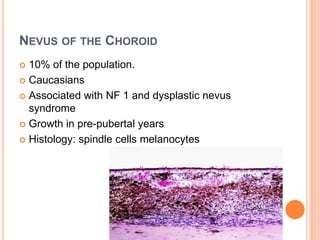
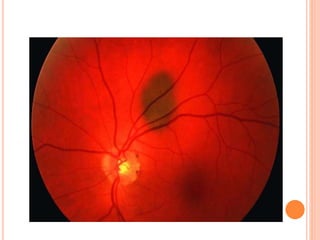
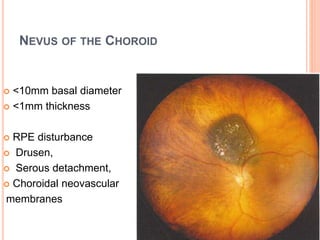
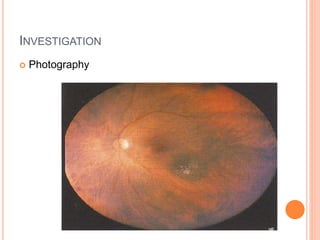
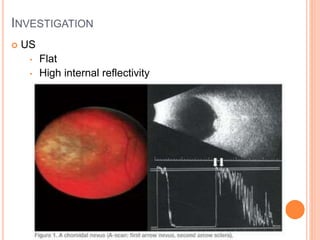
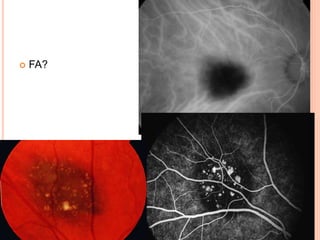
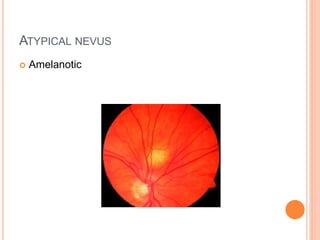
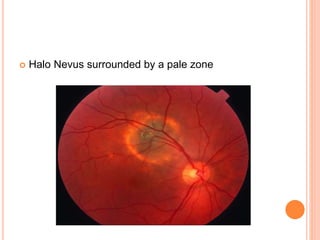
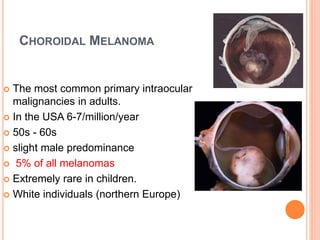
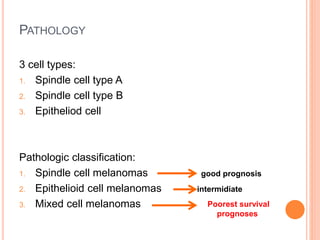
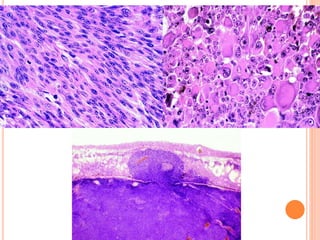
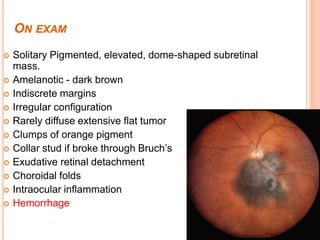
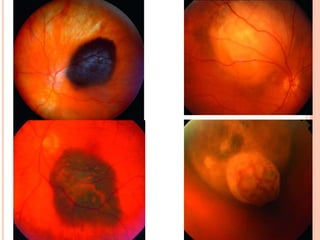
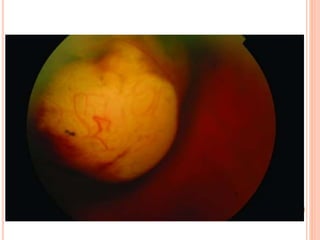
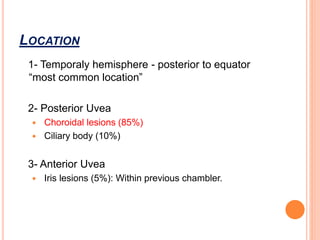
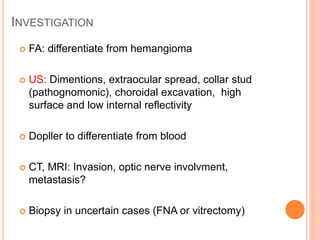
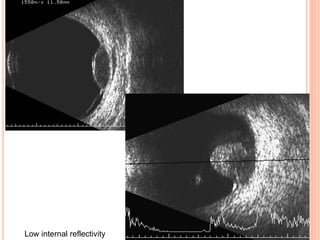
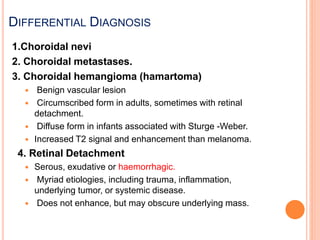
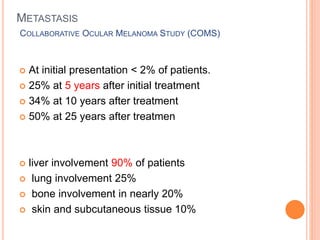
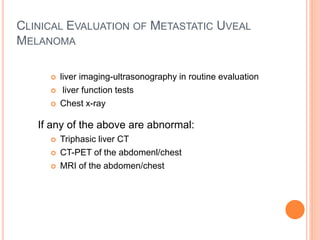
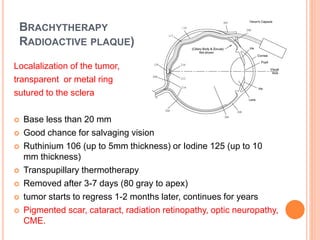
This document discusses choroidal nevus and melanoma. It begins by introducing choroidal melanocytes and describing the differences between benign nevi and malignant melanomas. It then discusses choroidal nevi in more detail, including their prevalence, appearance on examination, investigation methods, and recommended follow up. The document also provides extensive details on choroidal melanoma, including risk factors, pathology, clinical presentation, location, investigation, differential diagnosis, metastasis patterns, treatment options, and prognosis.