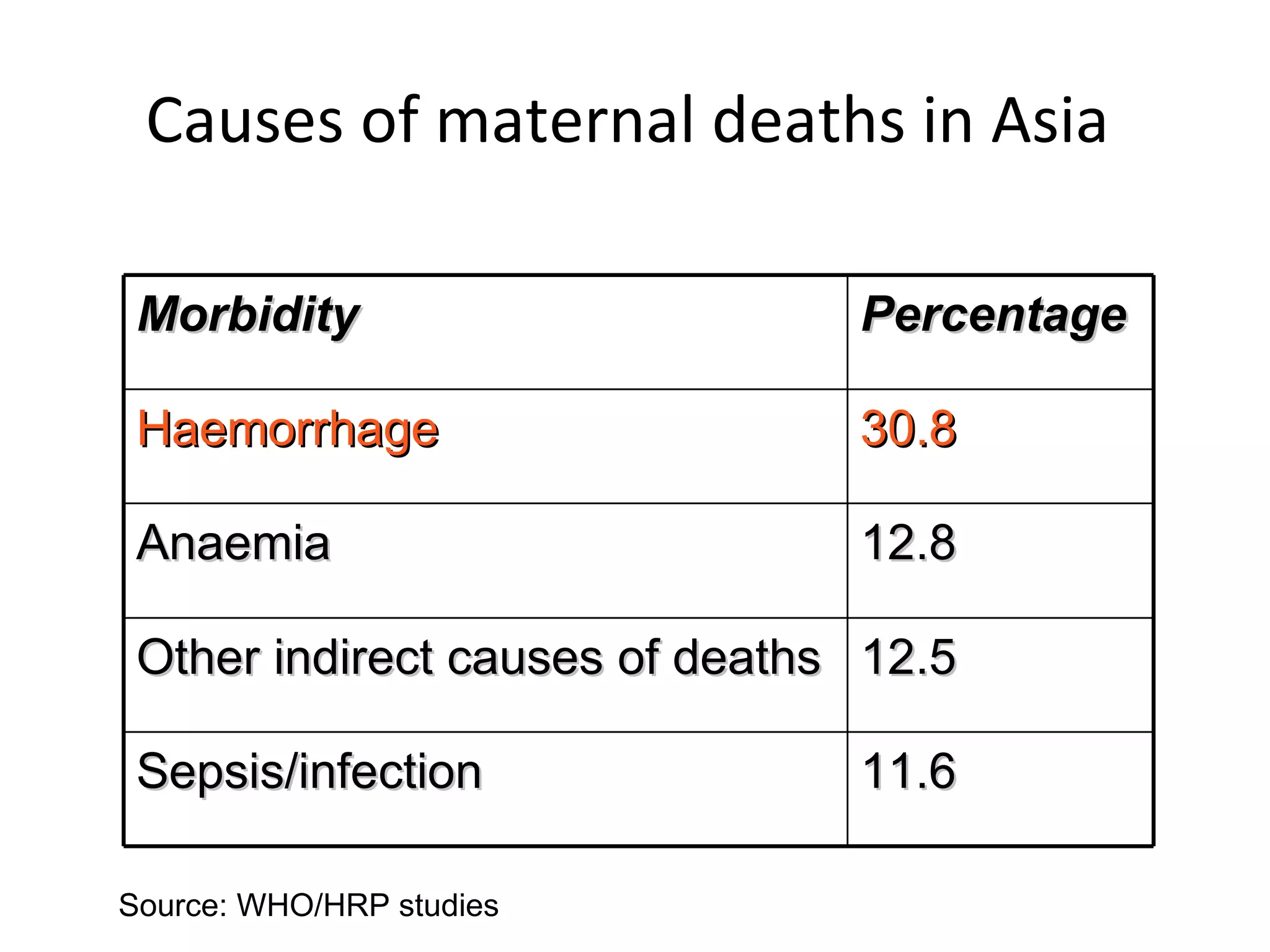
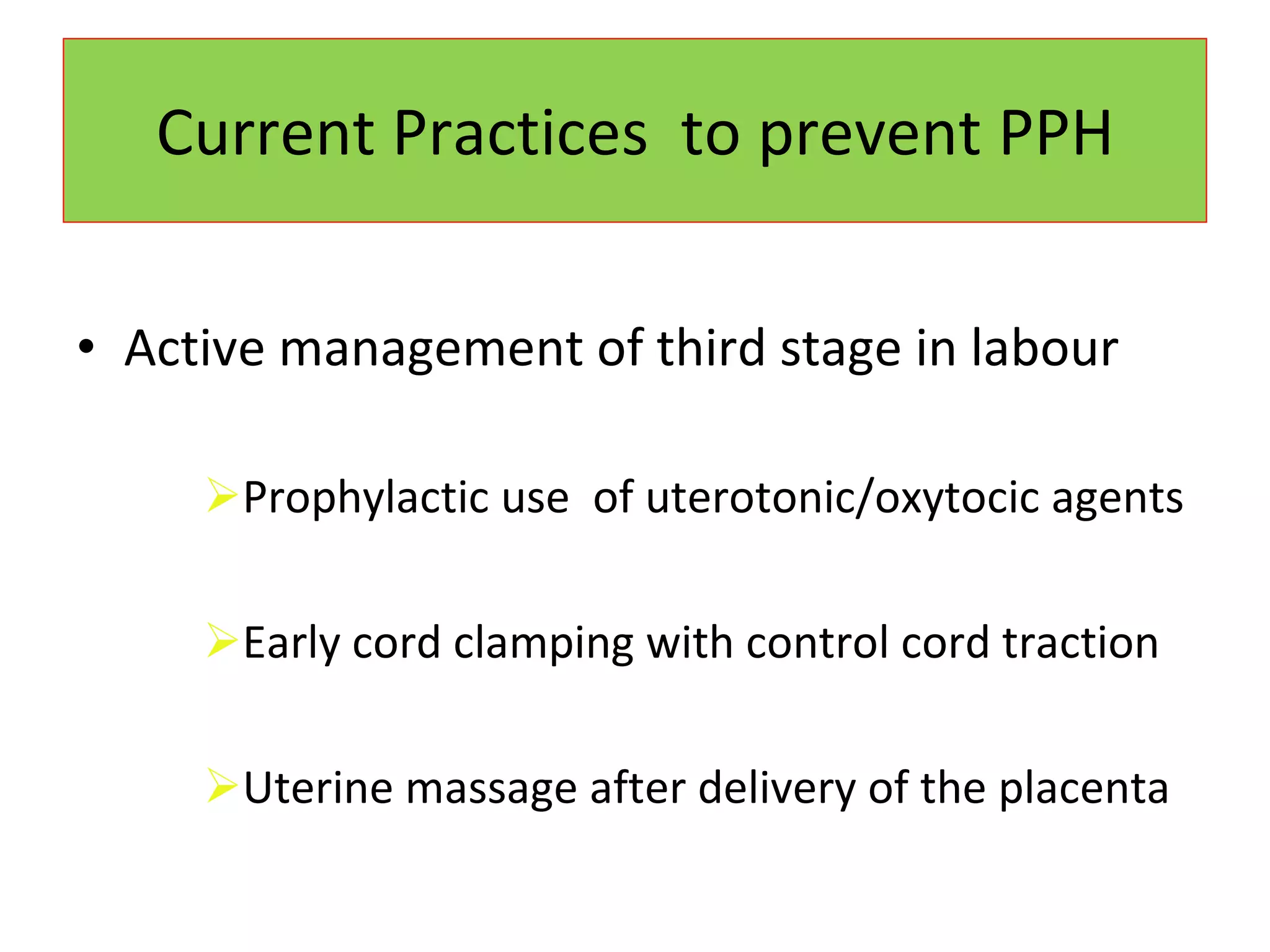
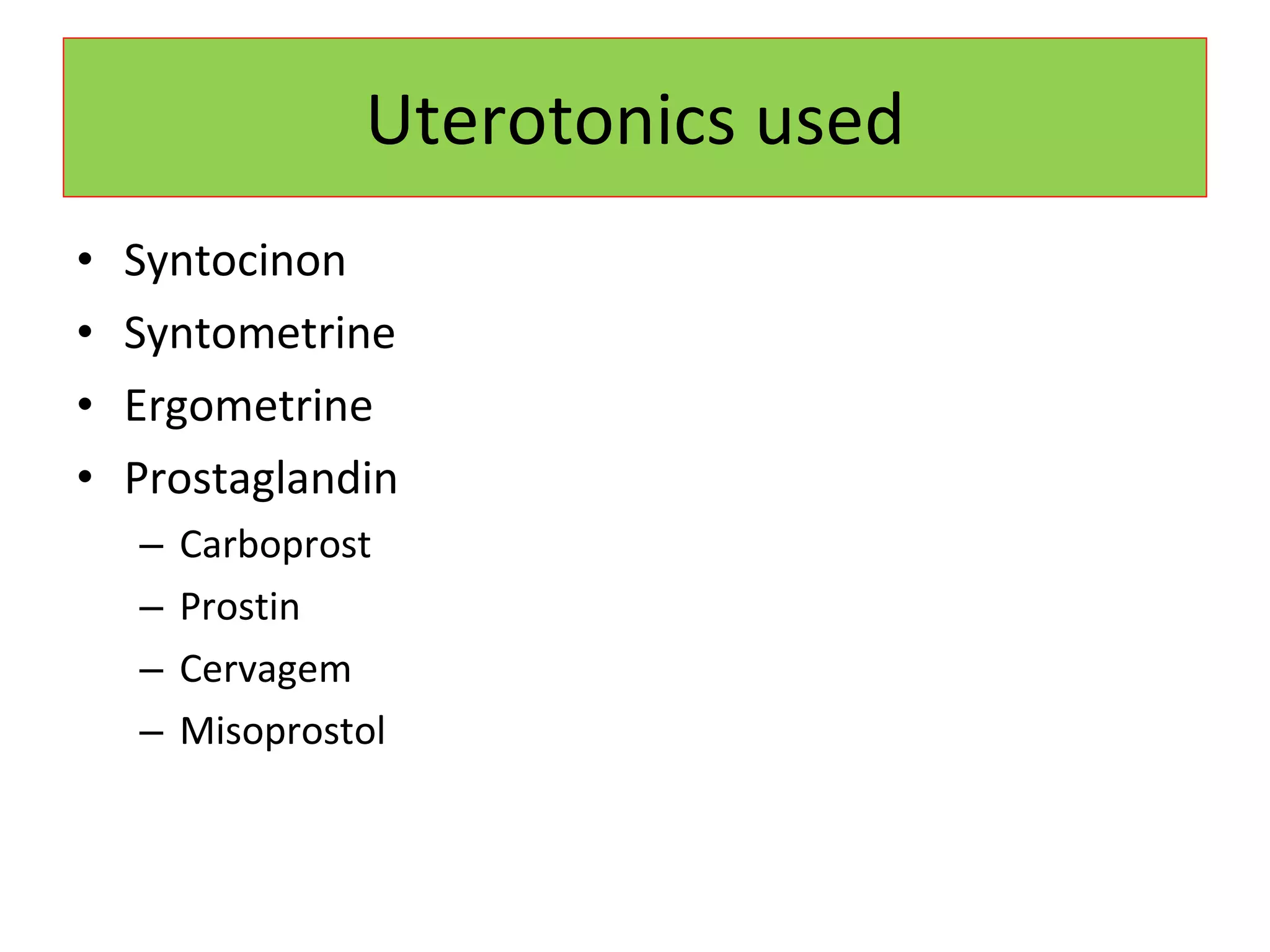
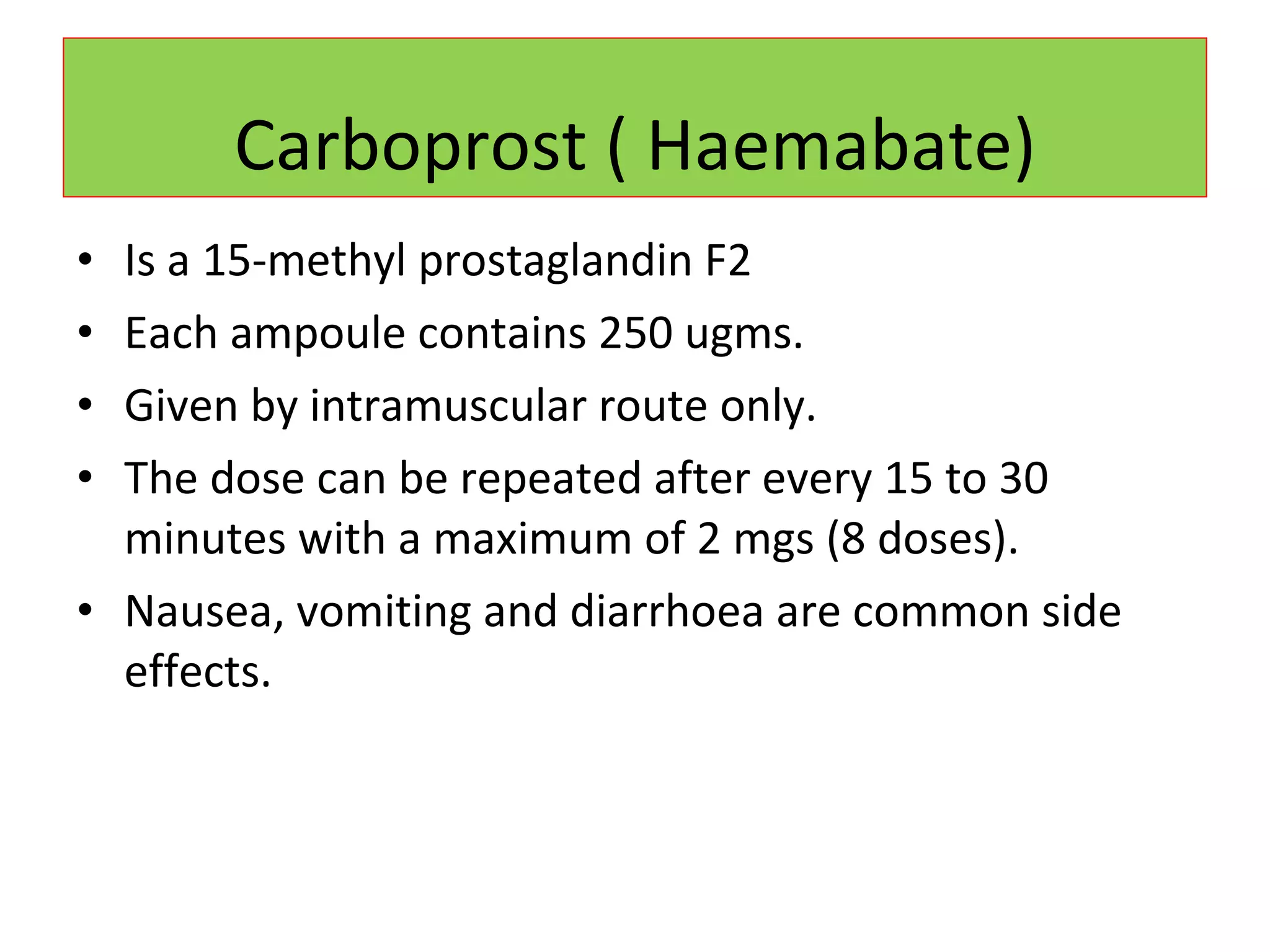
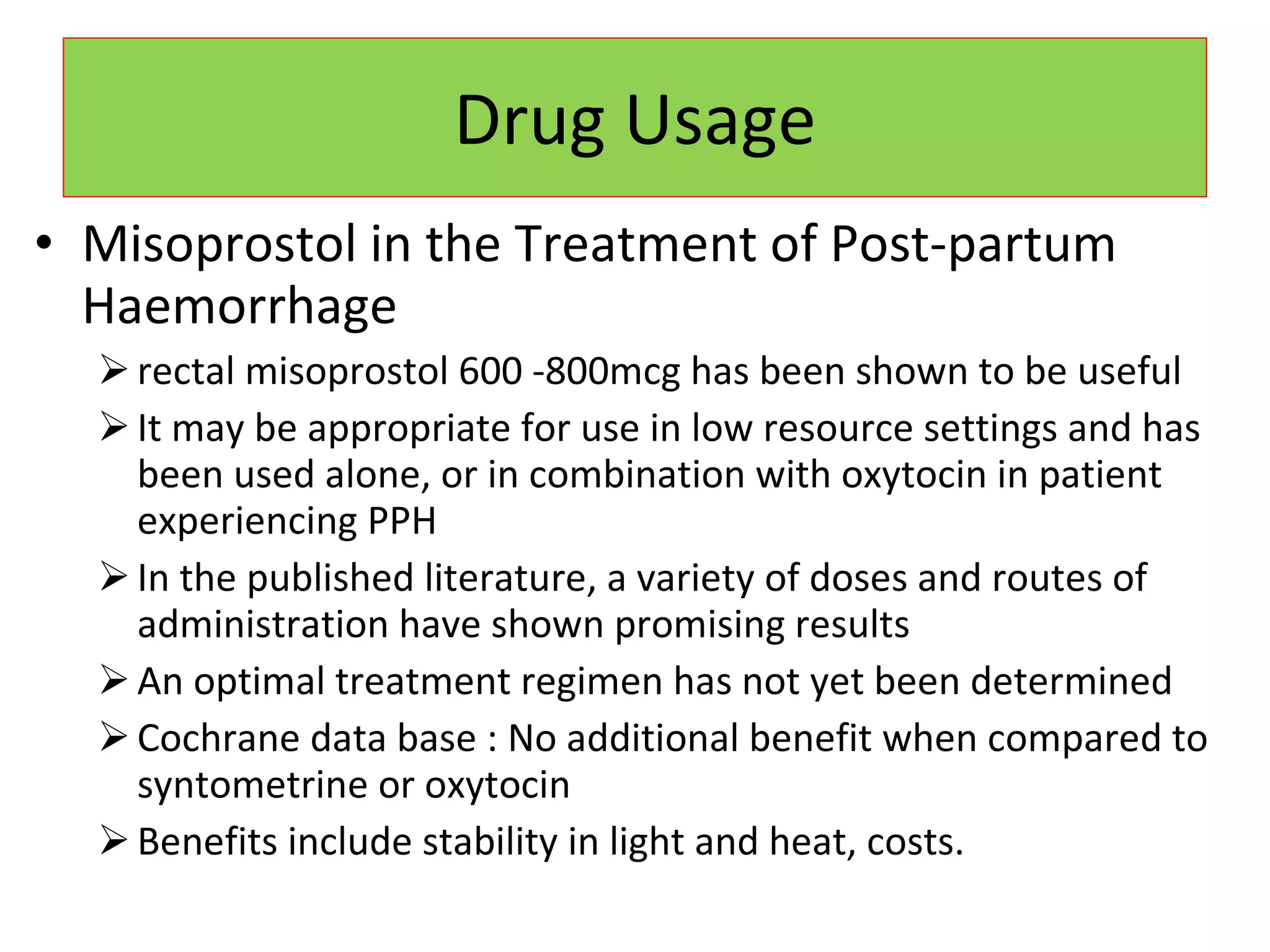
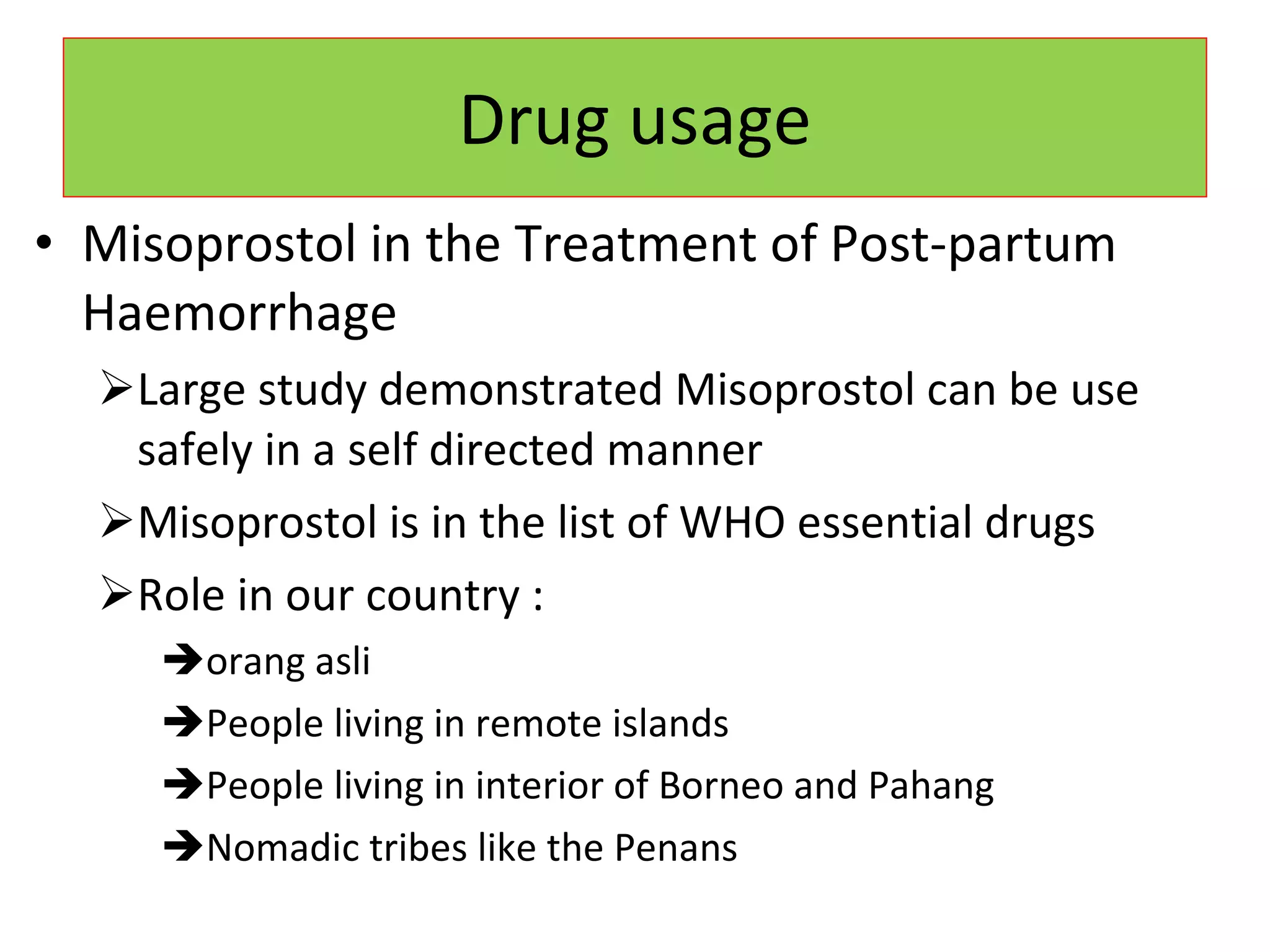
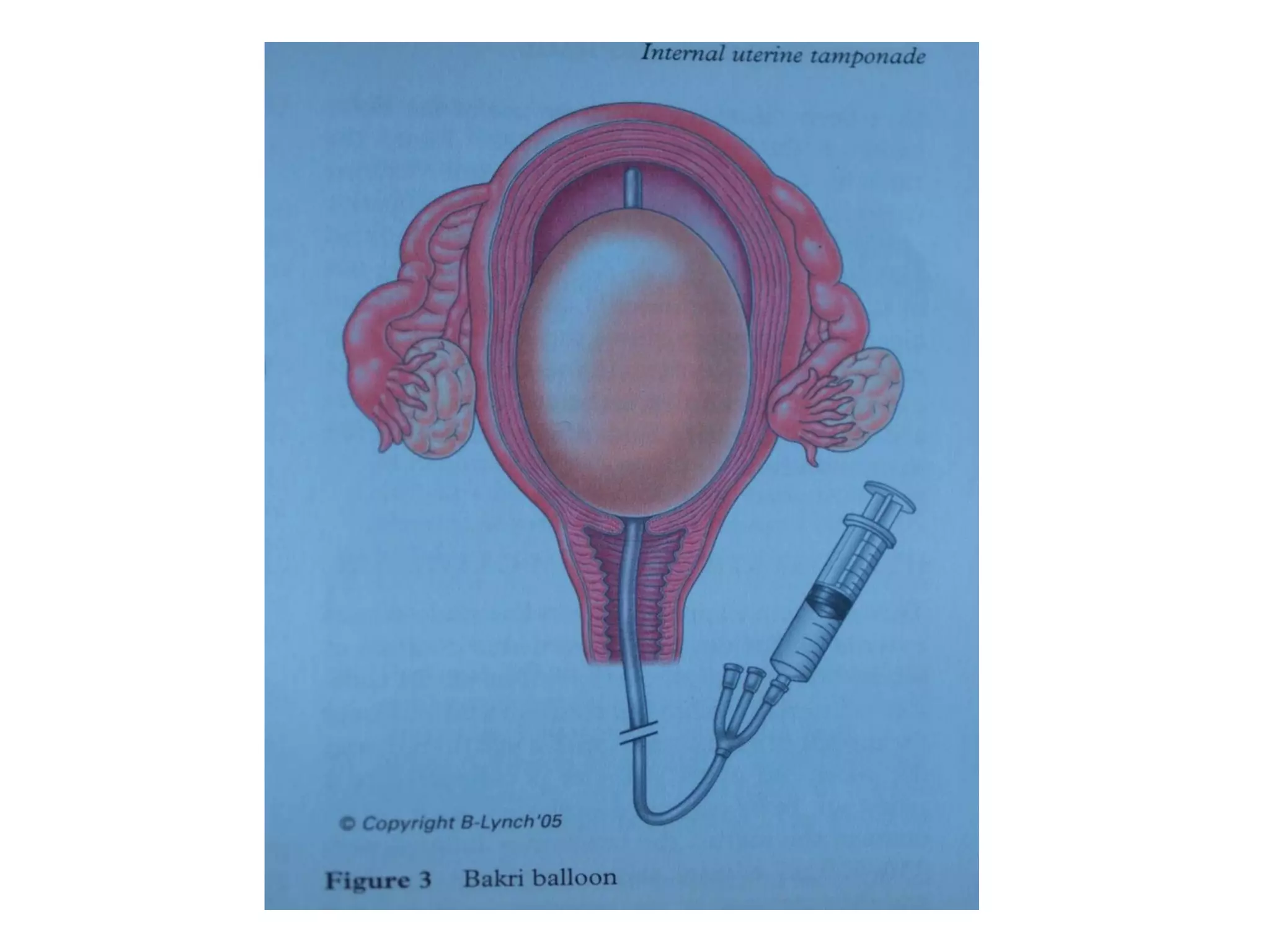
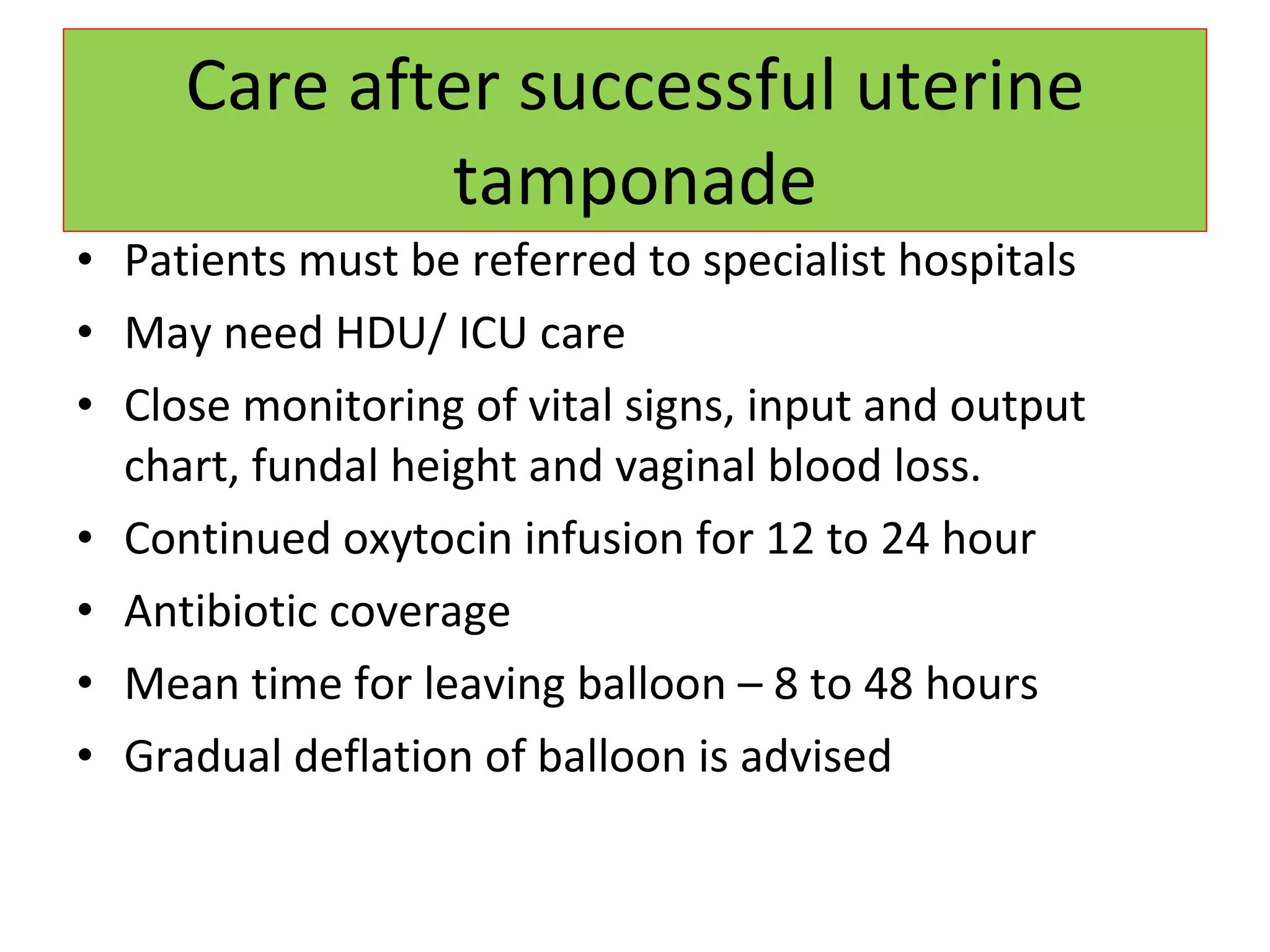
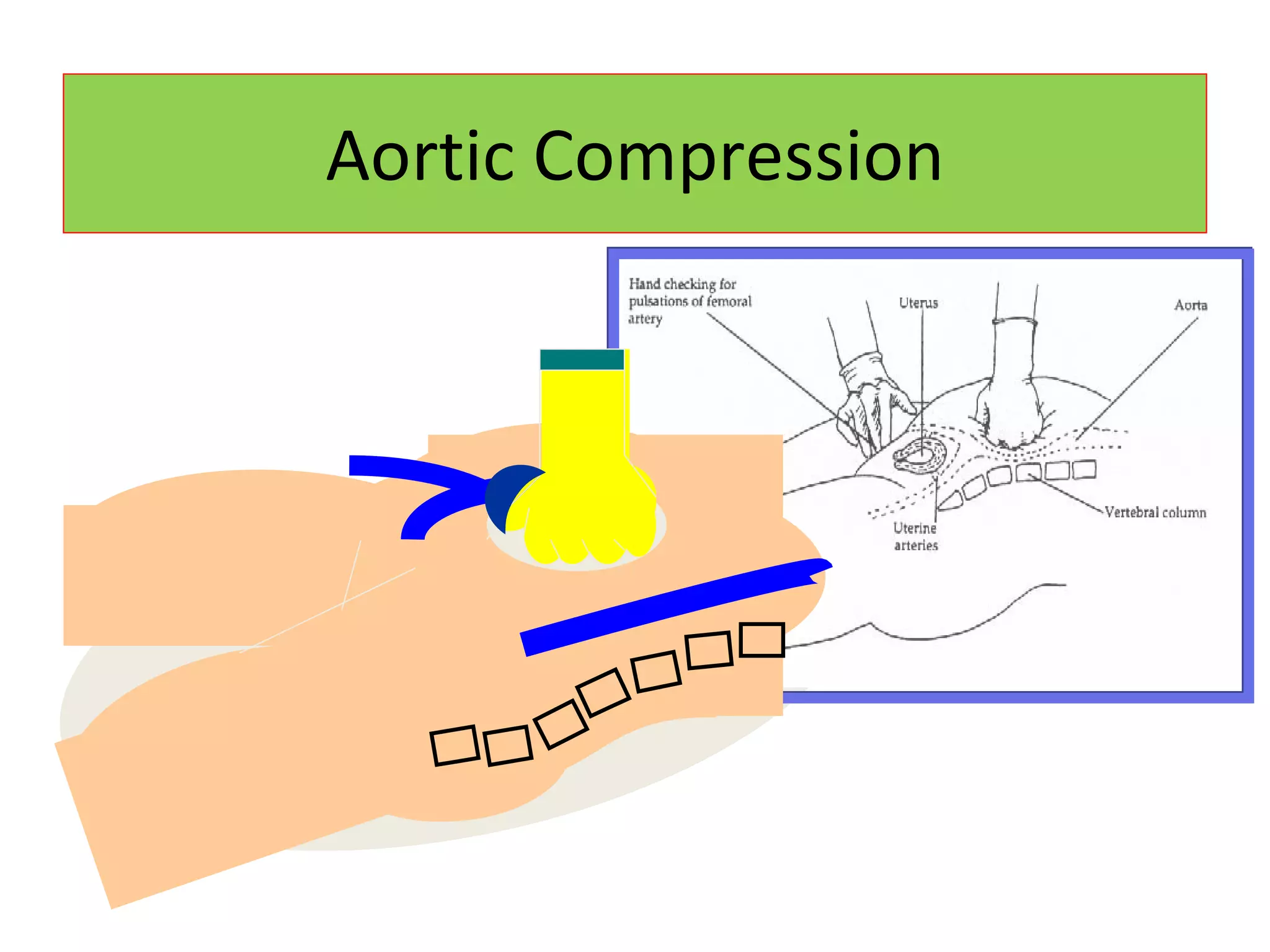
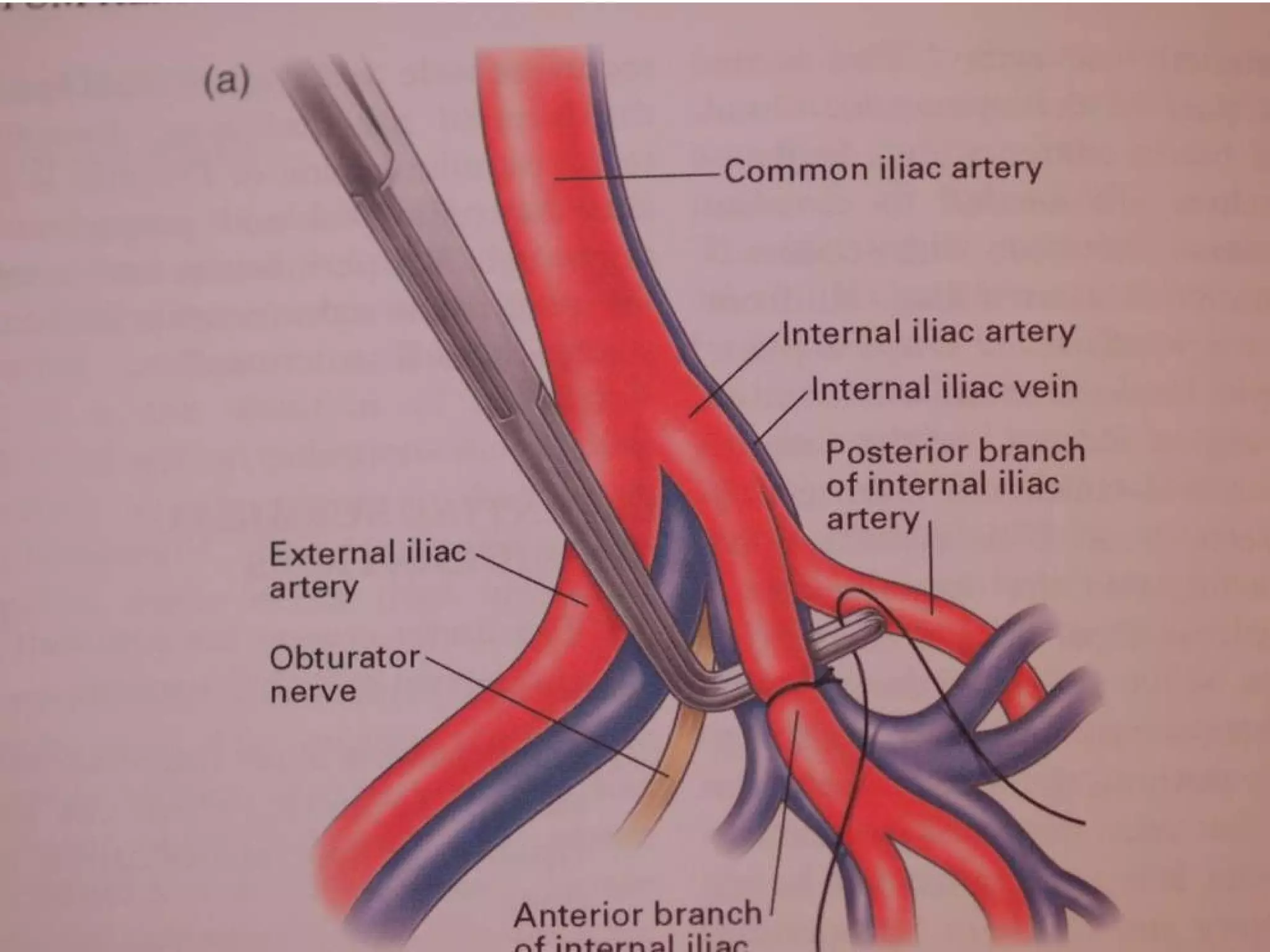
The document discusses non-surgical management of postpartum hemorrhage (PPH). It outlines that PPH is a leading cause of maternal mortality, with causes including uterine atony, retained placenta, and coagulation disorders. Prevention focuses on risk identification and active management of the third stage of labor. Medical management includes uterotonics like oxytocin, carboprost, and misoprostol. Temporary measures like uterine packing, balloon tamponade, and embolization can control bleeding while arranging transfer for hysterectomy if needed.