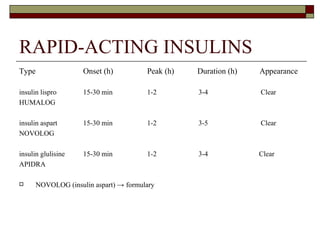
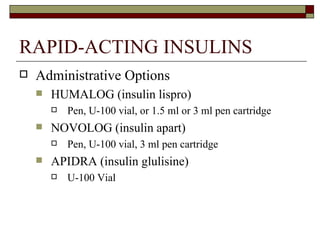
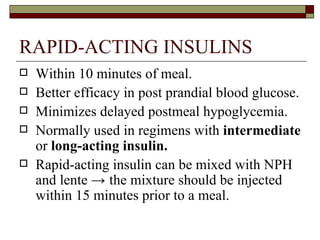
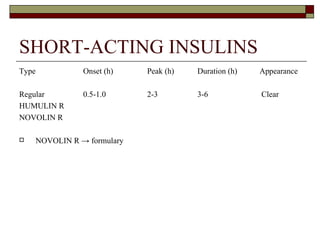
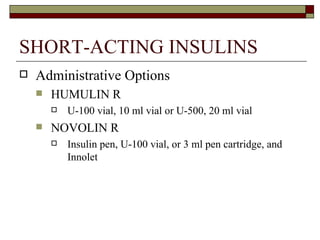
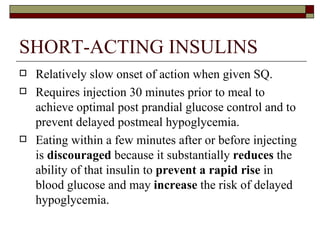
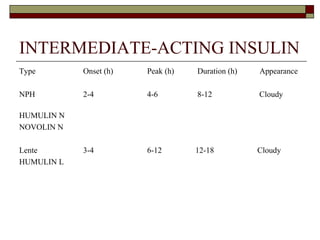
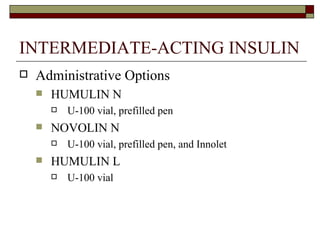
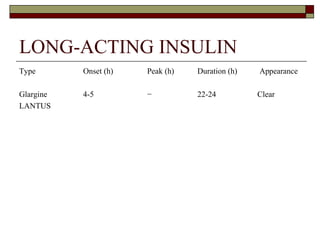
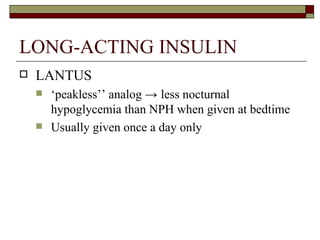
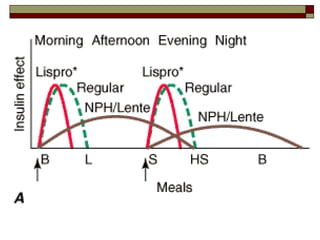
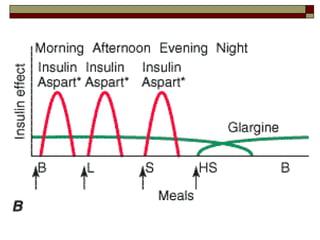
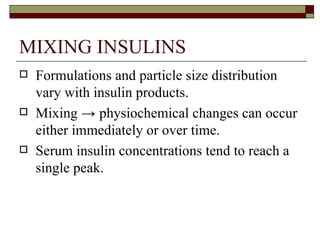
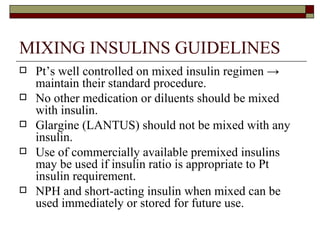
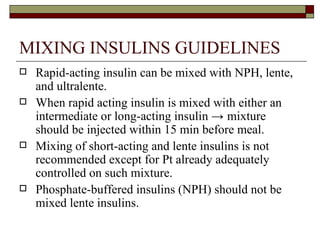
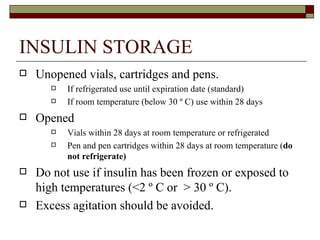
Insulin is used to treat diabetes by regulating blood sugar levels. There are various types of insulin differentiated by their onset, peak time and duration of effect. Rapid-acting insulins work within 15 minutes, short-acting within 30 minutes to 1 hour, intermediate within 2-4 hours and long-acting up to 24 hours. Proper administration and storage of insulin is required to ensure safety and efficacy.