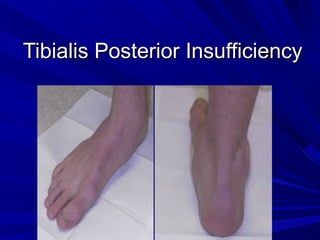
Tibialis posterior insufficiency
•Download as PPT, PDF•
17 likes•5,610 views
Report
Share
Report
Share
More Related Content
What's hot (20)
Superior Shoulder Suspensory Complex injuries (SSSC)

Superior Shoulder Suspensory Complex injuries (SSSC)
Viewers also liked
Viewers also liked (20)
Neutral and Relaxed Stance X-ray Positioning for TaloTarsal Joint Dislocation

Neutral and Relaxed Stance X-ray Positioning for TaloTarsal Joint Dislocation
Similar to Tibialis posterior insufficiency
Similar to Tibialis posterior insufficiency (20)
orthopedic and rheumatologic disorders of the knee joint

orthopedic and rheumatologic disorders of the knee joint
The effect of intact fibula on functional outcome of reamed intramedullary in...

The effect of intact fibula on functional outcome of reamed intramedullary in...
Orthopedics 5th year, 9th lecture (Dr. Ali A.Nabi)

Orthopedics 5th year, 9th lecture (Dr. Ali A.Nabi)
More from Jayant Sharma
More from Jayant Sharma (12)
Fracture proximal humerus Fixation with K wires and External fixator

Fracture proximal humerus Fixation with K wires and External fixator
Recently uploaded
Recently uploaded (20)
💰Call Girl In Bangalore☎️7304373326💰 Call Girl service in Bangalore☎️Bangalor...

💰Call Girl In Bangalore☎️7304373326💰 Call Girl service in Bangalore☎️Bangalor...
Premium Call Girls Dehradun {8854095900} ❤️VVIP ANJU Call Girls in Dehradun U...

Premium Call Girls Dehradun {8854095900} ❤️VVIP ANJU Call Girls in Dehradun U...
Premium Call Girls Nagpur {9xx000xx09} ❤️VVIP POOJA Call Girls in Nagpur Maha...

Premium Call Girls Nagpur {9xx000xx09} ❤️VVIP POOJA Call Girls in Nagpur Maha...
7 steps How to prevent Thalassemia : Dr Sharda Jain & Vandana Gupta

7 steps How to prevent Thalassemia : Dr Sharda Jain & Vandana Gupta
❤️Call Girl Service In Chandigarh☎️9814379184☎️ Call Girl in Chandigarh☎️ Cha...

❤️Call Girl Service In Chandigarh☎️9814379184☎️ Call Girl in Chandigarh☎️ Cha...
Call Girls Bangalore - 450+ Call Girl Cash Payment 💯Call Us 🔝 6378878445 🔝 💃 ...

Call Girls Bangalore - 450+ Call Girl Cash Payment 💯Call Us 🔝 6378878445 🔝 💃 ...
ANATOMY AND PHYSIOLOGY OF REPRODUCTIVE SYSTEM.pptx

ANATOMY AND PHYSIOLOGY OF REPRODUCTIVE SYSTEM.pptx
Cardiac Output, Venous Return, and Their Regulation

Cardiac Output, Venous Return, and Their Regulation
Call Girls Rishikesh Just Call 9667172968 Top Class Call Girl Service Available

Call Girls Rishikesh Just Call 9667172968 Top Class Call Girl Service Available
Chandigarh Call Girls Service ❤️🍑 9809698092 👄🫦Independent Escort Service Cha...

Chandigarh Call Girls Service ❤️🍑 9809698092 👄🫦Independent Escort Service Cha...
Exclusive Call Girls Bangalore {7304373326} ❤️VVIP POOJA Call Girls in Bangal...

Exclusive Call Girls Bangalore {7304373326} ❤️VVIP POOJA Call Girls in Bangal...
Call Girl in Chennai | Whatsapp No 📞 7427069034 📞 VIP Escorts Service Availab...

Call Girl in Chennai | Whatsapp No 📞 7427069034 📞 VIP Escorts Service Availab...
💚Reliable Call Girls Chandigarh 💯Niamh 📲🔝8868886958🔝Call Girl In Chandigarh N...

💚Reliable Call Girls Chandigarh 💯Niamh 📲🔝8868886958🔝Call Girl In Chandigarh N...
Kolkata Call Girls Shobhabazar 💯Call Us 🔝 8005736733 🔝 💃 Top Class Call Gir...

Kolkata Call Girls Shobhabazar 💯Call Us 🔝 8005736733 🔝 💃 Top Class Call Gir...
Dehradun Call Girls Service {8854095900} ❤️VVIP ROCKY Call Girl in Dehradun U...

Dehradun Call Girls Service {8854095900} ❤️VVIP ROCKY Call Girl in Dehradun U...
Cheap Rate Call Girls Bangalore {9179660964} ❤️VVIP BEBO Call Girls in Bangal...

Cheap Rate Call Girls Bangalore {9179660964} ❤️VVIP BEBO Call Girls in Bangal...
💚Call Girls In Amritsar 💯Anvi 📲🔝8725944379🔝Amritsar Call Girl No💰Advance Cash...

💚Call Girls In Amritsar 💯Anvi 📲🔝8725944379🔝Amritsar Call Girl No💰Advance Cash...
Chennai ❣️ Call Girl 6378878445 Call Girls in Chennai Escort service book now

Chennai ❣️ Call Girl 6378878445 Call Girls in Chennai Escort service book now
Tibialis posterior insufficiency
- 11. Too Many Toes Sign
- 12. Single limb heel raise
- 20. Medial Displacement Calcaneal Osteotomy
