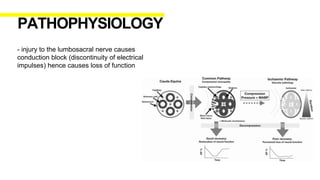
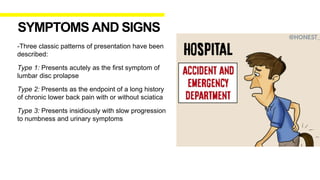
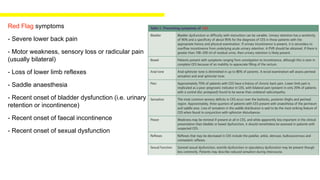
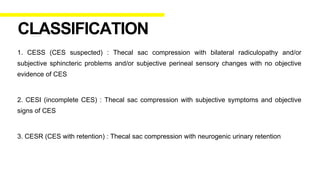
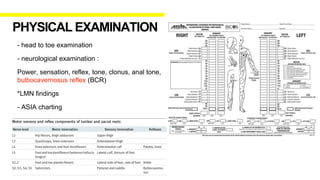
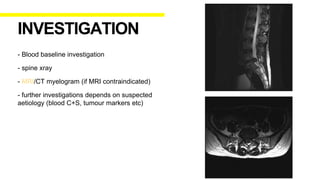
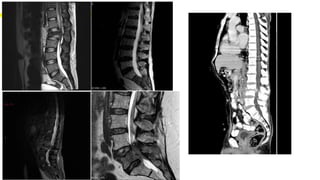
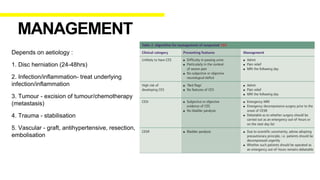
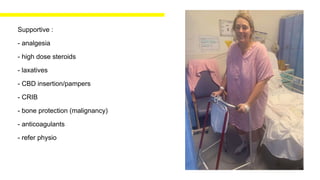
Cauda Equina Syndrome (CES) involves compression of the bundle of nerves at the end of the spinal cord, and can cause leg weakness, loss of sensation, and bladder/bowel issues. A herniated disc is a common cause of CES. Urgent surgical treatment is important to prevent permanent neurological damage. Early diagnosis and treatment leads to better outcomes, especially for bladder function.