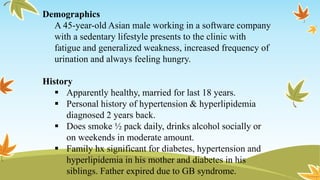
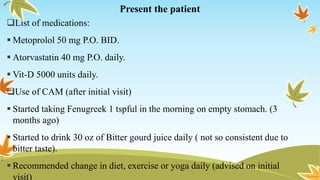
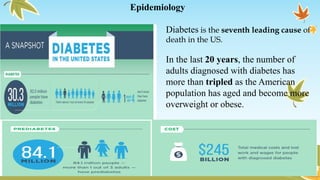
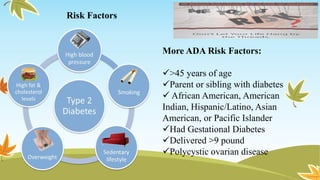
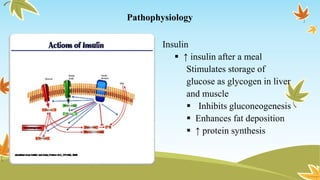
This document presents a case study of a 45-year-old Asian male diagnosed with type 2 diabetes mellitus. It discusses the epidemiology, pathophysiology, risk factors, signs and symptoms, diagnostics, and therapeutic interventions for diabetes. It also provides details of the patient's history, medications, physical exam findings, assessment, and treatment plan. The patient was started on metformin and lifestyle changes including diet, exercise, and quitting smoking. Herbal supplements like fenugreek and bitter gourd juice were also recommended. The goal is to control his blood glucose and prevent diabetes complications through proper management.