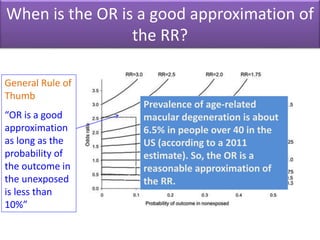
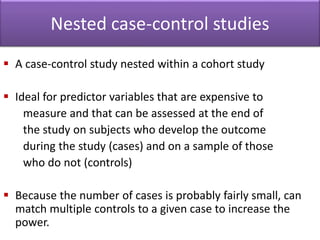
This document discusses different types of observational study designs used in epidemiology, including descriptive and analytical studies. Descriptive studies like case reports and case series describe characteristics of patients but cannot determine causation. Analytical observational studies include cross-sectional studies, which measure exposures and outcomes at one time point, and cohort studies, which follow groups over time. Case-control studies sample based on outcome and look back at exposures. While observational studies are useful for hypothesis generation, experimental randomized controlled trials are needed to prove causation. The odds ratio from case-control studies approximates the risk ratio when studying rare diseases or outcomes.