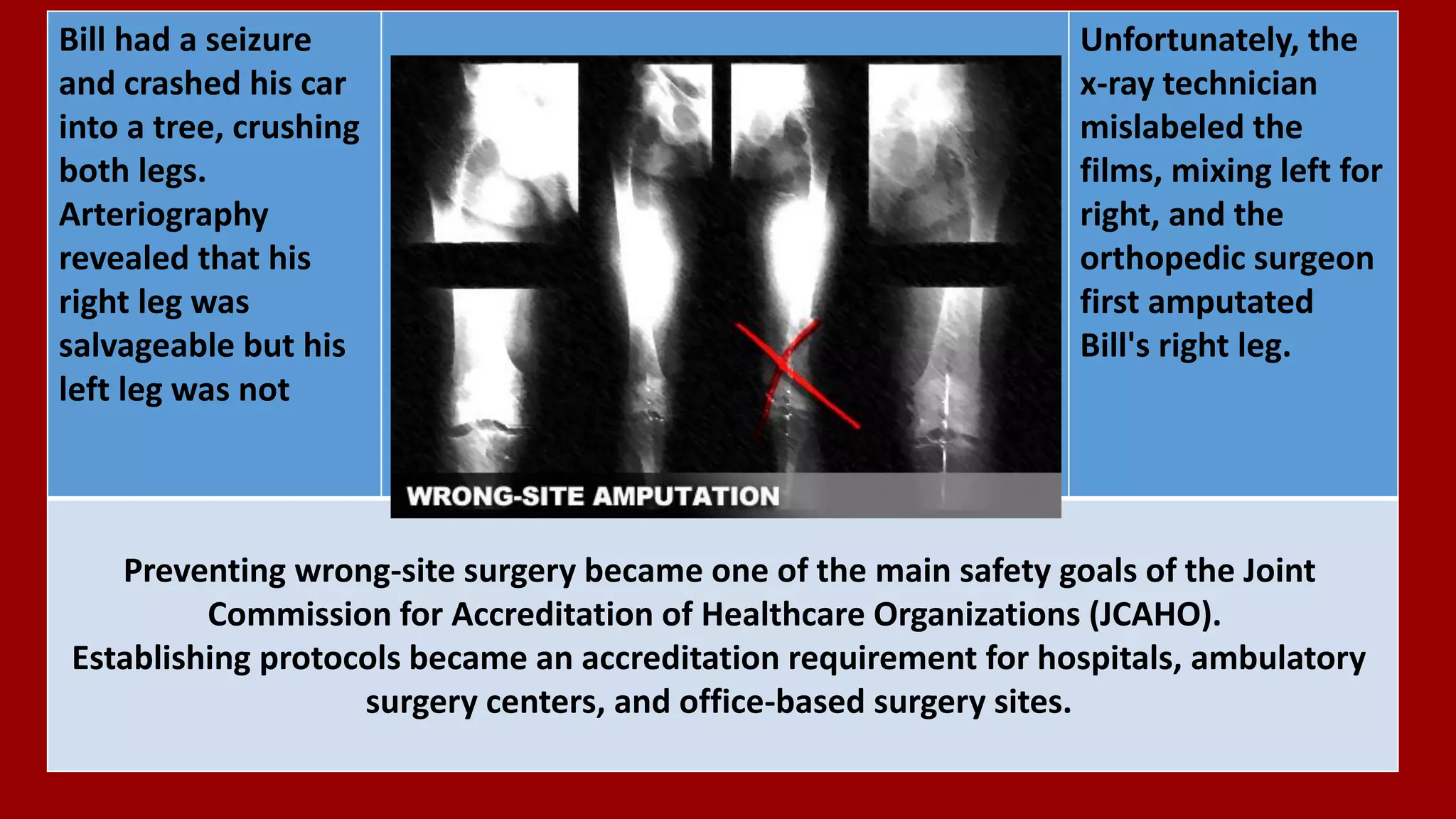
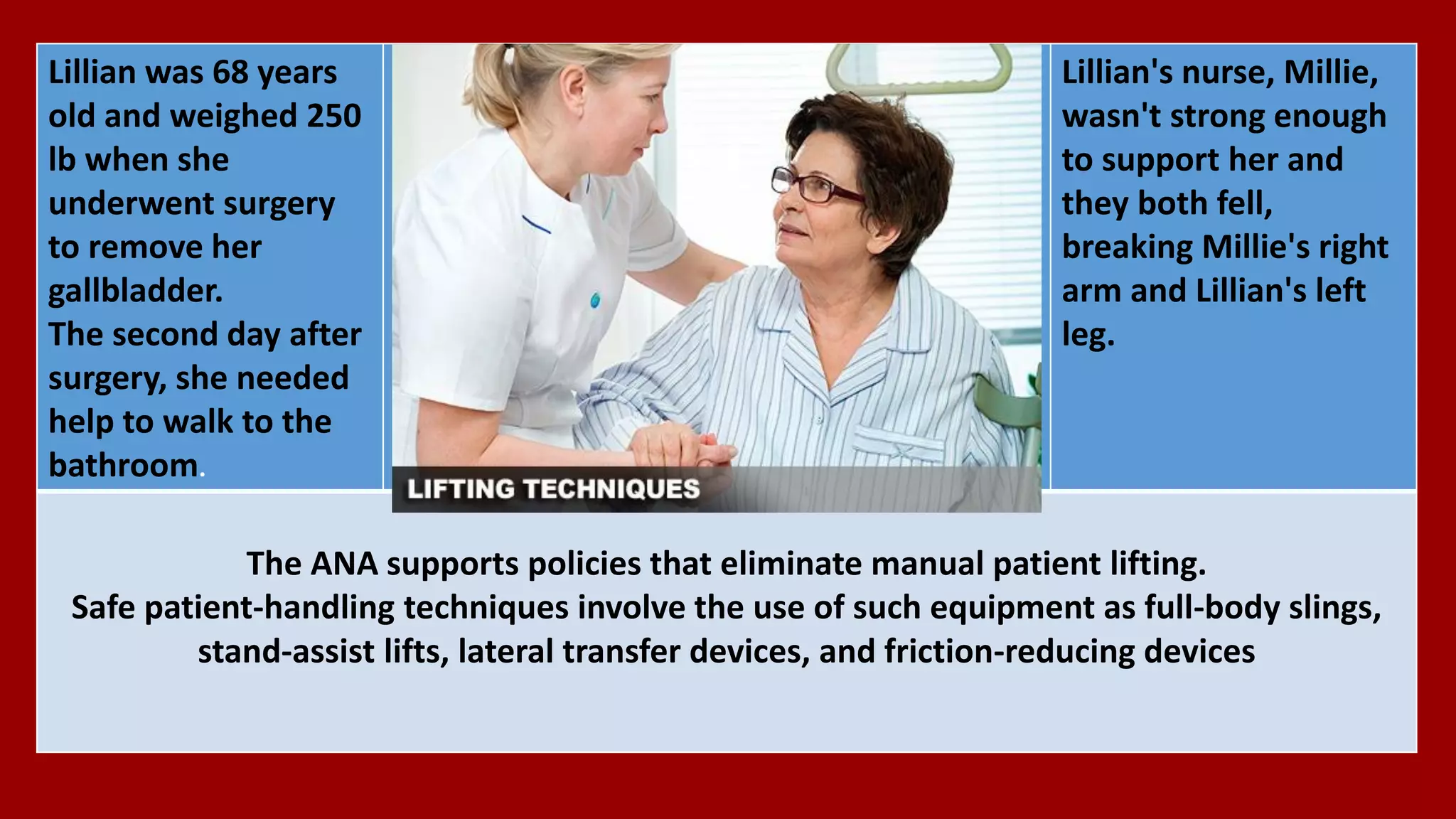
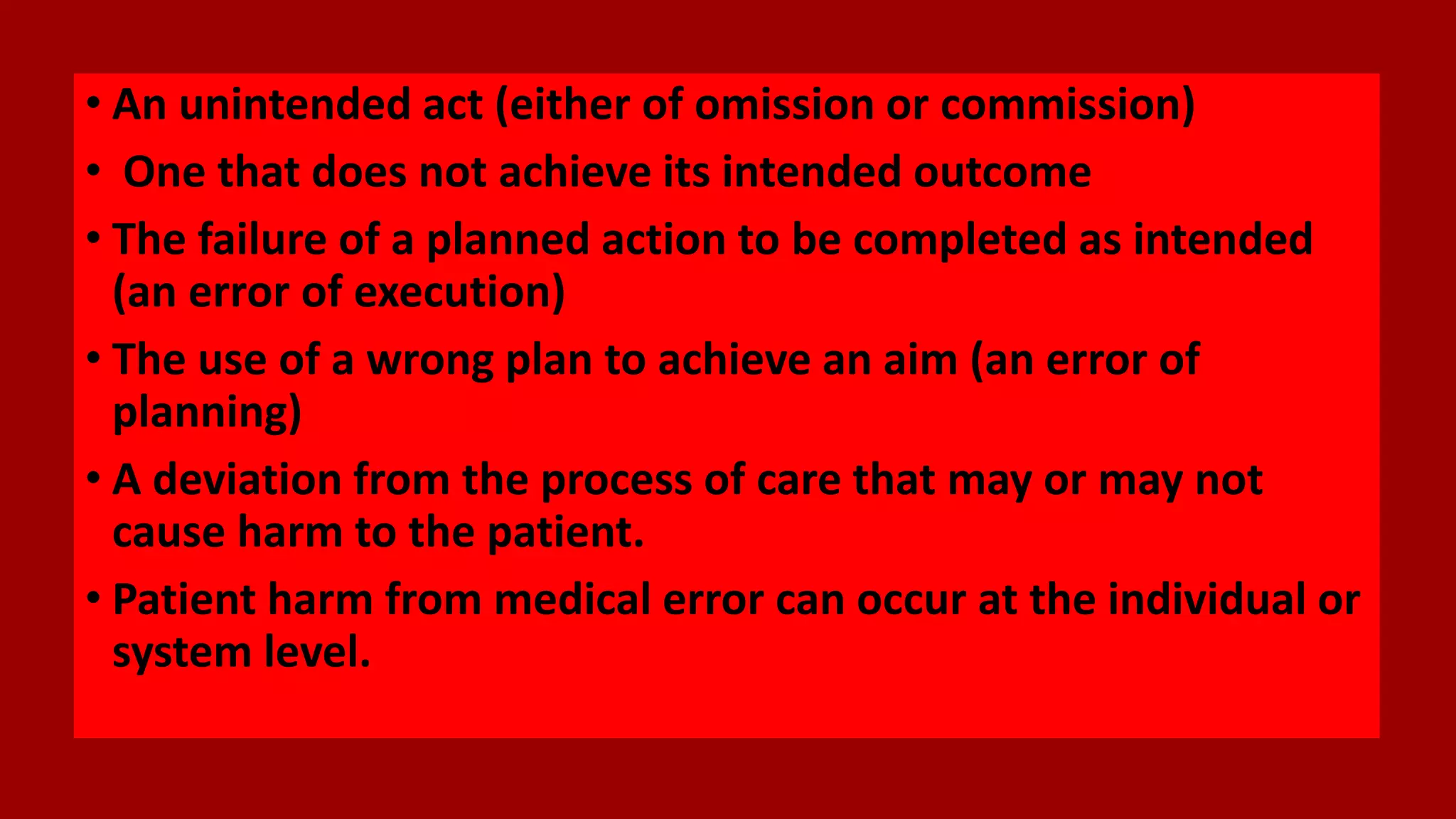
Medical errors represent a serious public health problem and occur frequently in various healthcare settings. They can involve medicines, surgery, diagnosis, equipment, or lab reports. Studies estimate medical errors may be the third leading cause of death in the US, resulting in between 200,000 to 400,000 deaths per year. Many common types of errors like misdiagnosis, unnecessary treatment, medication mistakes, and uncoordinated care have been reduced through standardized protocols and safety practices, but medical errors still frequently harm and kill patients.






![Some Facts
• 440,000 patients die every year from preventable medical
errors. [Journal of Patient Safety]
• Preventable medical errors cost USA tens of billions of dollars a
year. [Institute of Medicine]
• One in three patients who are admitted to the hospital will
experience a medical error. [Health Affairs]
• Studies of wrong site, wrong surgery, wrong patient procedures
show that “never events” are happening at an alarming rate of
up to 40 times per week in U.S. hospitals. [Archives of Surgery ]](https://image.slidesharecdn.com/medicalerrors-170426171835/75/Medical-errors-8-2048.jpg)