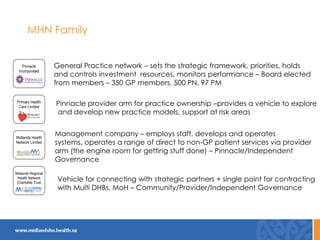
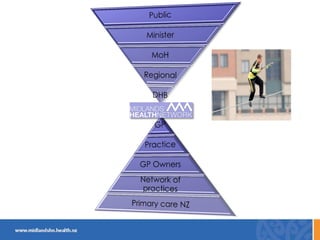
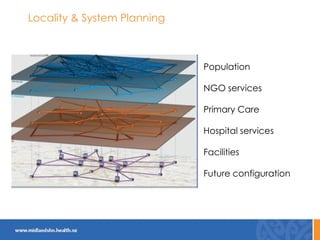
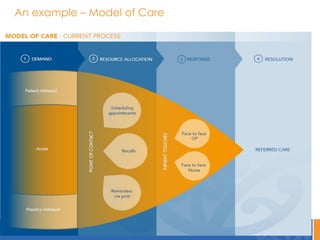
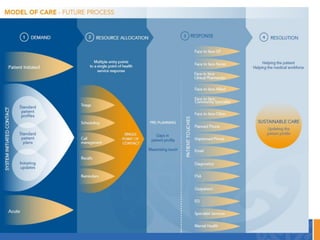
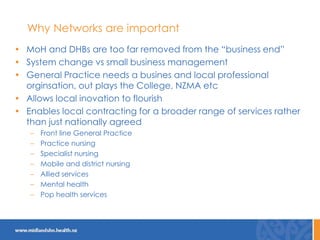
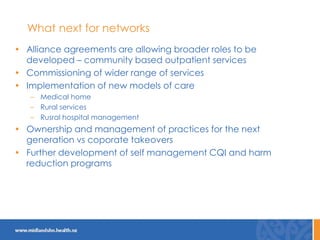
This document discusses the New Zealand health system and primary care networks. It provides an overview of the NZ health system, noting challenges around costs, an aging population, and fragmentation. It then describes primary care networks, how they have organically grown from small practices to networks of hundreds of practices serving over 500,000 patients. The networks aim to improve quality, reduce isolation, and facilitate collective bargaining. They operate across a spectrum from advocacy to community service delivery and quality improvement. The document concludes by discussing the importance of networks and potential future roles around new models of care, broader services, and practice ownership.