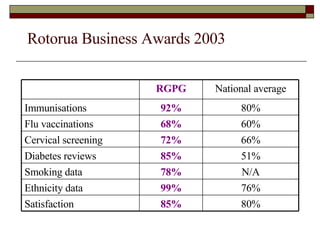
1) The Rotorua General Practice Group Practice (RGPG) in New Zealand successfully implemented electronic health records (EHR) in general practices due to good software, connectivity between systems, and an early adopter culture.
2) RGPG developed their information capacity over time by upgrading hardware, cabling, software, and providing training. This allowed for secure connectivity between practices and supported quality initiatives.
3) Clinical governance requires creating an environment where excellence can flourish through relationships, leadership, and appropriate use of people, processes, and technology. Top-down prescription stifles innovation while empowering local ownership and high trust relationships enables improvement.