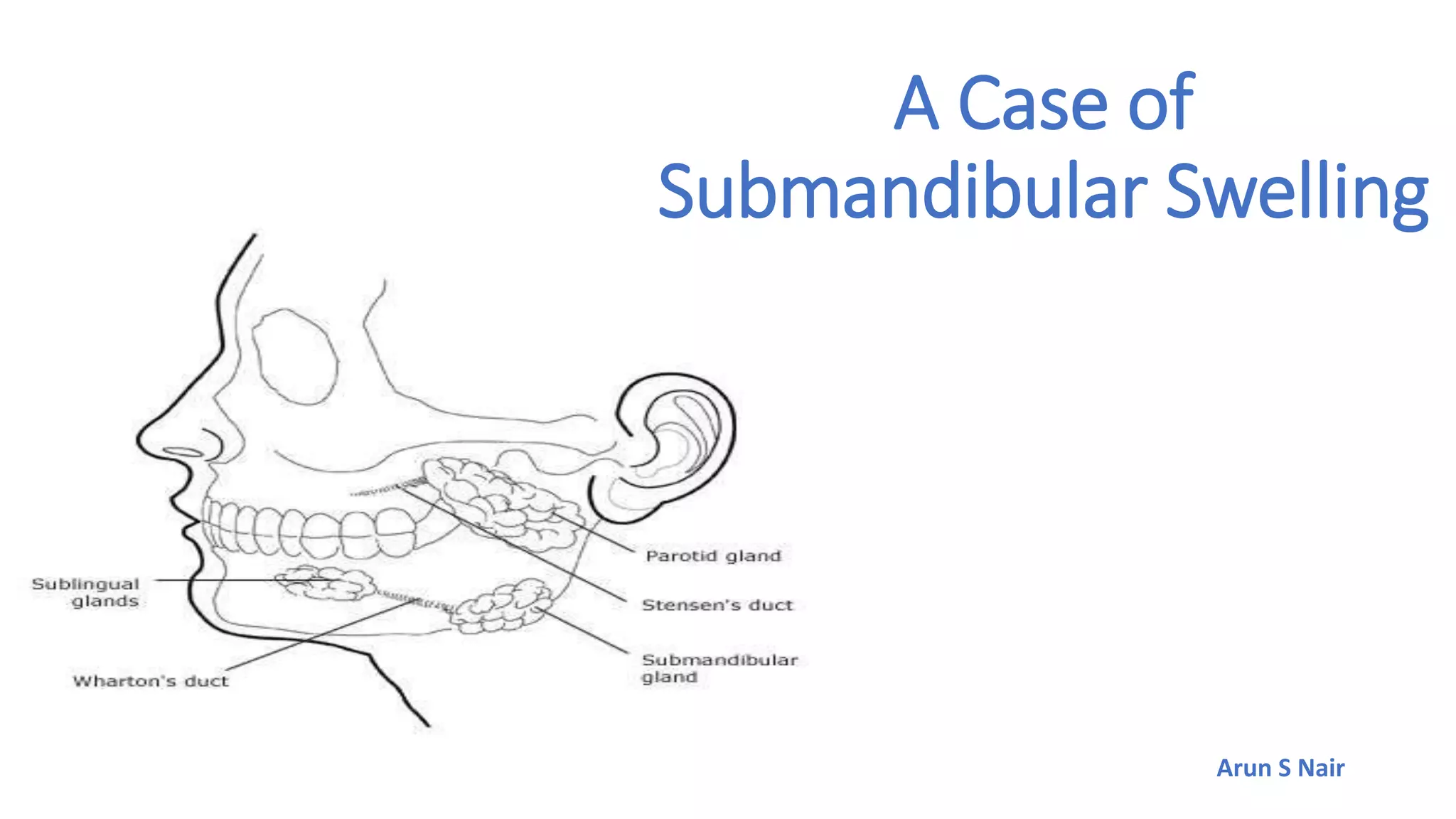
This case report describes a 22-year-old male presenting with a painful swelling in the right submandibular region for 7 days that was aggravated by eating. Clinical examination revealed a sublingual hard mass that was mobile with an irregular surface. Ultrasound showed a sialolithiasis measuring 20 x 8 mm in the right Wharton's duct with secondary sialadenitis of the right submandibular gland. The patient underwent transoral excision of the sialolithiasis and was discharged after recovery with no complications.