excretion pdf.pdf
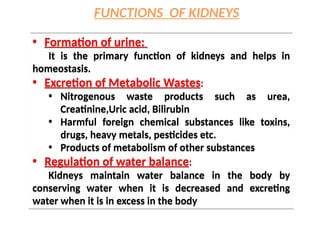
- 1. • Formation of urine: It is the primary function of kidneys and helps in homeostasis. • Excretion of Metabolic Wastes: • Nitrogenous waste products such as urea, Creatinine,Uric acid, Bilirubin • Harmful foreign chemical substances like toxins, drugs, heavy metals, pesticides etc. • Products of metabolism of other substances • Regulation of water balance: Kidneys maintain water balance in the body by conserving water when it is decreased and excreting water when it is in excess in the body • Formation of urine: It is the primary function of kidneys and helps in homeostasis. • Excretion of Metabolic Wastes: • Nitrogenous waste products such as urea, Creatinine,Uric acid, Bilirubin • Harmful foreign chemical substances like toxins, drugs, heavy metals, pesticides etc. • Products of metabolism of other substances • Regulation of water balance: Kidneys maintain water balance in the body by conserving water when it is decreased and excreting water when it is in excess in the body FUNCTIONS OF KIDNEYS
- 2. • Regulation of electrolyte balance: Kidneys retain sodium if the osmolarity of body water decreases and eliminate sodium when osmolarity increases. • Regulation of arterial blood pressure Kidneys play an important role in long term regulation of arterial blood pressure by two ways; by regulating ECF volume and through renin angiotensin system • Regulation of acid base balance: Maintenance of pH of blood and body fluids within normal limits is the function of kidneys. • Regulation of blood calcium level • Regulation of calcium level by activation of vitamin D, which is necessary for intestinal absorption of calcium • Regulation of electrolyte balance: Kidneys retain sodium if the osmolarity of body water decreases and eliminate sodium when osmolarity increases. • Regulation of arterial blood pressure Kidneys play an important role in long term regulation of arterial blood pressure by two ways; by regulating ECF volume and through renin angiotensin system • Regulation of acid base balance: Maintenance of pH of blood and body fluids within normal limits is the function of kidneys. • Regulation of blood calcium level • Regulation of calcium level by activation of vitamin D, which is necessary for intestinal absorption of calcium
- 3. • Endocrine function i.e. secretion of hormones: I. Release of renin II. Release of prostaglandins III. Release of erythropoietin (stimulates RBC production) IV. Activation of vitamin D produced by the skin • Endocrine function i.e. secretion of hormones: I. Release of renin II. Release of prostaglandins III. Release of erythropoietin (stimulates RBC production) IV. Activation of vitamin D produced by the skin • Hemopoietic function: I. Kidneys stimulate the production of erythrocytes or erythropoiesis by secreting erythropoietin. II. Kidneys also secrete another hormone thrombopoietin, which stimulates Thrombopoiesis. • Hemopoietic function: I. Kidneys stimulate the production of erythrocytes or erythropoiesis by secreting erythropoietin. II. Kidneys also secrete another hormone thrombopoietin, which stimulates Thrombopoiesis.
- 7. • Each kidney contains approximately 1 million nephrons. • Each nephron begins with a spherical filtering component, called the renal corpuscle, followed by a long tubule leading out of it that continues until it merges with the tubules of other nephrons to form collecting ducts, which are themselves long tubes. • Collecting ducts eventually merge with others in the renal papilla to form a ureter that conveys urine to the bladder.
- 8. Cortical and Juxtamedullary Nephrons
- 9. CORTICAL NEPHRONS JUXTAMEDULLARY NEPHRONS 85 % Small sized glomeruli located in the renal cortex Short loops of Henle The descending loop of Henle contain a thin segment where as ascending limb contains a thick segment Blood supply to tubules are by peritubular capillaries Filtration rate slow Excretion of waste or formation of urine • 15 % • Large glomeruli located at the junction of the cortex and the medulla • Long loops of Henle • Both the descending and ascending limbs of loop of Henle contain thin segments • Blood supply through vasa recta • High • Counter current mechanism for the concentration of urine. Also urine formation
- 10. RENAL CORPUSCLE • The renal corpuscle is a hollow sphere (Bowman’s capsule) filled with a compact tuft of interconnected capillary loops, the glomerulus • The function of renal corpuscle is filtration of blood which forms first phase of urine formation • Is formed of two parts; 1. Glomerulus 2. Bowman‘s capsule RENAL CORPUSCLE • The renal corpuscle is a hollow sphere (Bowman’s capsule) filled with a compact tuft of interconnected capillary loops, the glomerulus • The function of renal corpuscle is filtration of blood which forms first phase of urine formation • Is formed of two parts; 1. Glomerulus 2. Bowman‘s capsule
- 11. GLOMERULUS • Is a rounded tuft of capillaries enclosed by bowman’s capsule • Blood enters the capillaries inside Bowman’s capsule through an afferent arteriole that penetrates the surface of the capsule at one side, called the vascular pole. • Blood then leaves the capillaries through a nearby efferent arteriole on the same side. • The diameter of efferent arteriole is less than that of afferent arteriole • The capillaries are made up of single layer of endothelial cells • Another cell type—the mesangial cell—is found in close association with the capillary loops of the glomerulus. Glomerular mesangial cells act as phagocytes. • They also contain large numbers of myofilaments and can contract in response to a variety of stimuli GLOMERULUS • Is a rounded tuft of capillaries enclosed by bowman’s capsule • Blood enters the capillaries inside Bowman’s capsule through an afferent arteriole that penetrates the surface of the capsule at one side, called the vascular pole. • Blood then leaves the capillaries through a nearby efferent arteriole on the same side. • The diameter of efferent arteriole is less than that of afferent arteriole • The capillaries are made up of single layer of endothelial cells • Another cell type—the mesangial cell—is found in close association with the capillary loops of the glomerulus. Glomerular mesangial cells act as phagocytes. • They also contain large numbers of myofilaments and can contract in response to a variety of stimuli
- 12. BOWMAN’S CAPSULE • It encloses the glomerulus • It is formed of two layers; inner visceral layer and outer parietal layer • Visceral layer covers the glomerular capillaries and is continued as the parietal layer at the visceral pole. • Parietal layer is continued with the wall of tubular portion of nephron. • The space within Bowman’s capsule not occupied by the glomerulus is called the urinary space or Bowman’s space, and it is into this space that fluid filters from the glomerular capillaries. It is continued as the lumen of the tubular portion. • Both the layers of bowman's capsule are composed of a single layer of epithelial cells resting on a basement membrane BOWMAN’S CAPSULE • It encloses the glomerulus • It is formed of two layers; inner visceral layer and outer parietal layer • Visceral layer covers the glomerular capillaries and is continued as the parietal layer at the visceral pole. • Parietal layer is continued with the wall of tubular portion of nephron. • The space within Bowman’s capsule not occupied by the glomerulus is called the urinary space or Bowman’s space, and it is into this space that fluid filters from the glomerular capillaries. It is continued as the lumen of the tubular portion. • Both the layers of bowman's capsule are composed of a single layer of epithelial cells resting on a basement membrane
- 13. • The proximal tubule, which drains Bowman’s capsule, consists of a coiled segment, the proximal convoluted tubule (pars convoluta) followed by a straight segment, the proximal straight tubule (pars recta) which descends toward the medulla, perpendicular to the cortical surface of the kidney. • Made up of single layer of cuboidal epithelial cells • Apical membrane contain microvilli or hair like projections directed towards the lumen of the tubule, hence called brush bordered epithelium • About 75% of sodium is removed from fluid here (by active transport, chloride follows passively. • The proximal tubule, which drains Bowman’s capsule, consists of a coiled segment, the proximal convoluted tubule (pars convoluta) followed by a straight segment, the proximal straight tubule (pars recta) which descends toward the medulla, perpendicular to the cortical surface of the kidney. • Made up of single layer of cuboidal epithelial cells • Apical membrane contain microvilli or hair like projections directed towards the lumen of the tubule, hence called brush bordered epithelium • About 75% of sodium is removed from fluid here (by active transport, chloride follows passively. PROXIMAL CONVOLUTED TUBULE
- 14. • The next segment is the descending thin limb of the loop of Henle (or simply the descending thin limb). • The descending thin limbs of different nephrons penetrate into the medulla to varying depths, and then abruptly reverse at a hairpin turn and begin an ascending portion of the loop of Henle parallel to the descending portion. • In long loops, the epithelium of the first portion of the ascending limb remains thin. This segment is called the ascending thin limb. Further up the ascending portion the epithelium thickens, and this next segment is called the thick ascending limb. • In short loops, there is no ascending thin portion, and the thick ascending portion begins right at the hairpin loop. LOOP OF HENLE
- 15. • The thick ascending limb rises back into the cortex to the very same Bowman’s capsule from which the tubule originated. Here it passes directly between the afferent and efferent arterioles at the point where they enter and exit the renal corpuscle. • The cells in the thick ascending limb closest to Bowman’s capsule (between the afferent and efferent arterioles) are a group of specialized cells known as the macula densa . • LOOP OF HENLE: act as The counter current multiplier: – Descending Loop Of Henle: Permeable to water and other solute – Ascending Loop Of Henle: Chloride ions--active transport out. Sodium follows. Water does NOT.
- 16. • The macula densa marks the end of the thick ascending limb and the beginning of the distal convoluted tubule. • Made up of cuboidal epithelial cells which are larger(I cells) in size and have extensive infoldings of basolateral membrane without brush border. • Responds to Aldosterone and ADH • Distal convoluted tubule: NaCl, Potassium, ammonia, carbonate removed here. • The macula densa marks the end of the thick ascending limb and the beginning of the distal convoluted tubule. • Made up of cuboidal epithelial cells which are larger(I cells) in size and have extensive infoldings of basolateral membrane without brush border. • Responds to Aldosterone and ADH • Distal convoluted tubule: NaCl, Potassium, ammonia, carbonate removed here. DISTAL CONVOLUTED TUBULE
- 17. • DCT is followed by the connecting tubule, which leads to the cortical collecting tubule. • Connecting tubules from several nephrons merge to form cortical collecting tubules, and a number of initial collecting ducts. • Seven to ten initial collecting ducts unite to form the straight collecting duct. • At the inner zone of medulla, the straight collecting duct from each medullary pyramid unite to form papillary ducts or ducts of Bellini, which opens in to papilla. • Papilla collects urine from each medullary pyramid and drains in to a minor calyx • Three or four minor calyces unite to form major calyx • Each kidney has about 8 minor calyces and 2 or 3 major calyces • The major calyces open in to renal pelvis which is the expended portion of ureter • DCT is followed by the connecting tubule, which leads to the cortical collecting tubule. • Connecting tubules from several nephrons merge to form cortical collecting tubules, and a number of initial collecting ducts. • Seven to ten initial collecting ducts unite to form the straight collecting duct. • At the inner zone of medulla, the straight collecting duct from each medullary pyramid unite to form papillary ducts or ducts of Bellini, which opens in to papilla. • Papilla collects urine from each medullary pyramid and drains in to a minor calyx • Three or four minor calyces unite to form major calyx • Each kidney has about 8 minor calyces and 2 or 3 major calyces • The major calyces open in to renal pelvis which is the expended portion of ureter COLLECTING DUCT
- 18. It is made up of three types of cells (1) Juxtaglomerular cells (granular cells),which are specialized smooth muscle cells surrounding the afferent arteriole. • The granular cells are named because they contain secretory vesicles that appear granular. These granules contain the hormone renin. (2) Mesangial cells are of two types; I. Extraglomerular mesangial cells are also called lacis cells or agranular cells. These are situated in the triangular region bound by afferent arteriole, efferent arteriole and macula densa. Act as relay centre. II. Intraglomerular mesangial cells or glomerular mesangial cells are situated between the glomerular capillaries and form a cellular network which supports capillary loops. These cells are contractile in nature. It is made up of three types of cells (1) Juxtaglomerular cells (granular cells),which are specialized smooth muscle cells surrounding the afferent arteriole. • The granular cells are named because they contain secretory vesicles that appear granular. These granules contain the hormone renin. (2) Mesangial cells are of two types; I. Extraglomerular mesangial cells are also called lacis cells or agranular cells. These are situated in the triangular region bound by afferent arteriole, efferent arteriole and macula densa. Act as relay centre. II. Intraglomerular mesangial cells or glomerular mesangial cells are situated between the glomerular capillaries and form a cellular network which supports capillary loops. These cells are contractile in nature. JUXTAGLOMERULAR (JG) APPARATUS
- 19. (3) The macula densa is the terminal portion of thick ascending segment of henle’s loop that runs in between afferent and efferent arteriole. • The macula densa cells are detectors of the composition of the fluid within the nephron at the very end of the thick ascending limb and contribute to the control of glomerular filtration rate.
- 20. FUNCTIONS OF JGA • JG cells act as baroreceptors and responds to changes in transmural pressure gradient. JG cells also act as vascular volume receptors and monitor renal perfusion pressure. • Macula densa act as chemoreceptors and are stimulated by decreased sodium chloride concentration. • Mesangial or lacis cells are in contact with both macula densa and JG cells and relay signals from macula densa to the JG cells. • Secretion of renin by juxtaglomerular cells and helps in regulation of BP and in turn RBF and GFR. • Secretion of other substances i.e. • Prostaglandins by extraglomerular mesangial cells • In vitro secretion of cytokines like IL-2 and TNF by mesangial cells • Thromboxane A 2 by macula densa FUNCTIONS OF JGA • JG cells act as baroreceptors and responds to changes in transmural pressure gradient. JG cells also act as vascular volume receptors and monitor renal perfusion pressure. • Macula densa act as chemoreceptors and are stimulated by decreased sodium chloride concentration. • Mesangial or lacis cells are in contact with both macula densa and JG cells and relay signals from macula densa to the JG cells. • Secretion of renin by juxtaglomerular cells and helps in regulation of BP and in turn RBF and GFR. • Secretion of other substances i.e. • Prostaglandins by extraglomerular mesangial cells • In vitro secretion of cytokines like IL-2 and TNF by mesangial cells • Thromboxane A 2 by macula densa
- 23. The juxtaglomerular cells secrete renin. When renin is released in to the blood, it acts on angiotensinogen and converts it in to angiotensin I and then in to angiotensin II. Angiotensin II is short-lived and degrade in to angiotensin III and then in to angiotensin IV. Angiotensin II is the most active form. Its actions are; 1. Increases arterial blood pressure by causing vasoconstriction 2. It stimulates secretion of aldosterone 3. Regulates glomerular filtration 4. Increases sodium reabsorption 5. Increases water intake by stimulating thirst centre 6. Increases secretion of ADH
- 24. RBF- REGULATION • 1.2 – 1.3 Liters / min - 21% of CO • AUTOREGULATION of RBF – Intrinsic ability of renal blood flow to regulate its own blood flow is called autoregulation. – Autoregulation is also seen in other vital organs like brain and heart. It is highly significant and effective in kidneys only. – It is important to maintain the GFR. Blood flow to kidneys remains normal even when the mean arterial pressure vary widely between 60 and 180 mm Hg. RBF- REGULATION • 1.2 – 1.3 Liters / min - 21% of CO • AUTOREGULATION of RBF – Intrinsic ability of renal blood flow to regulate its own blood flow is called autoregulation. – Autoregulation is also seen in other vital organs like brain and heart. It is highly significant and effective in kidneys only. – It is important to maintain the GFR. Blood flow to kidneys remains normal even when the mean arterial pressure vary widely between 60 and 180 mm Hg.
- 25. TUBULO-GLOMERULAR FEEDBACK • Macula densa plays an important role in tubulo- glomerular feedback for controlling the RBF and GFR • Macula densa act as a sensor and detects the concentration of sodium chloride in the tubular fluid and accordingly alters the glomerular blood flow and GFR. TUBULO-GLOMERULAR FEEDBACK • Macula densa plays an important role in tubulo- glomerular feedback for controlling the RBF and GFR • Macula densa act as a sensor and detects the concentration of sodium chloride in the tubular fluid and accordingly alters the glomerular blood flow and GFR. – Two mechanisms are involved in renal autoregulation • MYOGENIC MECHANISM OF AUTOREGULATION • TUBULO-GLOMERULAR FEED BACK MECHANISM
- 26. • When sodium chloride concentration increases in the filtrate, macula densa releases adenosine from ATP. It causes constriction of afferent arteriole. So the blood flow decreases leading to decrease in GFR. • When sodium chloride concentration increases in the filtrate, macula densa releases adenosine from ATP. It causes constriction of afferent arteriole. So the blood flow decreases leading to decrease in GFR. • When sodium chloride concentration decreases, macula densa secrete prostaglandin, bradykinin and renin. • PGE2 and kinins cause dilatation of afferent arteriole. • Renin causes angiotensin activation which causes constriction of efferent arteriole. • Both results in increase in RBF & GFR. • When sodium chloride concentration decreases, macula densa secrete prostaglandin, bradykinin and renin. • PGE2 and kinins cause dilatation of afferent arteriole. • Renin causes angiotensin activation which causes constriction of efferent arteriole. • Both results in increase in RBF & GFR.
- 27. • Whenever blood flow to kidney increases, it stretches the elastic wall of the afferent arteriole. • Stretching of vessel wall increases the flow of calcium ions from ECF in to the cells • The influx of calcium ions leads to the contraction of smooth muscles of afferent arteriole which causes constriction of afferent arteriole • So the blood flow is decreased • Whenever blood flow to kidney increases, it stretches the elastic wall of the afferent arteriole. • Stretching of vessel wall increases the flow of calcium ions from ECF in to the cells • The influx of calcium ions leads to the contraction of smooth muscles of afferent arteriole which causes constriction of afferent arteriole • So the blood flow is decreased
- 28. Renal circulation • Renal arteries arises directly from abdominal aorta and enters the kidney through the hilus. • The renal artery divides in to segmental arteries, interlobar artery, arcuate artery, interlobular artery, afferent arteriole, glomerular capillaries, efferent arteriole. • The renal circulation forms a portal system by the presence of two capillaries; glomerular capillaries and peritubular capillaries or vasa recta. • Peritubular capillaries and vasa recta drain in to venous system. It start as peritubular venules and continues as interlobular veins, arcuate veins, interlobar veins, segmental veins and finally the renal vein. The renal vein leaves the kidney through the hilus and joins inferior venacava.
- 29. Special features 1. The renal arteries arise directly from the aorta, so the high aortic pressure facilitatates high blood flow . 2. Receives 26% of cardiac output about 1300ml/minute 3. When blood passes through glomerular capillaries blood is completely filtered. 4. High pressure is maintained in glomerular capillaries helps in filtration. Low pressure in peritubular capillaries helps in tubular reabsorption. 5. It has a portal system; glomerular capillaries and peritubular capillaries. 6. Renal autoregulation is well developed.
- 31. FILTRATION MEMBRANE It is formed by three layers; The glomerular capillary membrane is formed by single layer of endothelial cells which are attached to the basement membrane. The capillary membrane has many pores called fenestra or filtration pores. Allows water, small solutes but proteins are not filtered. Basement membrane of glomerular capillaries fuses with the basement membrane of visceral layer. Act as a barrier for the protein Visceral layer of bowman’s capsule composed of single layer of flattened epithelial cells resting on a basement membrane. Each cell is connected with the basement membrane by cytoplasmic extensions called pedicles or podocytes. The pedicles are arranged in an interdigitating manner leaving small cleft like spaces in between called slit pores. Filtration occurs through these slit pores. FILTRATION MEMBRANE It is formed by three layers; The glomerular capillary membrane is formed by single layer of endothelial cells which are attached to the basement membrane. The capillary membrane has many pores called fenestra or filtration pores. Allows water, small solutes but proteins are not filtered. Basement membrane of glomerular capillaries fuses with the basement membrane of visceral layer. Act as a barrier for the protein Visceral layer of bowman’s capsule composed of single layer of flattened epithelial cells resting on a basement membrane. Each cell is connected with the basement membrane by cytoplasmic extensions called pedicles or podocytes. The pedicles are arranged in an interdigitating manner leaving small cleft like spaces in between called slit pores. Filtration occurs through these slit pores.
- 33. GLOMERULAR FILTRATION • It is the process by which the blood that passes through glomerular capillaries is filtered through filtration membrane in to the bowman’s capsule. • All the substances are filtered except plasma proteins. It is because plasma proteins are larger than the slit pores present in capillary endothelium. • The filtered fluid is called glomerular filtrate. • The rate at which glomerular filtration takes place is called GFR. • Glomerular filtration rate or GFR is defined as the total quantity of filtrate formed in all nephrons of both the kidneys in the given unit of time. The normal GFR is 125 ml/minute.
- 34. DETERMINANTS OF GFR The rate of filtration in all capillaries, including the glomeruli, is determined by the hydraulic permeability of the capillaries, their surface area, and the net filtration pressure (NFP) acting across them, given as follows: Rate of filtration = Hydraulic permeability × Surface area × NFP Because it is difficult to estimate the area of a capillary bed, a parameter called the filtration coefficient (Kf) is used to denote the product of the hydraulic permeability and the area. The NFP is the algebraic sum of the hydrostatic pressures and the osmotic pressures resulting from protein(the oncotic, or colloid osmotic pressures)on the two sides of the capillary wall.
- 35. • There are four pressures to consider: two hydrostatic pressures and two oncotic pressures. These are the Starling forces. NPF = (PGC – PBC) – (πGC – πBC) where PGC is glomerular capillary hydraulic pressure (promotes filtration), πBC the oncotic pressure of fluid in Bowman’s capsule (promotes filtration),, PBC the hydraulic pressure in Bowman’s capsule (opposes filtration), and πGC the oncotic pressure in glomerular capillary plasma(opposes filtration). • Because there is normally little total protein in Bowman’s capsule, πBC may be taken as zero and not considered in our analysis. • Accordingly, the overall equation for GFR becomes: GFR = Kf (PGC – PBC – πGC)
- 36. • The Kf is a measure of the product of the hydraulic conductivity and surface area of the glomerular capillaries. • The normal Kf is calculated to be about 12.5 ml/min/mm Hg of filtration pressure • The GFR can therefore be expressed as GFR = Kf x (PGC – PBS – pGC + pBS) Forces Favouring Filtration (mm Hg) • Glomerular hydrostatic pressure= 60 • Bowman’s capsule colloid osmotic pressure = 0 Forces Opposing Filtration (mm Hg) • Bowman’s capsule hydrostatic pressure =18 • Glomerular capillary colloid osmotic pressure= 32 Net filtration pressure = 60 – 18 – 32 = +10 mm Hg
- 38. FACTORS AFFECTING GFR 1. GFR is directly proportional to renal blood flow, glomerular capillary pressure, surface area of capillary membrane, permeability of capillary membrane. 2. GFR is inversely proportional to colloidal osmotic pressure and hydrostatic pressure in bowman's capsule 3. Constriction of afferent arteriole reduces blood flow and in turn decreases GFR 4. Constriction of efferent arteriole increases GFR initially due to stagnation of blood and then declines 5. Tubuloglomerular feedback 6. Sympathetic stimulation causes initial increase and then decreases. 7. Contraction of glomerular mesangial cells decreases surface area of capillaries resulting in reduction in GFR 8. Hormonal or other factors: many hormones alter GFR FACTORS AFFECTING GFR 1. GFR is directly proportional to renal blood flow, glomerular capillary pressure, surface area of capillary membrane, permeability of capillary membrane. 2. GFR is inversely proportional to colloidal osmotic pressure and hydrostatic pressure in bowman's capsule 3. Constriction of afferent arteriole reduces blood flow and in turn decreases GFR 4. Constriction of efferent arteriole increases GFR initially due to stagnation of blood and then declines 5. Tubuloglomerular feedback 6. Sympathetic stimulation causes initial increase and then decreases. 7. Contraction of glomerular mesangial cells decreases surface area of capillaries resulting in reduction in GFR 8. Hormonal or other factors: many hormones alter GFR
- 39. FACTORS INCREASING GFR BY VASODILATION are I. Natriuretic Peptide[ANP & BNP] II. cAMP III. Dopamine IV. Endothelial derived nitric oxide V. Prostaglandin E2 FACTORS DECREASING GFR BY VASOCONSTRICTION are VI. Angiotensin II VII. Endothelins VIII.Noradrenaline IX. Platelet activating factor X. Platelet derived factor XI. Prostaglandin F2 FACTORS INCREASING GFR BY VASODILATION are I. Natriuretic Peptide[ANP & BNP] II. cAMP III. Dopamine IV. Endothelial derived nitric oxide V. Prostaglandin E2 FACTORS DECREASING GFR BY VASOCONSTRICTION are VI. Angiotensin II VII. Endothelins VIII.Noradrenaline IX. Platelet activating factor X. Platelet derived factor XI. Prostaglandin F2
- 40. TUBULAR REABSORPTION • It is the process by which water and other substances are transported from renal tubules back to the blood • It is selective reabsorption • Essential substances such as glucose, aminoacids and vitamins are completely reabsorbed from renal tubule. SITES OF REABSORPTION PCT: (about 88%) mainly glucose, aminoacids, sodium, potassium, calcium, bicarbonates, chlorides, phosphates , uric acid and water. Loop of Henle: Sodium and chloride DCT: Sodium, calcium, bicarbonate, and water SITES OF REABSORPTION PCT: (about 88%) mainly glucose, aminoacids, sodium, potassium, calcium, bicarbonates, chlorides, phosphates , uric acid and water. Loop of Henle: Sodium and chloride DCT: Sodium, calcium, bicarbonate, and water
- 41. TUBULAR SECRETION • It is the process by which the substances are transported from blood in to renal tubules • Substances secreted are • Potassium is secreted actively by sodium potassium pump in proximal and distal convoluted tubules and collecting ducts • Ammonia is secreted in the proximal convoluted tubules • Hydrogen ions are secreted in the proximal and distal convoluted tubules
- 42. MODIFICATION OF URINE • Changes in concentration of urine : Either concentrated [if water content in the body decreases] or dilute urine [for excreting excess water]is formed. • Acidification of urine is done [by excreting excess hydrogen ions and retaining bicarbonate ions] for maintaining acid- base balance MODIFICATION OF URINE • Changes in concentration of urine : Either concentrated [if water content in the body decreases] or dilute urine [for excreting excess water]is formed. • Acidification of urine is done [by excreting excess hydrogen ions and retaining bicarbonate ions] for maintaining acid- base balance
- 43. Formation of DILUTE Urine • Formation of dilute urine occurs when the fluid reaches DCT • It occurs when there is excess of water in the body and decreased osmolarity, which is achieved by inhibition of ADH secretion. • When volume of body fluid increases or osmolarity decreases, ADH secretion stops. So water reabsorption from renal tubules does not take place and leads to excretion of large amount of water in urine making the urine dilute Formation of DILUTE Urine • Formation of dilute urine occurs when the fluid reaches DCT • It occurs when there is excess of water in the body and decreased osmolarity, which is achieved by inhibition of ADH secretion. • When volume of body fluid increases or osmolarity decreases, ADH secretion stops. So water reabsorption from renal tubules does not take place and leads to excretion of large amount of water in urine making the urine dilute
- 44. Formation of concentrated urine It involves two important processes ; 1. Medullary gradient 2. Secretion of ADH Formation of concentrated urine It involves two important processes ; 1. Medullary gradient 2. Secretion of ADH • ADH is a hormone secreted by posterior pituitary in response to either decreased body fluid volume or increased sodium concentration. ADH increases the water reabsorption from DCT & collecting duct resulting in concentration of urine
- 45. Medullary gradient • The osmolarity of cortical interstitial fluid is isotonic to plasma i.e. 300 mOsm/L. The osmolarity of medullary interstitial fluid near the cortex is 300 mOsm/L. • It then increases gradually and reaches the maximum of 1200 mOsm/L at the innermost part of medulla near the renal sinus. • This type of gradual increase in the osmolarity of medullary interstitial fluid is called medullary gradient. • Maintenance of medullary gradient and hyperosmolarity of interstitial fluid is done by countercurrent system.
- 46. In kidneys, counter current system composed of Loop of Henle, act as counter current multiplier and is responsible for production of hyperosmolarity and medullary gradient Vasa recta, act as counter current exchanger ad is responsible for the maintenance of medullary gradient and hyperosmolarity. In kidneys, counter current system composed of Loop of Henle, act as counter current multiplier and is responsible for production of hyperosmolarity and medullary gradient Vasa recta, act as counter current exchanger ad is responsible for the maintenance of medullary gradient and hyperosmolarity.
- 47. Loop of Henle act as counter current multiplier Medullary gradient is developed by active reabsorption of sodium chloride and other solutes from ascending limb of loop of Henle in to medullary interstitium. These salts get accumulated in the medullary interstitium and increase the osmolarity. Now due to concentration gradient the sodium and chloride ions diffuse from medullary interstitium into descending limb of henle's loop. Sodium and chloride ions are repeatedly recirculated between ascending and descending limb. In addition more and more new sodium and chloride ions are added by constant filtration. Loop of Henle act as counter current multiplier Medullary gradient is developed by active reabsorption of sodium chloride and other solutes from ascending limb of loop of Henle in to medullary interstitium. These salts get accumulated in the medullary interstitium and increase the osmolarity. Now due to concentration gradient the sodium and chloride ions diffuse from medullary interstitium into descending limb of henle's loop. Sodium and chloride ions are repeatedly recirculated between ascending and descending limb. In addition more and more new sodium and chloride ions are added by constant filtration.
- 48. Vasa recta act as counter current exchanger • It runs parallel to loop of Henle. • Sodium chloride reabsorbed from ascending limb of henle's loop enters medullary interstitium. From here it enters the descending limb of vasa recta • Simultaneously water diffuses from descending limb of vasa recta. • The blood flows very slowly through vasa recta. So a large quantity of sodium chloride accumulates in descending limb of vasa recta and flows slowly towards ascending limb of vasa recta • Increase in sodium chloride concentration causes diffusion of sodium chloride in to medullary interstitium • Water from medullary interstitium enters ascending limb and cycle is repeated. Vasa recta act as counter current exchanger • It runs parallel to loop of Henle. • Sodium chloride reabsorbed from ascending limb of henle's loop enters medullary interstitium. From here it enters the descending limb of vasa recta • Simultaneously water diffuses from descending limb of vasa recta. • The blood flows very slowly through vasa recta. So a large quantity of sodium chloride accumulates in descending limb of vasa recta and flows slowly towards ascending limb of vasa recta • Increase in sodium chloride concentration causes diffusion of sodium chloride in to medullary interstitium • Water from medullary interstitium enters ascending limb and cycle is repeated.
- 50. The excretion of hydrogen ions is done by kidneys for preventing metabolic acidosis. Three mechanisms are 1. By bicarbonate mechanism 2. By phosphate mechanism 3. By ammonia mechanism
- 52. PROPERTIES OF URINE 1. VOLUME: Normal urine output per day is 800-2500 ml. abnormalities are polyuria, oliguria, and anuria 2. COLOUR : Yellow colour is due to presence of urochrome a compound of urobilin and urobilinogen with peptide. On standing colour deepens. I. Brownish yellow indicates jaundice , II. Cloudy appearance seen in strongly alkaline urine, III. Frothy appearance indicates proteinuria, IV. Red dark brown tinge seen in porphyria 3. OSMOLALITY AND SPECIFIC GRAVITY: Normal urinary osmolality varies from 50 to 1200 mom/kg and specific gravity from 1.003 to 1.030. 4. pH: Normally varies from 4.5 to 8
- 53. ABNORMAL CONSTITUENTS OF URINE 1. PROTEINURIA: Excretion of greater than 150 mg/day of protein. It occurs in conditions like congestive heart failure, after prolonged standing, renal diseases and in toxaemia of pregnancy 2. GLYCOSURIA: Refers to the presence of glucose in the urine. It may be due to diabetes mellitus, renal disorders, GIT disorders. 3. KETONURIA: Refers to the presence of ketone bodies in the urine. It occurs in patients suffering from ketosis due to severe DM or prolonged starvation 4. BILIRUBINURIA: Refers to the presence of bilirubin in the urine occurs in jaundice 5. HAEMOGLOBINURIA: Presence of hemoglobin in urine indicates intravascular haemolysis 6. HEMATURIA: Presence of blood in the urine is seen in acute glomerulonephritis and renal stone disease
- 54. URINARY BLADDER
- 55. NERVE SUPPLY TO URINARY BLADDER AND SPHINCTERS • Sympathetic nerve fibres arise from first two lumbar segments of spinal cord through hypogastric nerve causes of filling of bladder by relaxation of detrusor muscle and constriction of internal sphincter • Parasympathetic nerve fibres arises from S2,S3,S4 segments through pelvic nerve causes emptying of urinary bladder by contraction of detrusor muscle and relaxation of internal sphincter. NERVE SUPPLY TO URINARY BLADDER AND SPHINCTERS • Sympathetic nerve fibres arise from first two lumbar segments of spinal cord through hypogastric nerve causes of filling of bladder by relaxation of detrusor muscle and constriction of internal sphincter • Parasympathetic nerve fibres arises from S2,S3,S4 segments through pelvic nerve causes emptying of urinary bladder by contraction of detrusor muscle and relaxation of internal sphincter. • Somatic nerve supply arising from S2,S3,S4 innervates external sphincter through pudendal nerve causes its constriction. Inhibition of pudendal nerve results in micturition by relaxation of external sphincter • Somatic nerve supply arising from S2,S3,S4 innervates external sphincter through pudendal nerve causes its constriction. Inhibition of pudendal nerve results in micturition by relaxation of external sphincter
- 56. MICTURITION CENTRES • Micturition process is controlled by • Spinal centres which are located in sacral, lower thoracic and upper lumbar segments of spinal cord. • Higher centres regulating spinal centres are of types; • Inhibitory centres situated in midbrain and cerebral cortex • Facilitatory centres situated in pons and cerebral cortex MICTURITION CENTRES • Micturition process is controlled by • Spinal centres which are located in sacral, lower thoracic and upper lumbar segments of spinal cord. • Higher centres regulating spinal centres are of types; • Inhibitory centres situated in midbrain and cerebral cortex • Facilitatory centres situated in pons and cerebral cortex
- 57. Micturition reflex • It is the reflex by which micturition occurs and is elicited by stimulation of stretch receptors situated on the wall of urinary bladder and urethra. • It is a self generative reflex i.e. the initial contraction of bladder further activate the receptors to cause still further increase in sensory reflex contraction of bladder and urethra. These impulses in turn cause further increase in reflex contraction of bladder • During micturition the flow of urine is facilitated by the increase in the abdominal pressure due to voluntary contraction of abdominal muscle Micturition reflex • It is the reflex by which micturition occurs and is elicited by stimulation of stretch receptors situated on the wall of urinary bladder and urethra. • It is a self generative reflex i.e. the initial contraction of bladder further activate the receptors to cause still further increase in sensory reflex contraction of bladder and urethra. These impulses in turn cause further increase in reflex contraction of bladder • During micturition the flow of urine is facilitated by the increase in the abdominal pressure due to voluntary contraction of abdominal muscle • Micturition is the process by which the urinary bladder empties when it becomes filled.
- 58. Filling of urinary bladder Filling of urinary bladder Stimulation of stretch receptors in the bladder Stimulation of stretch receptors in the bladder Afferent impulses via pelvic nerve to sacral segments of spinal cord Afferent impulses via pelvic nerve to sacral segments of spinal cord Contraction of detrusor muscle and relaxation of internal sphincter Contraction of detrusor muscle and relaxation of internal sphincter Flow of urine in to urethra from the bladder Flow of urine in to urethra from the bladder stretch receptors in the urethra stimulated and impulses send to spinal cord stretch receptors in the urethra stimulated and impulses send to spinal cord Results in inhibition of pudendal nerve and relaxation of external sphincter Results in inhibition of pudendal nerve and relaxation of external sphincter Voiding of urine Voiding of urine MICTURITION REFLEX
- 59. • When about 300 to 400 ml of urine is collected in the bladder, the pressure inside the bladder increases • This stretches bladder wall resulting in stimulation of stretch receptors and generation of sensory impulses • Sensory impulses reaches the sacral segments of spinal cord via pelvic nerve • The motor impulses from the spinal cord travel through motor fibres of pelvic nerve towards bladder and internal sphincter • It causes contraction of detrusor muscle and relaxation of internal sphincter so that urine enters urethra from bladder • Once urine enters urethra the stretch receptors in the urethra are stimulated and send impulses to spinal cord via pelvic nerve • These impulses inhibit pudendal nerve resulting in relaxation of external sphincter and micturition occurs • When about 300 to 400 ml of urine is collected in the bladder, the pressure inside the bladder increases • This stretches bladder wall resulting in stimulation of stretch receptors and generation of sensory impulses • Sensory impulses reaches the sacral segments of spinal cord via pelvic nerve • The motor impulses from the spinal cord travel through motor fibres of pelvic nerve towards bladder and internal sphincter • It causes contraction of detrusor muscle and relaxation of internal sphincter so that urine enters urethra from bladder • Once urine enters urethra the stretch receptors in the urethra are stimulated and send impulses to spinal cord via pelvic nerve • These impulses inhibit pudendal nerve resulting in relaxation of external sphincter and micturition occurs
- 60. • Renal clearance of a substance is the volume of plasma that is completely cleared of the substance by the kidneys per unit time • Renal clearance of a substance is calculated from the urinary excretion rate (Us V) of that substance divided by its plasma concentration. Cs = Us x V Ps where Cs is the clearance rate of a substance s, Ps is the plasma concentration of the substance, Us is the urine concentration of that substance, and V is the volume of urine excreted.
- 61. If a substance is freely filtered and is not reabsorbed or secreted by the renal tubules, then GFR = CS A substance that fits these criteria is inulin and creatinine. If a substance is completely filtered and secreted but not reabsorbed, the clearance rate of that substance is equal to the total renal plasma flow. The clearance of PAH can be used as an approximation of renal plasma flow. PAH {PARA-AMINOHIPPURIC acid} If renal plasma flow is 650 ml/min and GFR is 125 ml/min, the filtration fraction (FF) is calculated as FF = GFR/RPF = 125/650 = 0.19
- 62. • Urinary incontinence (UI) is loss of bladder control. • Most bladder control problems happen when muscles are too weak [stress incontinence] or too active [urge incontinence or overactive bladder]. Atonic bladder • Caused by destruction of sensory nerve fibres Automatic bladder • Caused by spinal cord damage above the sacral region Uninhibited neurogenic bladder • Caused by lack of inhibitory signals from the brain, which results in frequent and relatively uncontrolled micturition.
- 63. Diuretics • A diuretic (colloquially called a water pill) is any drug that elevates the rate of bodily urine excretion (diuresis) • Diuretics also decrease the extracellular fluid (ECF) volume, and are primarily used to produce a negative extracellular fluid balance. • Caffeine, cranberry juice and alcohol are all weak diuretics. In medicine, diuretics are used to treat heart failure, liver cirrhosis, hypertension and certain kidney diseases. Diuretics alleviate the symptoms of these diseases by causing sodium and water loss through the urine. • Some diuretics, such as acetazolamide, help to make the urine more alkaline and are helpful in increasing excretion of substances such as aspirin in cases of overdose or poisoning.
- 64. Diabetes Insipidus • This is caused by the deficiency of or decrease of ADH. • The person with (DI) has the inability to concentrate their urine in water restriction, in turn they will void up 3 to 20 litres/day. • There are two forms of (DI), neurogenic, and nephrogenic. • In nephrogenic (DI) the kidneys do not respond to ADH. Usually the nephrogenic (DI) is characterized by the impairment of the urine concentrating capability of the kidney along with concentration of water. The cause may be a genetic trait, electrolyte disorder, or side effect of drugs such as lithium. • In the neurogenic (DI), it is usually caused by head injury near the pituitary.
- 65. Kidney stones, also known as nephrolithiases, urolithiases or renal calculi • are solid crystals of dissolved minerals in urine found inside the kidneys or ureters. • They vary in size and texture. • Kidney stones typically leave the body in the urine stream; if they grow relatively large results in obstruction of a ureter and distention with urine. • It may cause severe pain most commonly felt in the flank, lower abdomen and groin. • Few symptoms of kidney stones 1. Pain in the abdomen or back 2. Pain spreading to the groin area or testicles 3. Blood in the urine 4. Nausea or vomiting 5. Burning sensation during urination
- 66. • Glomerulonephritis is usually caused by an abnormal immune reaction that damages the glomeruli. • In about 95 per cent of the patients with this disease, damage to the glomeruli occurs 1 to 3 weeks after an infection elsewhere in the body, usually caused by certain types of group A beta streptococci. • antibodies develop against the streptococcal antigen and antigen react with each other to form an insoluble immune complex that becomes entrapped in the glomeruli, especially in the basement membrane portion of the glomeruli. • Large numbers of white blood cells become entrapped in the glomeruli. Many of the glomeruli become blocked by this inflammatory reaction, and those that are not blocked usually become excessively permeable,allowing both protein and red blood cells.
- 67. (1) acute renal failure, in which the kidneys abruptly stop working entirely or almost entirely but may eventually recover nearly normal function, and (2) chronic renal failure, in which there is progressive loss of function of more and more nephrons that gradually decreases overall kidney function