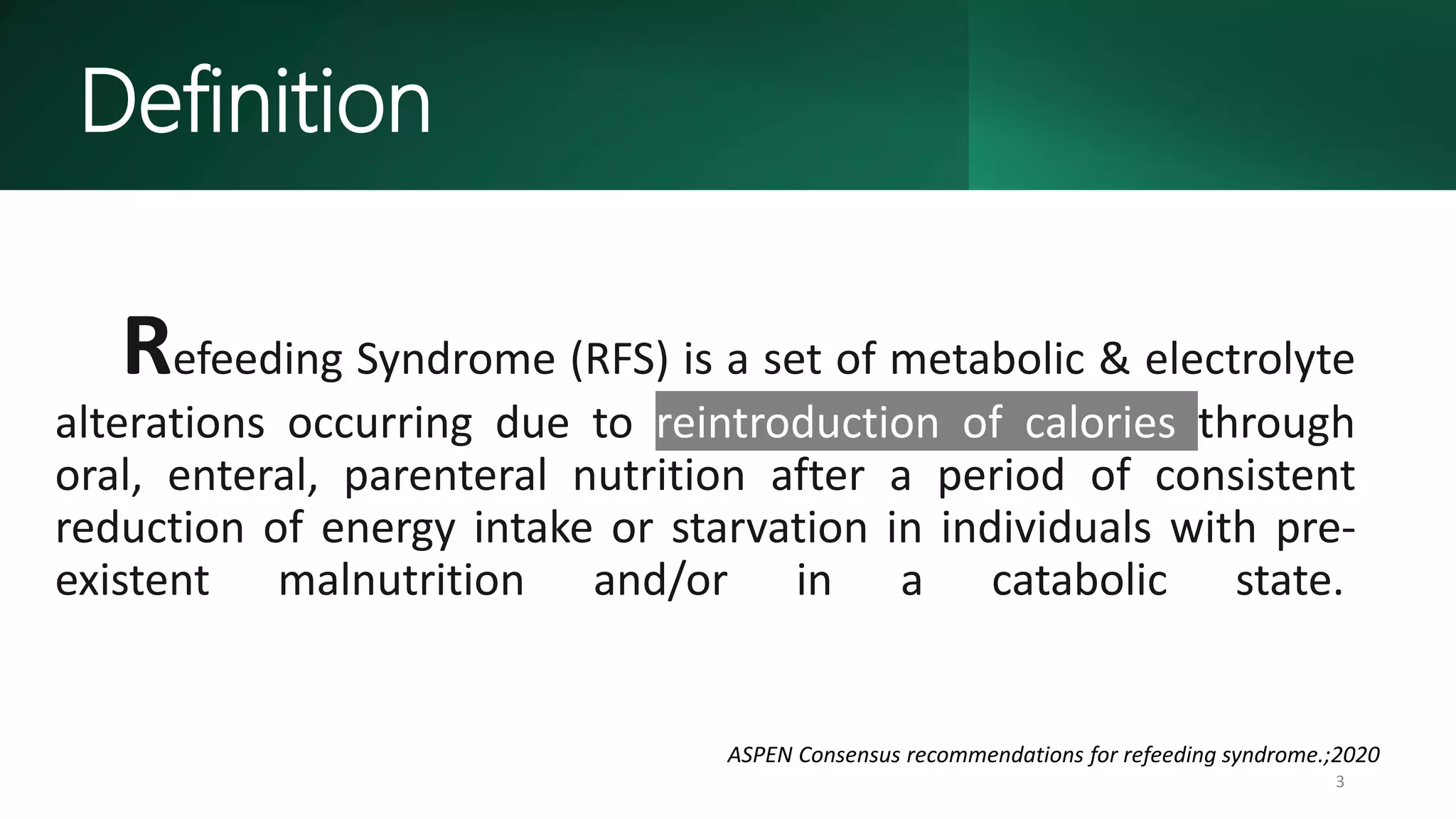
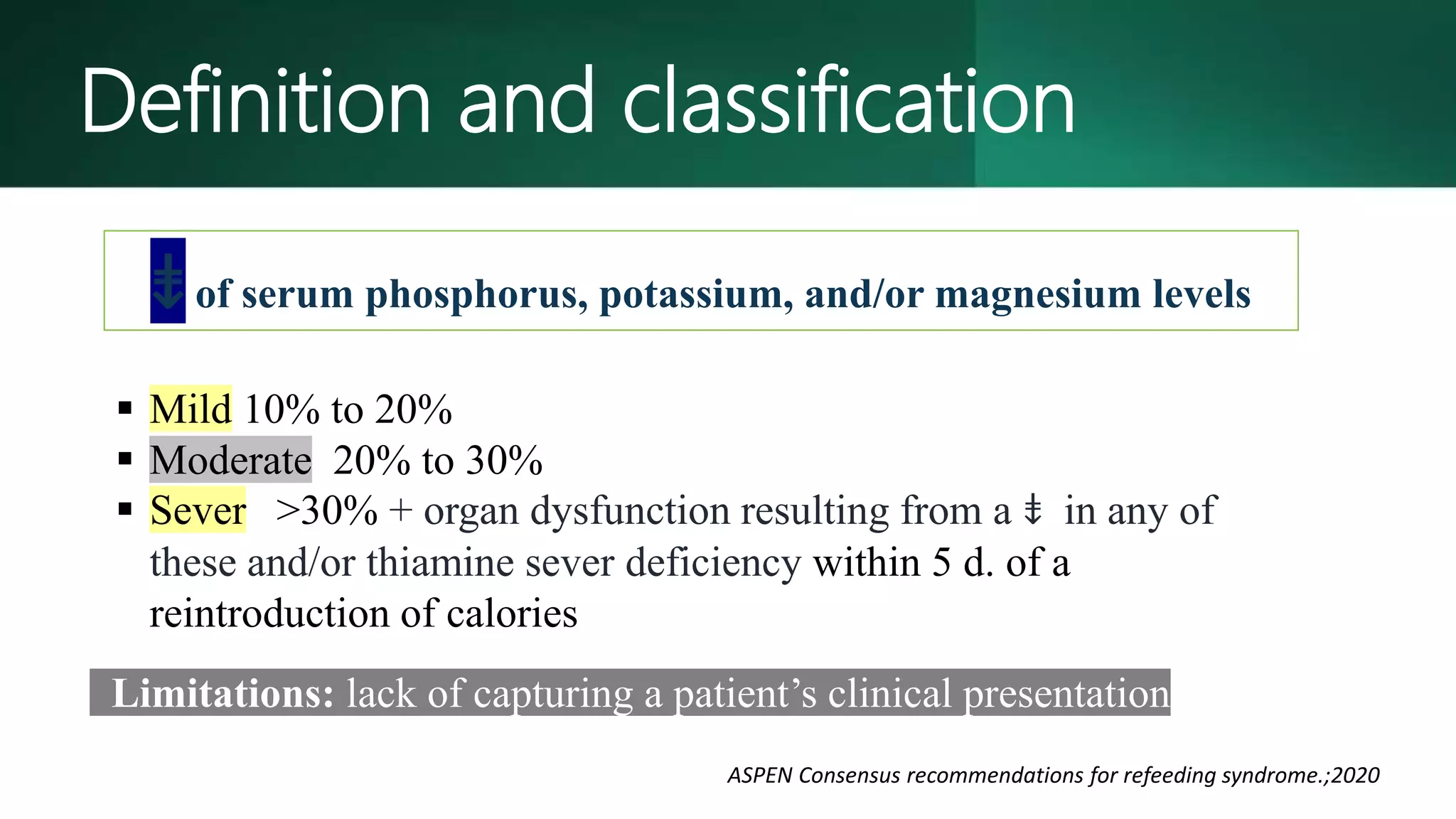
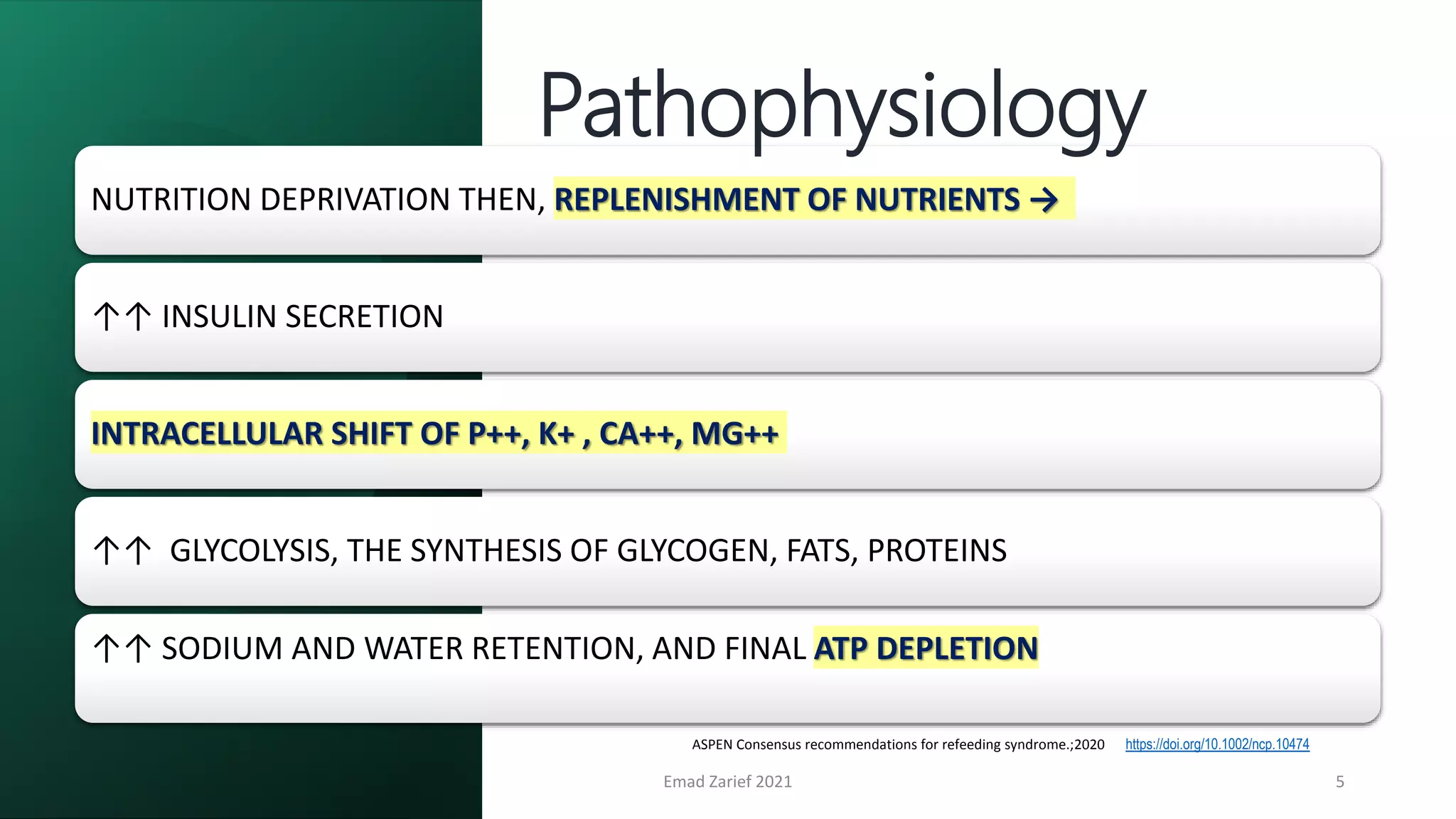
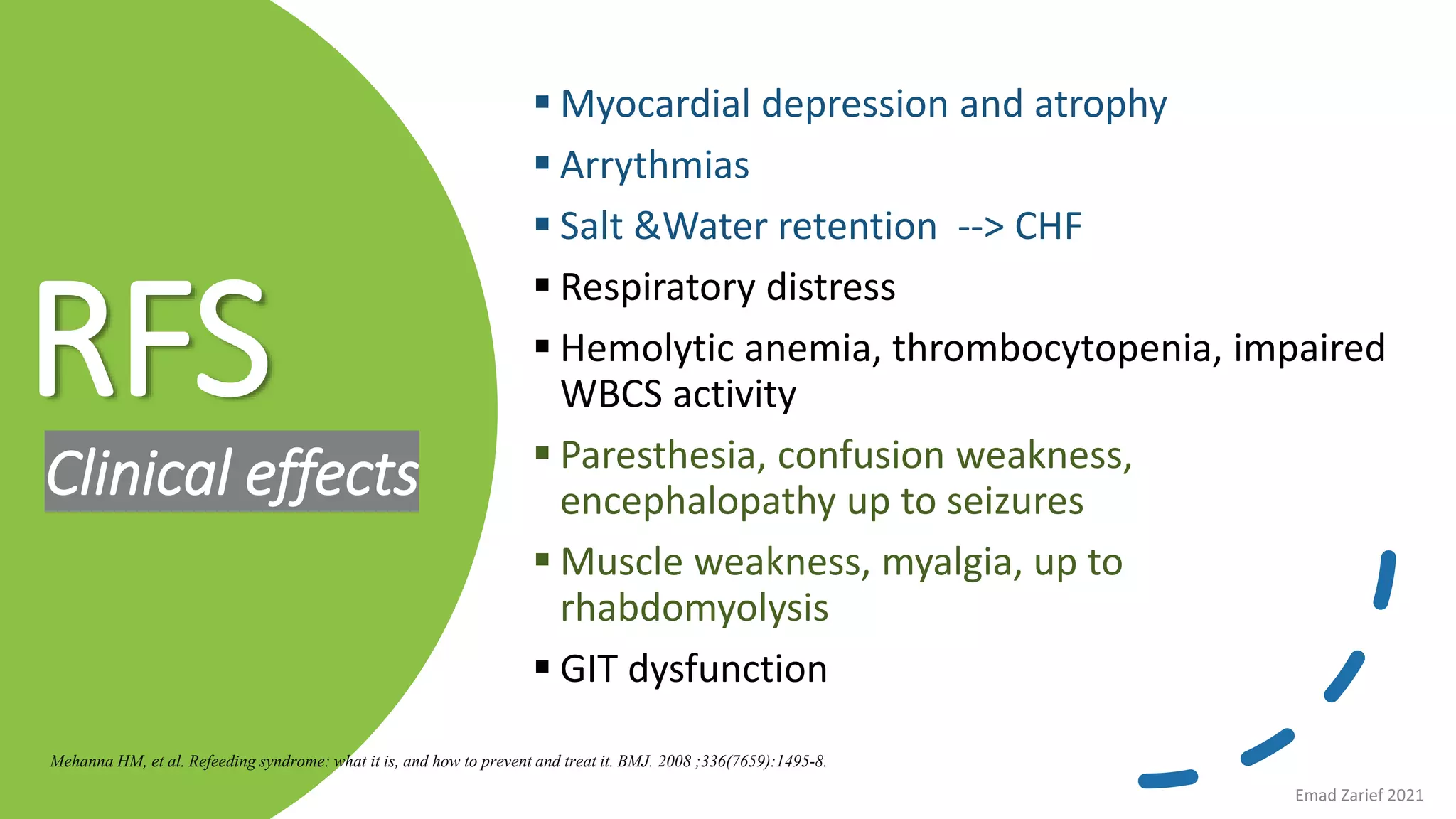
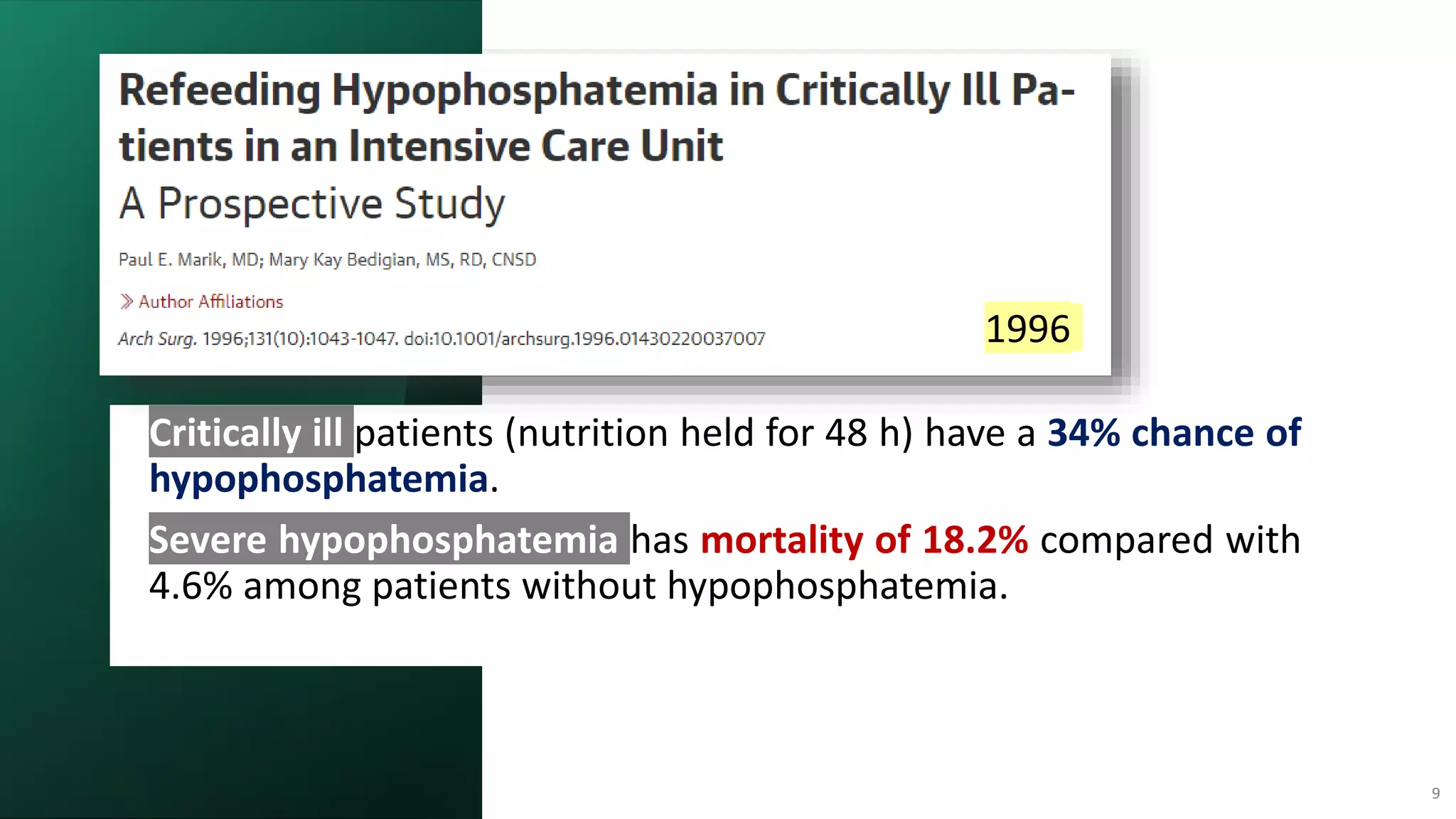
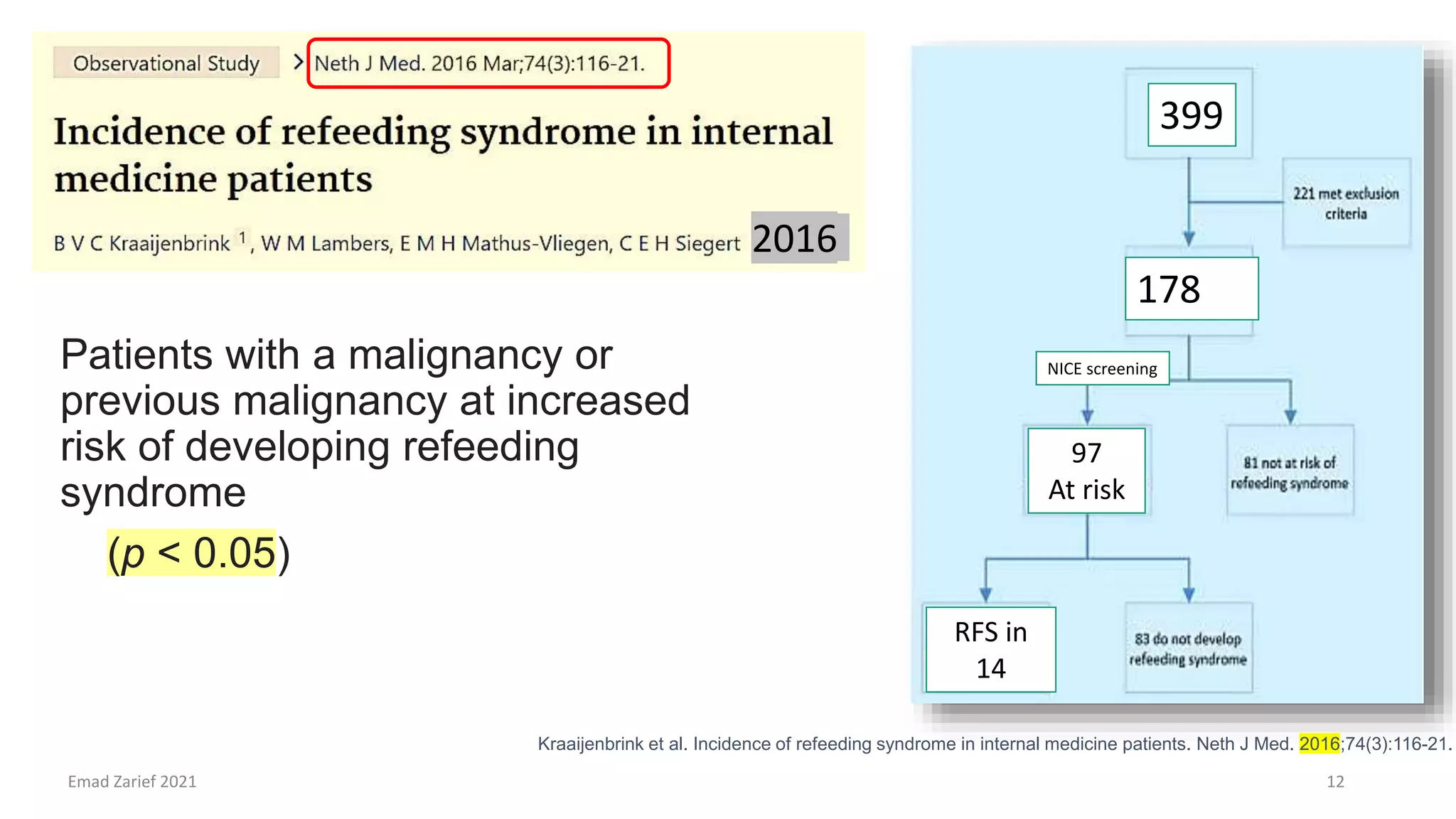
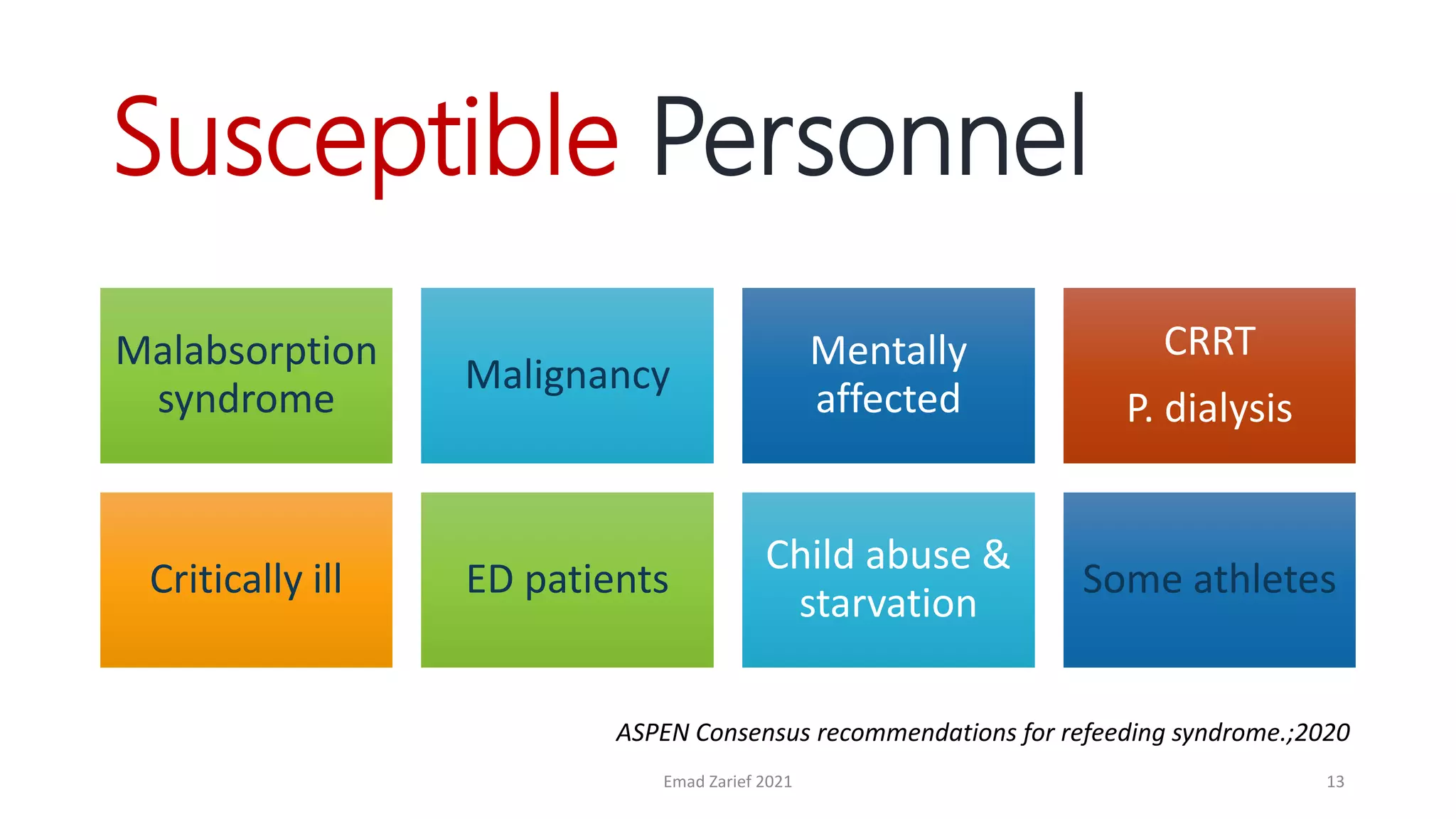
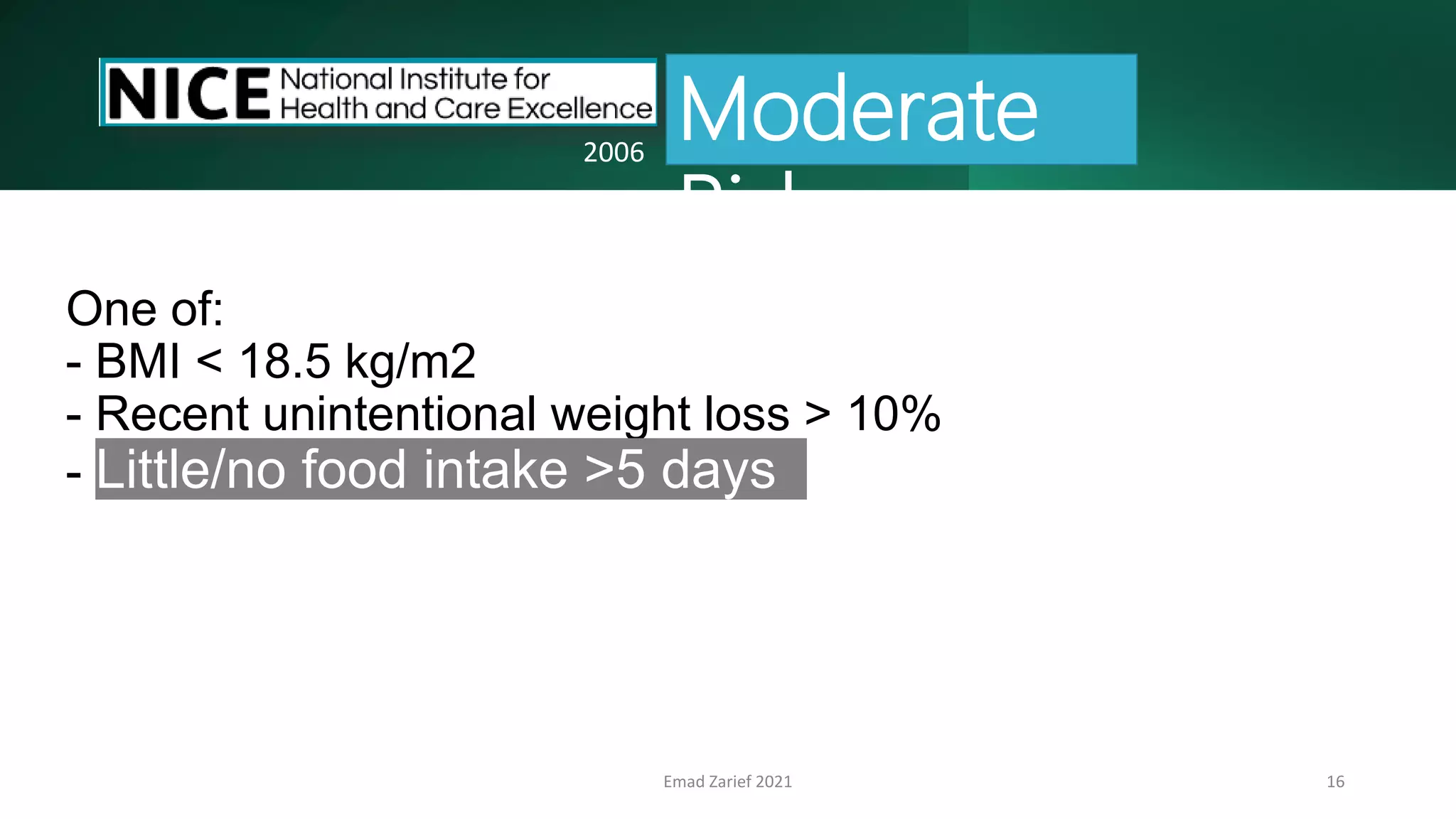
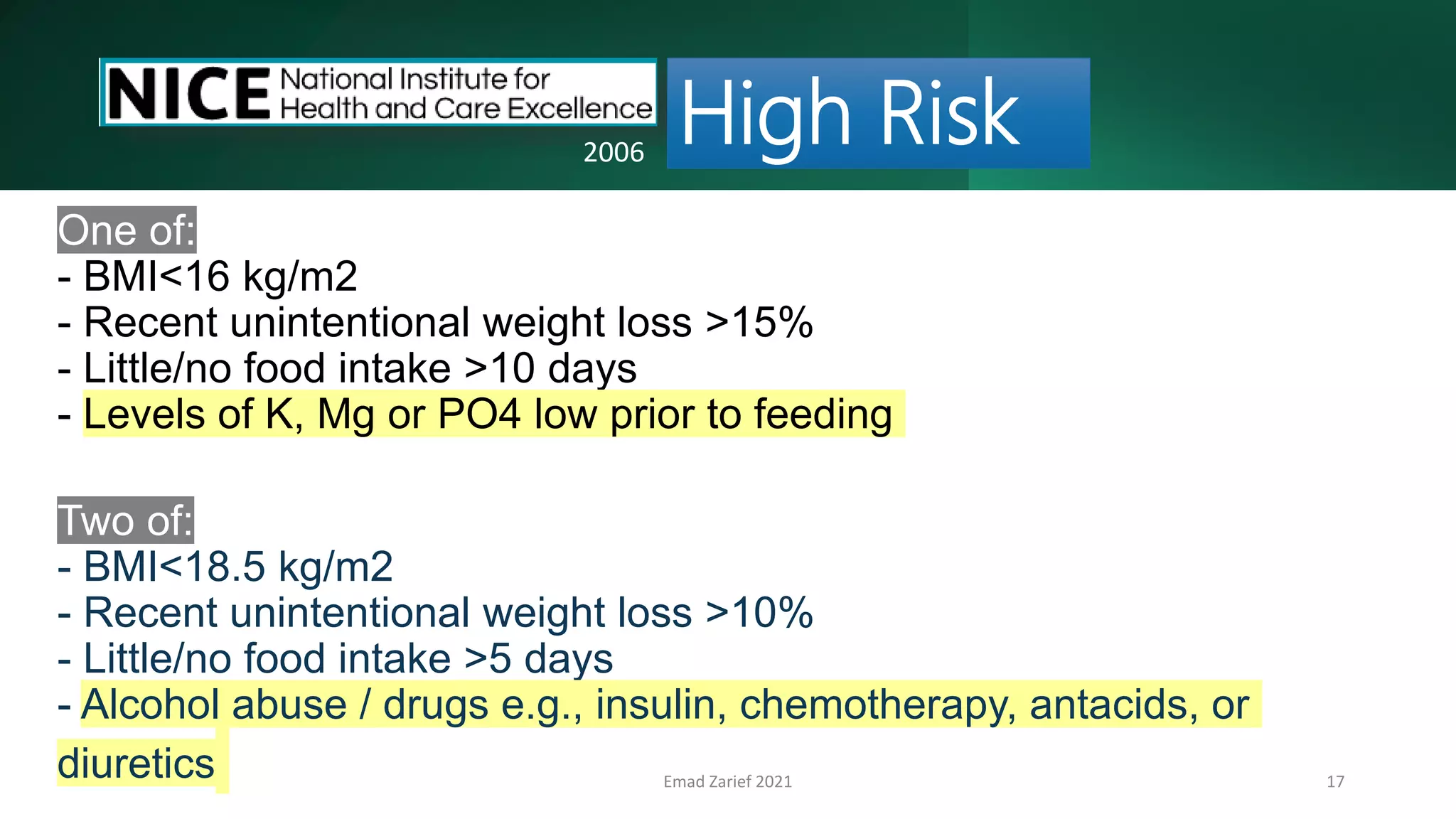
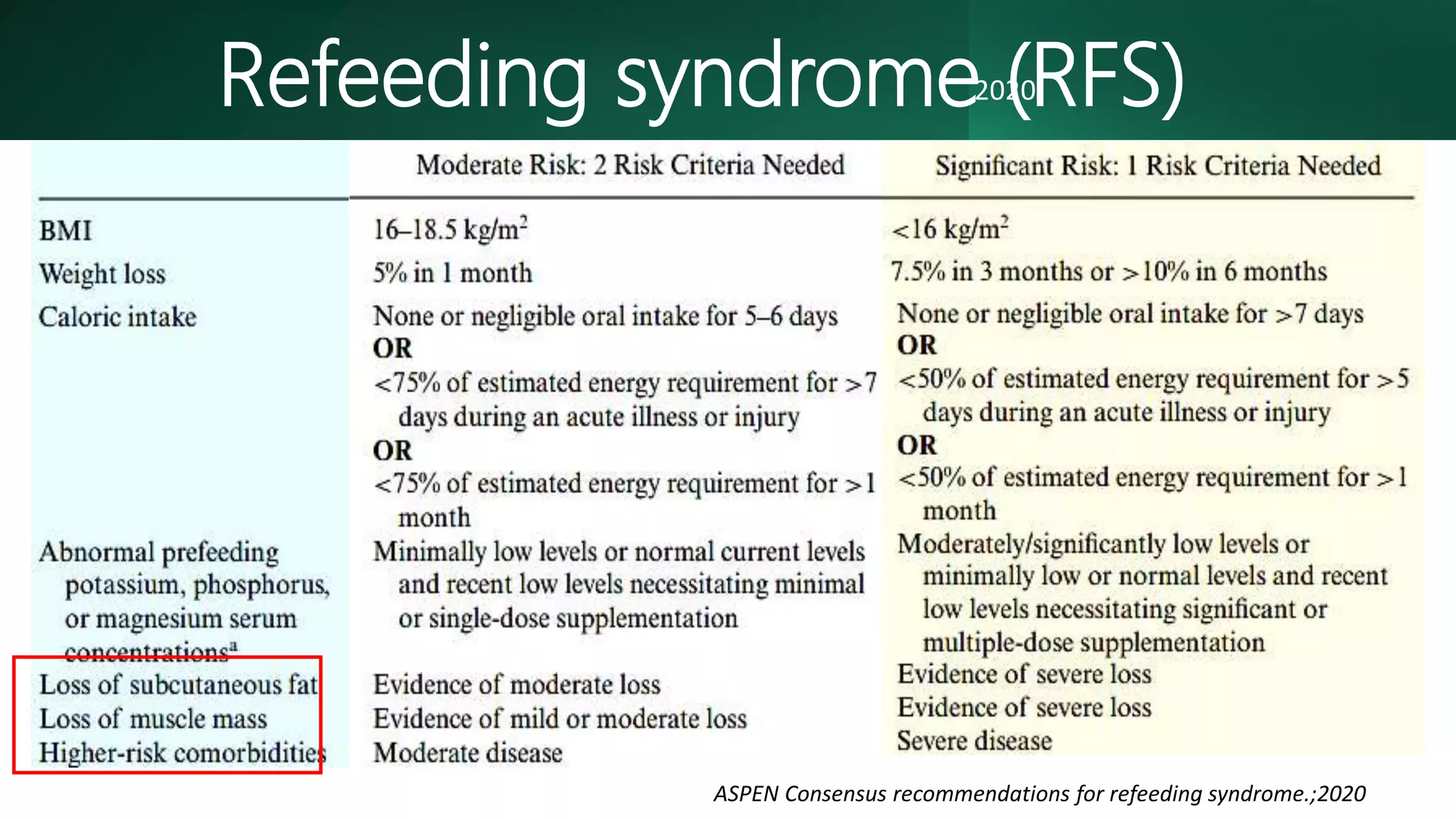
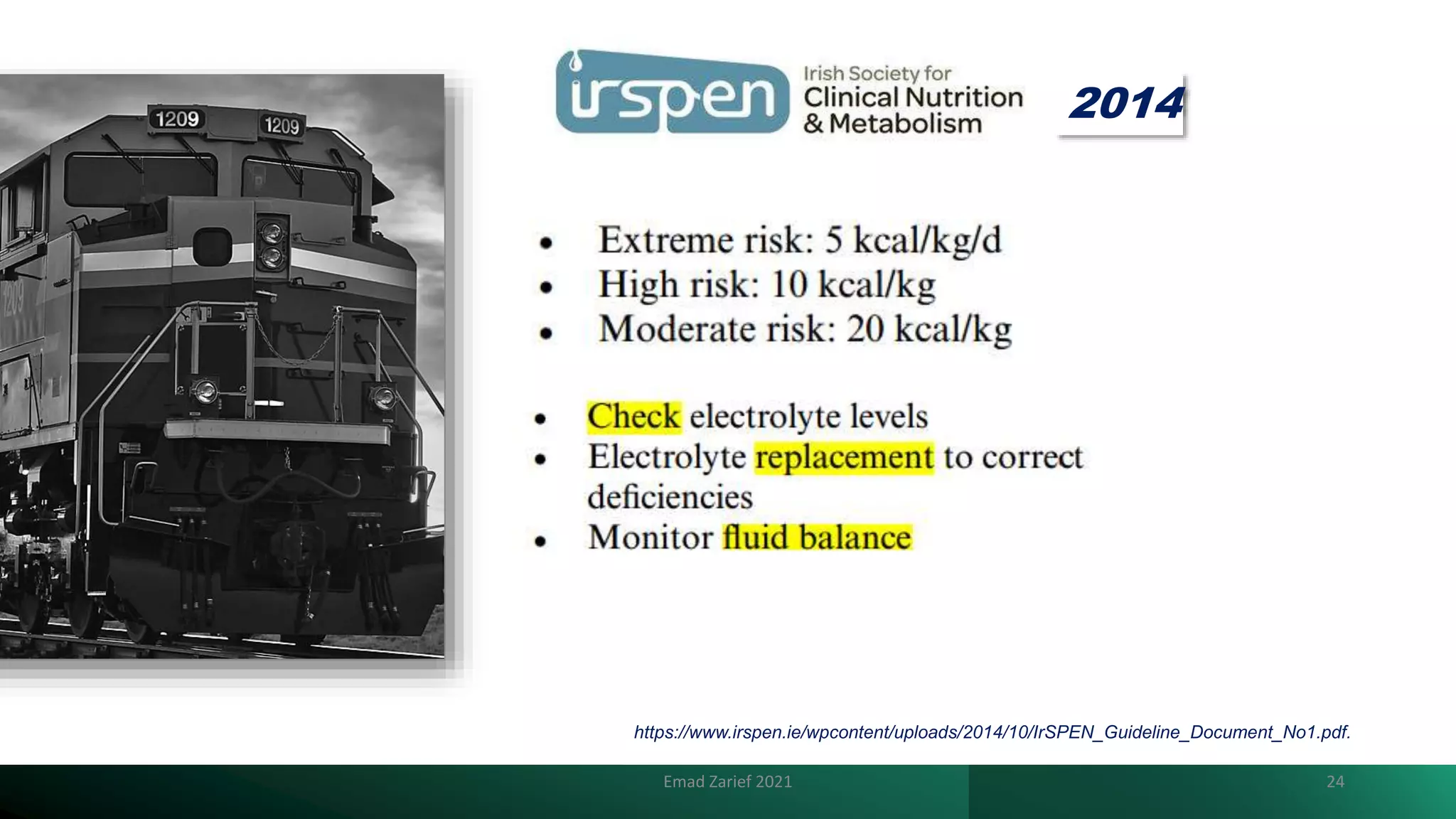
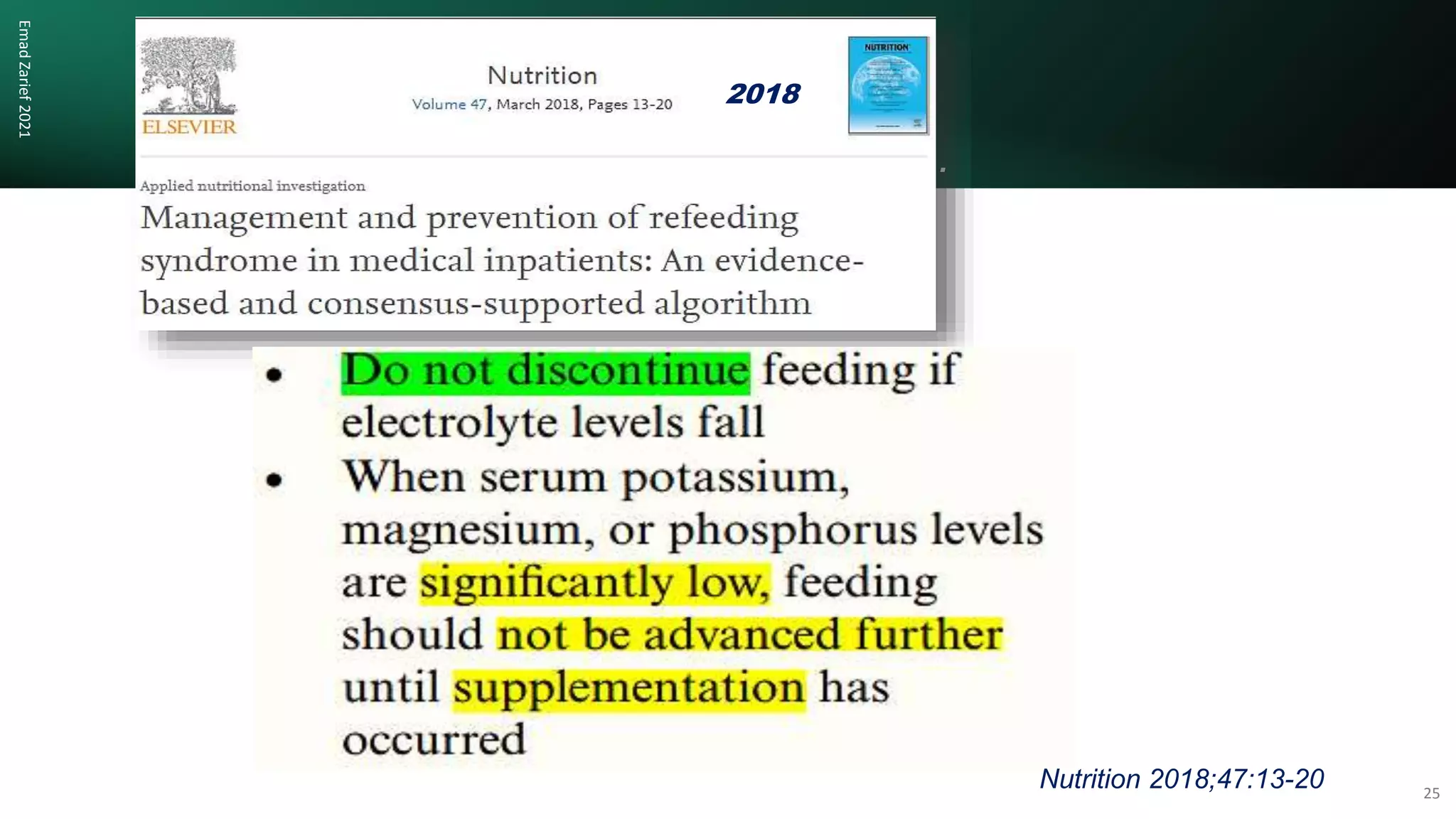
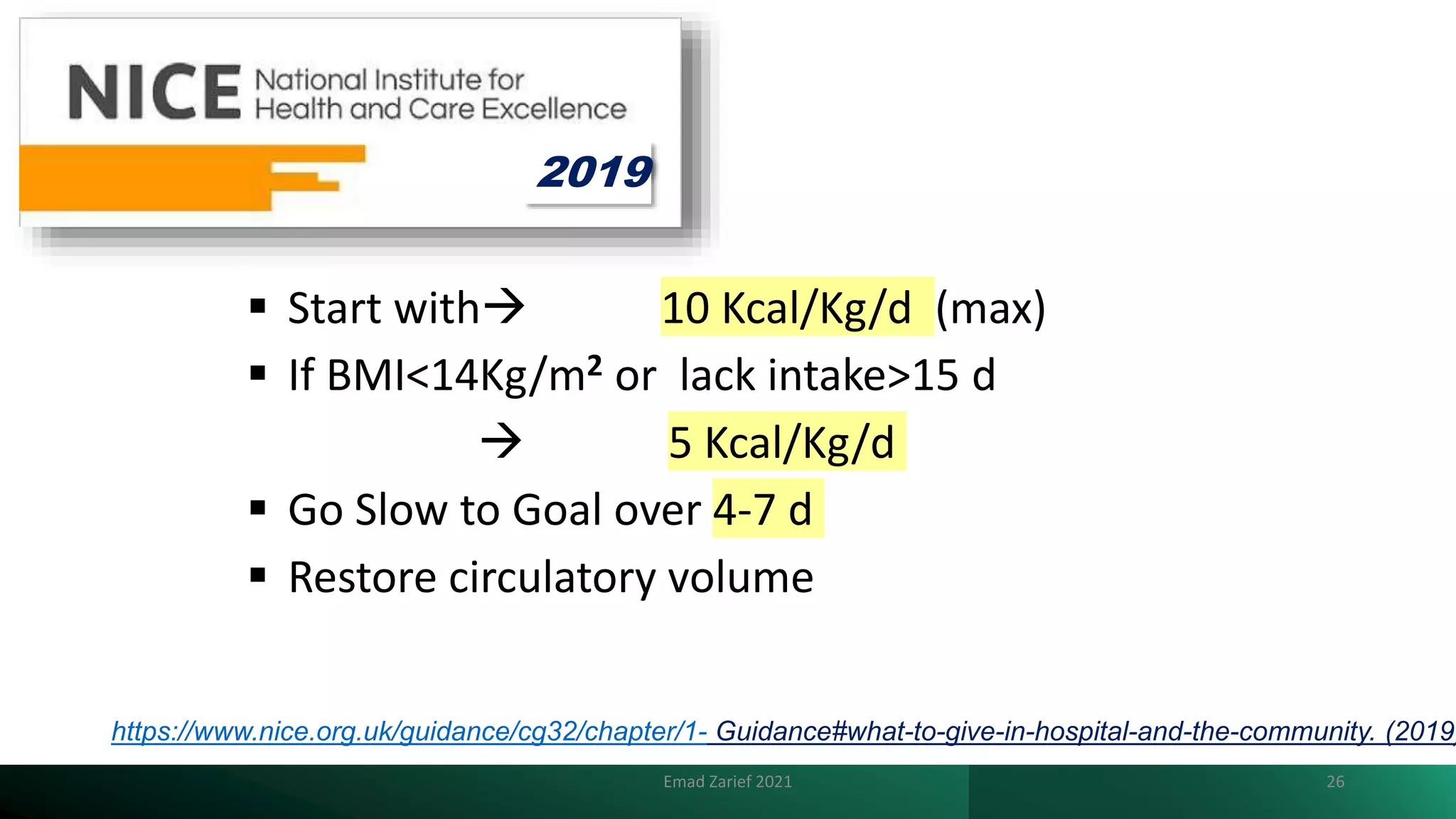
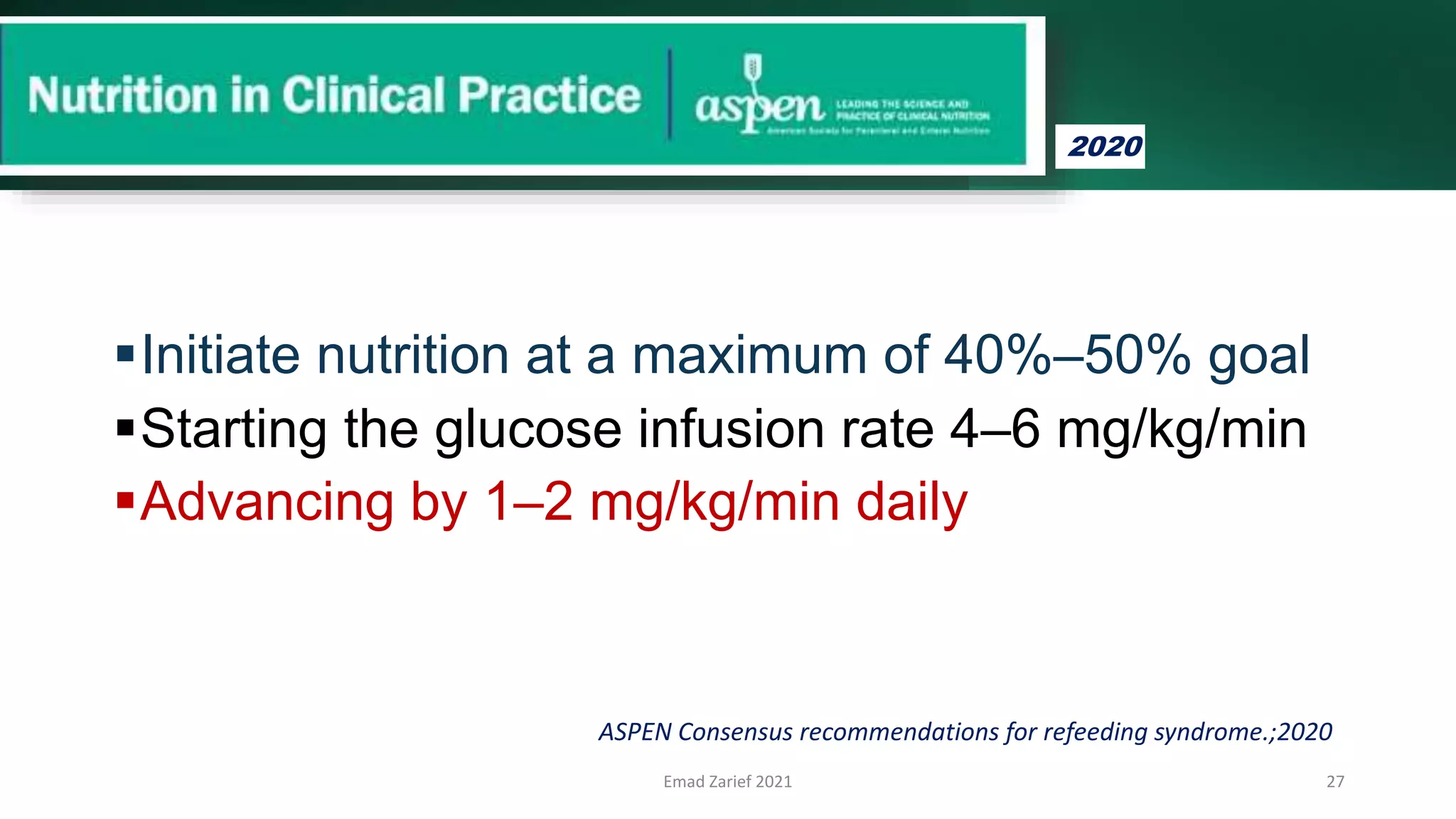
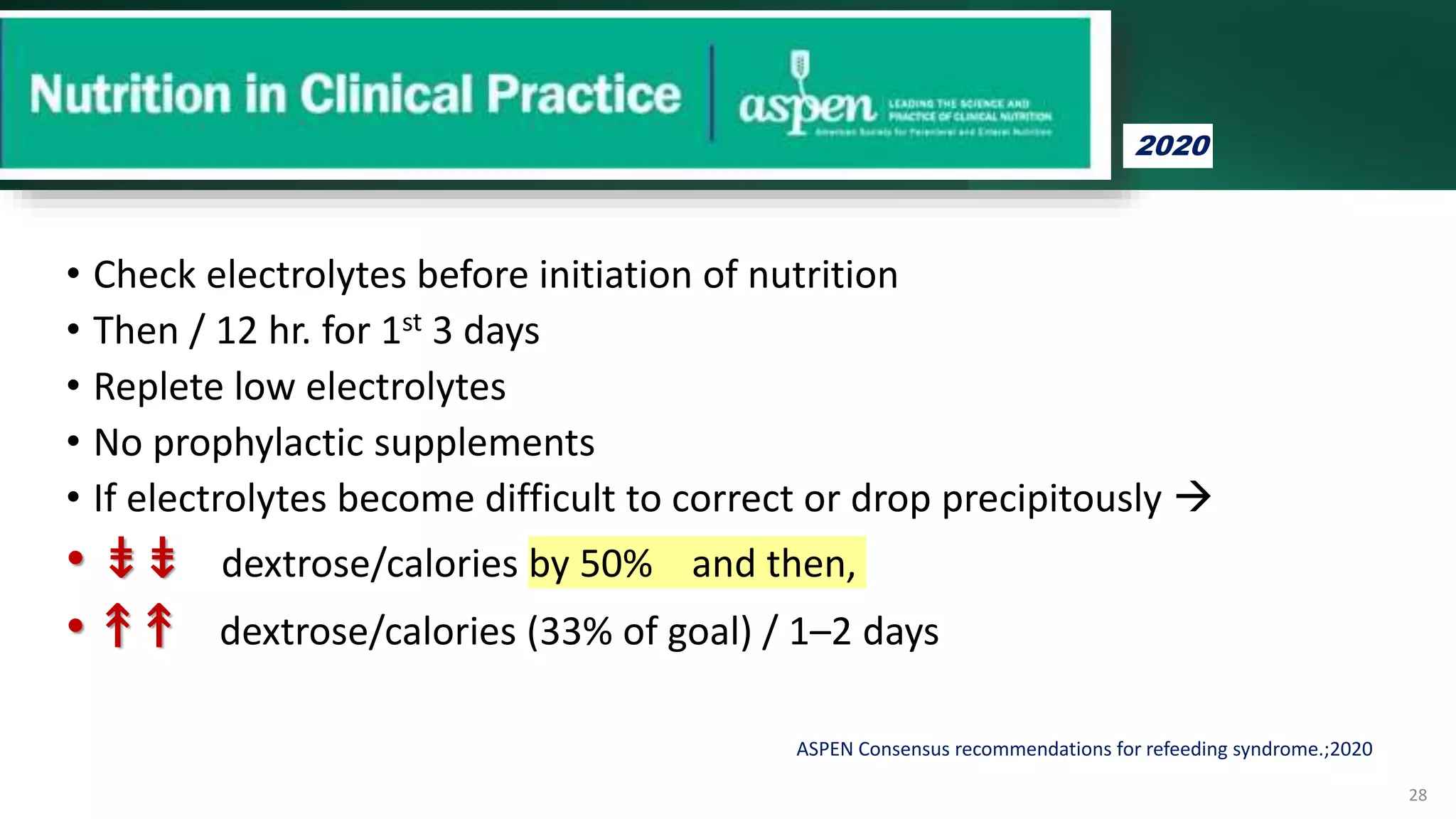
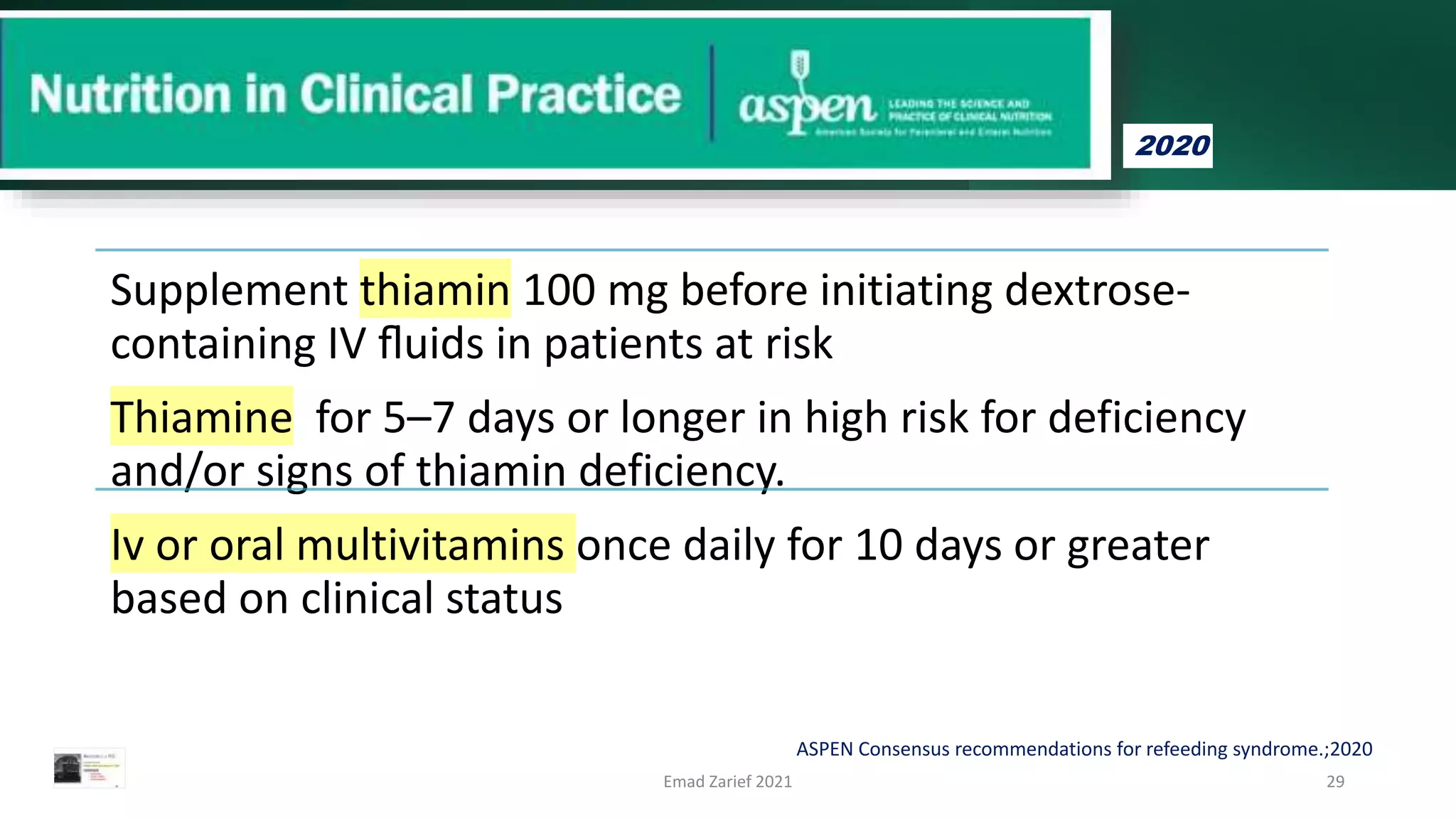
Refeeding syndrome (RFS) is a potentially fatal set of metabolic and electrolyte imbalances that occurs when feeding is restarted in malnourished individuals, highlighted by electrolyte disturbances such as hypophosphatemia. The incidence of RFS is notably high in critically ill patients, especially those with a history of malnutrition or certain risk factors, and proper screening and management are crucial to avoid complications. Recommendations emphasize gradual refeeding, close monitoring of electrolytes, and appropriate supplementation of vitamins like thiamine in high-risk patients.