Uterine-Fibroids.ppt
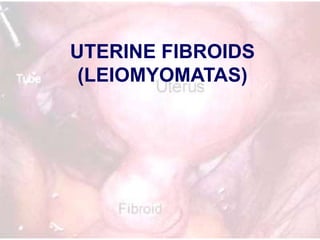
- 2. • Smooth Muscle Tumor of the Uterus • The most common uterine tumor – Occurring in about 30% of women above the age of 30 years. • Occurs up to 75% of hysterectomy specimens • Symptomatic in 1/3 of cases What are they?
- 3. Patient Characteristics • Age: – 30-40 years. – Rare before 30 or after 40 years • Parity: – Common in nulliparas, patients with low parity. – It is rare in multiparas. • Race: – 3-9 times more common in negroids. • Family history: – Usually positive. • Hyper-estrenemia: – Estrogen receptors (ER) more than the surrounding myometrium but less than those in the endometrium • Common in low parity. • Atrophies and shrinks after menopause. • Common association with other hyper-estrenic conditions as endometriosis, endometrial hyperplasia and endometrial carcinoma.
- 4. Fibroids Uterine [99%] Extrauterine [1%] Corporeal [95%] Cervical [4%] Interstitial [60%] Submucous [ 20%] Subserous [15%] Genital Extragenital Parasitic Fibroid Others
- 6. Characteristics • Size – from microscopic to very huge size filling the whole abdominal cavity (up to 40 kg was recorded). • Shape – Spherical, flattened, or pointed according to the type. • Cut section: – On cut section,, whorly in appearance, and more pale than the surrounding uterine muscle. • Consistency: – firmer than the surrounding myometrium. – Soft fibroid occurs in pregnancy, cystic changes, vascular, inflammatory, and malignant changes. – Hard fibroid occurs in calcification. • Capsule: – Is a pseudo-capsule formed by compressed normal surrounding muscle fibres. – the blood supply comes through it, – it is the plain of cleavage during myomectomy – its presence differentiate the myoma from adenomyosis. • Blood supply: – Nourishes the myoma from the periphery, – The tumor itself is relatively avascular.
- 8. Presentations • Asymptomatic: – Accidentally discovered during examination. – It is the commonest presentation, especially in subserous and interstitial fibroids. • Vaginal bleeding: It is the commonest symptom, – Menorrhagia or polymenorrhea: (commonest): This occurs due to: • Associated hormonal imbalance and endometrial hyperplasia. • Surface ulceration of submucous fibroid. • Interstitial fibroid acts as F.B. preventing full contraction of myometrium to decrease blood loss. • Pelvic congestion. • Increased uterine size, vascularity, and endometrial surface area. – Metrorrhagia: due to: • In submucous fibroid due to ulceration of the surface, necrosis of the tip, or secondary infection. • Associated endometrial polyp. • Associated malignancy (cancer body or sarcomatous change). – Contact bleeding: (rare) • ulcerated or infected tip of submucous fibroid polyp. – Post-menopausal bleeding: • Either due to sarcomatous change or associated endometrial carcinoma. • Picture of iron deficiency anemia.
- 9. Presentations • Discharge: – Leucorrhea and mucoid discharge due to pelvic congestion. – Muco-sanguinous discharge with ulcerated fibroid polyp. – Muco-purulent discharge due to secondary infection. • Swelling: – Either abdominal swelling due to large fibroid or vaginal swelling due to a polyp. • Infertility [in 5-10% of cases]: – Most important is the underlying predisposing factor as anovulation and hormonal disturbance. – Broad ligamentary fibroid may stretch or distort the tubes. – Corneal fibroids may obstruct the uterine end of the tube. – S.M.F. acts as F.B. interfering with implantation. – Cervical fibroid may obstruct the cervical canal. – Associated endometriosis or endometrial hyperplasia. • Pain: uncommon – Intermittent colicky pain in submucous fibroid (acts as F.B. in the uterine cavity). – Dull-aching pain and congestive dysmenorrhea due to pelvic congestion. – Acute abdomen in red degeneration, torsion, ruptured vessel, and inflammation.
- 10. Presentations • Pressure symptoms – Cervical fibroid: • Anteriorly on the urethra causing acute retention of urine, or the bladder causing frequency of micturition. • Laterally on the ureters causing colic and back pressure on the kidneys. • Posteriorly on the rectum causing dyskasia, constipation, and sense of incomplete defecation. – Huge fibroid: • On the pelvic veins causing edema, pain, and varicose veins in the lower limbs. • On the GIT causing distension and dyspepsia. • On the diaphragm causing dyspnea. • Spontaneous abortion: – Before myomectomy [ 40%] – 20% after myomectomy.
- 11. Signs of fibroid • General examination: – signs of chronic anemia. • Abdominal examination: – large pelvi-abdominal swelling in huge fibroids. • Pelvic examination: – symmetrically or asymmetrically enlarged uterus. • Speculum examination – fibroid polyp.
- 18. Differential Diagnosis • Causes of symmetrically enlarged uterus: – Pregnancy – Subinvolution of the uterus. – Submucous or interstitial fibroid. – Metropathia hemorrhagica. – Adenomyosis uteri. – Carcinoma or sarcoma of the uterus. – Pyo, hemato, or physometra. • Causes of asymmetrically enlarged uterus: – Subserous fibroid. – Localized adenomyosis. – Ovarian, tubal, or broad ligamentary swelling. – Pregnancy in a rudimentary horn.
- 19. Management • Conservative Management – small asymptomatic fibroid, – fibroid in pregnancy or puerperium. • Just keep observation every 6 months. • Beware of underlying and/or associated pathology
- 20. Medical Treatment: • Pre-operative till the time of surgery. • Patient near the menopause, or newly married with minimal symptoms. • Red degeneration with pregnancy. • Lines of treatment: – Symptomatic: • Correction of anemia, • haemostatics, • analgesics, and anti-spasmodics (anti-PG). – Anti-estrogens: • large dose of progesterone, • Tamoxifen, Danazol, • LH-RH analogues – useful in decreasing the size and vascularity of the tumor by 50% which is beneficial before myomectomy
- 21. Surgical Management Myomectomy vs. Hysterectomy ??!! •Indications: •Symptomatic cases or uterus larger than 12 weeks size. •Suspected malignancy (rapidly enlarging or post-menopausal growth). •Multiple huge fibroids liable to complications. •Infertility.
- 22. Myomectomy • Abdominal Myomectomy • Vaginal Myomectomy • Endoscopic Myomectomy – Hysteroscopic – Laparoscopic • Embolization techniques ( Interventional Radiology)
- 23. Principle •Myomectomy aims at – removal of all the myomas, – with conservation of a functioning uterus to preserve the reproductive function. •Generally the morbidity is higher than those with hysterectomy. – It is associated with much blood loss – Liability of recurrence of fibroid. •Myomectomy is better reserved only for those keen to preserve the reproductive function.
- 24. Principle • The patient must be prepared for the possible need for an emergency hysterectomy. • Precautions to minimize blood loss during myomectomy: – The timing of operation is post-menstrual (minimal pelvic congestion). – Pre-operative LH-RH analogues: may be given for 3 months before surgery to reduce the size and vascularity of the myomas. – Intraoperative hemostasis • Vertical midline incision is the least vascular • application of Bonney’s myomectomy clamp or a rubber tourniquet • Use ring forceps to occlude the ovarian vessels • Careful dissection to enucleate all the masses is needed to avoid recurrence. • Avoid anesthetic agents that induce uterine relaxation (e.g. halothane). • Vasopressin (pitressin) 20 IU in 20 ml in normal saline are injected in the uterine wall at the site of incision. • Obliteration of the tumour cavities. • Buried sutures to the tumor bed after shelling out of the masses. • Use absorbable sutures. • Blood needs to be prepared for possible transfusion
- 25. • Technique of abdominal myomectomy: • Preliminary diagnostic curettage to exclude endometrial carcinoma. • The uterine incision: – Avoid incisions on the posterior uterine wall, for the risk of adhesions to the bowel. – The smallest incision is designed to enable removal of as many lesions as possible. – Tunneling in the uterine wall is utilized to minimize many incisions and peritoneal trauma. – Try to avoid opening the endometrial cavity. • To keep the uterus anteverted – ventrosuspension or plication of the round ligaments and uterosacral ligaments. • Dextran solution, Ringer lactate solution or dexamethazone could be instilled in the peritoneal cavity to minimize postoperative adhesions.
- 26. Vaginal Procedures • Vaginal myomectomy: – Indicated when a fibroid polyp is not larger than 8 weeks pregnancy size. – The polyp is grasped and twisted until the pedicle tears. – If the pedicle is too thick it is cut with scissors. – A large polyp could be cut as piece-meal fashion (morcellation).
- 29. Hysterectomy • Patient around 40 years, and completed her family. • The number or site contraindicate myomectomy • Severe bleeding during myomectomy. • Major damage of the uterus by myomectomy which affects its function for pregnancy. • Recurrent fibroids. • Suspicious of malignancy
- 31. Embolization
- 33. Secondary Changes in Fibroids • Degenerative • Vascular • Inflammatory • Malignant Changes
- 34. Degenerative Changes • Hyaline degeneration: – Commonest secondary change. – Usually starts around the menopause, and in the center of the fibroid. – Macroscopically, fibroid looks homogenous, waxy, soft, with loss of whorly appearance. • Fatty changes: – Likely to start around the age of menopause. – Lipids reach the fibroid through the blood, so fatty change starts at the periphery of the fibroid, resulting in a yellow soft fibroid.
- 35. • Calcification: – Step following fatty change when fatty acids undergo saponification with Ca salts giving Ca stearate and palmitate, forming layers of calcifications. – Clinically, the fibroid become hard like bone (Womb stone). – Radiologically, show a radio-opaque shadow with typical onion skin appearance. • Red degeneration (Necrobiosis): – Usually occurs in the middle trimester of pregnancy, due to increased vascularity and venous stasis, the tumor enlarges with hemorrhage inside the tumor. – It is called necrobiosis because it shows dead parts (central) and living parts (peripheral).
- 37. • Atrophic changes: – Atrophy occurs due to estrogen withdrawal as after menopause, puerperium, or anti-estrogen use. – All myomas decrease in size after the menopause except in calcification it remains stationary, or with malignant change or HRT it increases in size. • Myxomatous change: – Occurs near the menopause, in the center of the myoma, forming a gelatinous mucoid material which may undergo pseudo-cystic changes. • Pseudo-cystic changes: – A step following hyaline or myxomatous changes, when it liquefies & becomes soft in consistency.
- 38. Vascular Changes • Torsion (Axial rotation): –Occurs in moderate-sized, pedunculated, subserous fibroid with no adhesions. –The precipitating factor is sudden twisting movement as trauma, intestinal movement, or fetal kick, leading to axial rotation which is prevented from re- twisting by the lashing effect of the pulsating pedicle. –The clinical effects depend on the onset of torsion: • Sudden torsion leads to acute abdomen and necrosis of the tumor. • Gradual torsion leads to gradual decrease of the blood supply from the pedicle which ends in the development of parasitic tumor. • Telangeactasis: –Likely to occur with pregnancy, malignant change, and cervical fibroid due to increased vascularity. –There are numerous dilated blood vessels on the surface of the fibroid which may rupture leading to acute abdomen and internal hemorrhage. • Lymphangeactasis: –Likely to occur around the age of menopause as the fibroid is full of lymphatics. –Dilated lymphatic vessels on the surface may rupture leading to lymphatic exudates and strong adhesions. • Congestion and edema: A result of impaction, incarceration, torsion, infection, or pregnancy
- 39. Inflammatory changes • Ways of infection: – Trauma of submucous fibroid e.g. D & C or labor. – Near by inflammation e.g. appendicitis. – Blood-borne (very rare). • Result of infection: – The fibroid becomes congested, tender, and even abscess formation; it becomes soft and heals by adhesions to the surrounding
- 40. Malignant changes • Rare (0.5%) into leiomyosarcoma (round, spindle, mixed or giant cell histopathology types). • Symptoms suggestive: – The fibroid becomes more painful. – Post-menopausal bleeding or growth of the tumor. • Signs suggestive: – The fibroid become softer, tender, or fixed. – Rapid growth of the tumor.
- 41. Hyaline degeneration & Leiomyosarcoma
- 42. Complications of fibroid • Degenerative changes. • Vascular changes. • Inflammatory changes. • Malignant changes. • Pregnancy complications e.g. abortion, and preterm labor. • Pressure complications on the urethra, bladder, ureters, rectum, and pelvic veins. • Rarely, chronic inversion of the uterus. • Polycythemia and hypertension due to the release of erythropoietic agent. • Infertility. • Secondary parasitic attachment of fibromyomas to other abdominal structures gaining another blood supply.
- 43. What is the effect of Fibroid on Pregnancy and Pregnancy on Fibroid?