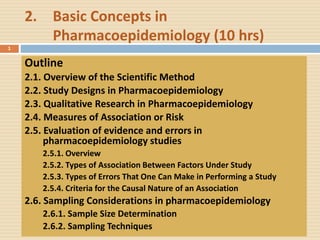
Ch 2 basic concepts in pharmacoepidemiology (10 hrs)
- 1. 2. Basic Concepts in Pharmacoepidemiology (10 hrs) Outline 2.1. Overview of the Scientific Method 2.2. Study Designs in Pharmacoepidemiology 2.3. Qualitative Research in Pharmacoepidemiology 2.4. Measures of Association or Risk 2.5. Evaluation of evidence and errors in pharmacoepidemiology studies 2.5.1. Overview 2.5.2. Types of Association Between Factors Under Study 2.5.3. Types of Errors That One Can Make in Performing a Study 2.5.4. Criteria for the Causal Nature of an Association 2.6. Sampling Considerations in pharmacoepidemiology 2.6.1. Sample Size Determination 2.6.2. Sampling Techniques 1
- 2. 2.1. Overview of the Scientific Method The whole point of science is to UNCOVER THE TRUTH Two tools to peruse SCIENTIFIC INQUIRY are 1. OUR SENSES – through which we experience the world and make observations 2. OUR ABILITY TO REASON – which enables us to make logical inferences 2
- 3. Scientific Method… In science we impose logic on observations There are two kinds of logic we impose: Deductive Inferences: From the GENERAL (theory) to the SPECIFIC, of the observations Involving inferences from general principles Inductive Inferences: Also called logic of reasoning From SPECIFIC to the GENERAL. Proceeding from particular facts to a general conclusion We make many observations Discern a pattern, Make generalizations, and Infer an explanation 3
- 4. Scientific Method… The scientific methods from the perspective of inductive approach is a three-stage process 1st stage: One studies a sample of study participants 2nd stage: One generalizes the information obtained from this sample of study participants Drawing a conclusion about a population in general → An association 3rd stage: One establishes causation → Making inferences 4
- 5. Example: One might perform a RCT of the efficacy of methyldopa in lowering BP, randomly allocating a total of 40 middle aged hypertensive men to receive either methyldopa or placebo and observing their BP six weeks later. One might expect that the BP of the 20 men treated with the active drug decrease more than the BP of 20 men treated with placebo. In this example The 40 study participants would represent the study sample One would make generalization that methyldopa lowers BP in middle aged hypertensive men (establishing association). One must further explore whether this observation is by chance or due to other factors. And further decide whether the association is casual in nature or not. 5 RCT- Randomized Controlled Trial
- 6. 6 Inductive Research Framework Ask Questions Do Background Research Construct Hypothesis Think! Try again Test with an Experiment Analyze Results, Draw Conclusion Hypothesis is TRUE Hypothesis is FALSE or Partially True Report Results
- 7. 2.2. Study Designs in Pharmacoepidemiology 7 Pharmacoepidemiology applies the methods of epidemiology to the content area of clinical pharmacology Different study designs can be applied within pharmacoepidemiology, all with their own Specific indications Advantages and Disadvantages
- 8. 8 Epidemiologic Study Designs Descriptive Case Series Case Report Ecologic Cross Sectional Analytic Non- Experimental Cohort Case-Control Experimental RCT Fig. Types of Epidemiologic Study Designs
- 9. 9
- 10. Hierarchy of Designs and Strength of Evidence 1. Randomized Controlled Trial (RCT) 2. Cohort: Prospective or Retrospective 3. Case Control- Prospective or Retrospective 4. Cross Sectional 5. Case Reports/Case Series 6. Systematic Reviews, Meta-Analysis: Secondary data analysis Strongest Evidence Weakest Evidence 10
- 11. Study Design Past Present Future Retrospective Cohort Prospective Cohort Case-Control (Retrospective) Cross-Sectional 11
- 12. Retrospective and Prospective Designs Retrospective Design The research question or hypothesis is conceived and studied using data that were collected and recorded previously (before the design of the current study). Prospective, or Longitudinal, Design The collection of data is planned in advance and actually occurs after the study has begun. 12
- 13. Comparison of Retrospective and Prospective Approaches Retrospective Prospective Inexpensive to conduct Expensive to conduct Completed in a shorter time period Completed over a longer time period Easier to access a larger number of subjects More difficult to access subjects and usually requires a larger number of subjects Allows results to be obtained more quickly Exposure status and diagnostic methods for disease may change Useful for studying exposures that no longer occur Loss of subjects from the study over time may be substantial Information and data may be less complete and inaccurate Information and data may be more complete and accurate Subjects may not remember past information Direct access to study subjects enhances reliability of data 13
- 14. Descriptive Studies A study in which explain the frequency and relative distributions of health and disease in populations Attempt to uncover and portray the occurrence of the condition or problem Useful in Signal detection Hypothesis generating Identifying previously unrecognised safety issues Explain the 5WH Questions (What, Who, Where, When, How much) Person Place Time model 14
- 15. The aspect of epidemiology concerned with the search for health problem-related causes and effects Determine causes or health problems Based on Natural exposure Use controls or comparison groups Focus on the determinants (causes) of diseases Ultimate goal is judging whether a particular exposure causes or prevents disease Test cause–effect relationships 15 Analytical Studies
- 16. Case Reports Case reports are simply reports of events observed in single patients In pharmacoepidemiology, A case report describes a single patient who was exposed to a drug and experiences a particular, usually adverse, outcome. (Individual Assignment 10%) Case reports are useful For raising hypotheses about drug effects, to be tested with more rigorous study designs. 16
- 17. Case Series Case series are collections of patients, all of whom have a single exposure, whose clinical outcomes are then evaluated and described. Examples Serious liver damage following use of XTC Birth defects after use of Thalidomide (Softenon) 17 XTC- Methylene dioxymethamphetamine (MDMA or 'Ecstasy')
- 18. 18 LETTER TO THE EDITOR McBride WG. The Lancet, December 16, 1961: page 1358
- 19. Ecological Studies (Correlational) The study of association between two factors Macro level study (can not imply with each individual) Studying the trend of health problems Examine trends in an exposure that is a presumed cause and trends in a disease that is a presumed effect and test whether the trends coincide. These trends can be examined over time or across geographic boundaries. Example: the association between amount of anti- asthma drug and the increase of asthma mortality among American people 19
- 20. Ecologic Studies: Breast Cancer Incidence by National Fat Intake (hypothetical example) 20 0 50 100 150 200 250 500 700 900 1100 1300 1500 1700 Fat intake (kcal/d) Incidence per 100,000 p-y Romania Yugoslavia Hong Kong Israel Italy Hungary Poland Spain Sweden UK N Zealand France Switzerland USA
- 21. Cross-Sectional Studies Prevalence study A study design that shows concurrently existing characteristics and health outcomes Information about the status of an individual with respect to the presence or absence of exposure and disease is assessed at a point in time. Cross sectional studies also show the picture of social, environmental, or other problems or events in a population. The point in time may be as short as few minutes or as long as two or three months. The time frame of "point in time" is based on the speed of data collection. 21
- 22. Case-Control Studies Comparing cases with a disease to controls without the disease, looking for differences in antecedent exposures. Comparing the diseased and non-diseased groups Look back in time to measure exposures of the study subjects Retrospective study Rare diseases Ex. Limb defect and Thalidomide in German babies 22
- 23. Case-control studies Cases Controls Population at Risk Exposed - b Unexposed - d Exposed - a Unexposed - c Cause Effect 23
- 24. Steps in conducting case control study Step 1: Define cases Step 2: Select cases Step 3: Select controls • The controls should be similar with the cases except that the cases have the disease or other outcome of interest. Step 4: Check the exposure status of individuals both in the cases and controls Step 5: Analysis • Prepare 2X2 table • Calculate Odds Ratio (OR) • Perform statistical tests to check whether there is significant association 24
- 25. Example case-control study What is the risk on breast cancer with the use of SSRI antidepressants? Cases: women with breast cancer Controls: women with no breast cancer Exposure: SSRIs 25
- 26. Coogan et al. Am J Epidemiol 2005 26
- 27. Case Control Exposure + a b - c d a + c b + d Odds of Exposed = a/b Odds of Non Exposed = c/d Odds Ratio (OR) = (a/b) / (c/d) = (a*d) / (b*c) RR Calculation OR 27
- 28. Rofecoxib and risk of MI Nested Case Control design: • 9218 MI cases of whom 93 used of rofecoxib < 3 months ago • 86349 controls, of whom 634 used of rofecoxib < 3 months ago MI control Rofecoxib + 93 634 - 9125 85715 OR (MI)= 93x85715 / 634x9125 = 1.38 BMJ 2005;330:1366 28
- 29. Selection of cases Establish strict diagnostic criteria for the outcome: Examples: Type 1 diabetes in children: severe symptoms, very high BG, marked glycosuria, and ketonuria. Type 2 diabetes: few if any symptoms, Slightly elevated BG, diagnosis “complicated”. 29
- 30. Selection of cases Population-based cases: include all subjects or a random sample of all subjects with the disease at a single point or during a given period of time in the defined population: Disease registers Hospital-based cases: All patients in a hospital department at a given time 30
- 31. Selection of Controls Principles of Control Selection: Study base: Controls can be used to characterise the distribution of exposure Comparable-accuracy Equal reliability in the information obtained from cases and controls no systematic misclassification Overcome confounding Elimination of confounding through control selection matching or stratified sampling 31
- 32. Selection of Controls General population controls: registries, households, telephone sampling costly and time consuming recall bias eventually high non-response rate Hospitalised controls: Patients at the same hospital as the cases Easy to identify Less recall bias Higher response rate 32
- 33. Ascertainment of outcome and exposure status External sources: Death certificates, disease registries, Hospital and physicians records etc. Internal sources: Questionnaires and interviews, information from a surrogate (spouses or mother of children), biological sampling( e.g. antibody) 33
- 34. Strengths Quick, inexpensive Well-suited to the evaluation of diseases with long latency period Rare diseases Examine multiple etiologic factors for a single disease Limitations Not rare exposure Incidence rates cannot be estimated unless the study is population based Selection Bias and recall bias 34 Strengths and Limitations of Case-Control
- 35. Cohort Studies Are studies that identify subsets of a defined population and follow them over time, looking for differences in their outcome. Cohort studies generally are used to compare exposed patients to unexposed patients Although they can also be used to compare one exposure to another. The design best allows for estimates of the probability or risk of developing the outcome The exposed or not exposed to a particular risk factors Measuring incidence The best design of observational studies that can explain causation of health problems 35
- 36. Cohort study / Follow-up study Study population Exposed Non-exposed Disease + Disease + Disease - Disease - Cause Effect 36
- 37. Strengths and Limitations of Cohort Study Strength Rare exposure Examine multiple effects of a single exposure Minimizes bias in the exposure determination Direct measurements of incidence of the disease Limitation Not rare diseases Prospective: Expensive and time consuming Retrospective: in adequate records Validity can be affected by losses to follow-up 37
- 38. Steps in conducting cohort study Step 1: Define exposure Step 2: Select exposed group Step 3: Select non-exposed group Step 4: Identify sources of data for exposure and outcome Step 5: Collect data Step 6: Analyze data • Prepare 2X2 table • Calculate Relative Risk (RR) • Perform statistical tests to check whether there is statistical significant association 38
- 39. Concurrent VS Retrospective Cohort Prospective or 39
- 40. Frequency measures cohort study (P1 personyears) (P0 personyears) A1 A0 Exposure No Exposure Disease Disease No disease Time Time No disease (B1) (B0) 40
- 41. Frequency measures Incidence Cumulative incidence (CI) Incidence rate (IR) 41
- 42. Risk disease + | exposure + = A1 / N1 = CI1 Risk disease + | exposure - = A0 / N0 = CI0 Frequency measures cohort study Disease No disease Total Exposure + A1 B1 N1 - A0 B0 N0
- 43. Force of morbidity | exposure + = A1 / P1 = IC1 Force of morbidity | exposure - = A0 / P0 = IC0 Frequency measures cohort study Disease Person-years Exposure + A1 P1 - A0 P0
- 44. Effect measures cohort study Risk difference RD CI1 – CI0 IC1 - IC0 Relative Risk RR CI1 / CI0 IC1 / IC0 Attributable Risk AR (CI1 - CI0) / CI1 (IC1-IC0) / IC1 Relative Risk Reduction RRR 1 – RR Number needed to treat NNT 1 / RD 44
- 45. Pill and Deep Venous Thrombosis Risk no pill = 3.9 per 100 000 py Risk pill gen. 2 = 10.3 per 100 000 py Risk pill gen. 3 = 21.3 per 100 000 py RR2/3 = 2.07 RV2/3 = 11.0 per 100 000 py AR2/3 = 52% ‘NNH’2/3 = 9091 per year Lancet 1995; 346: 1582 - 1588 45
- 46. Prospective vs. Retrospective Cohort Studies Prospective Cohort Studies Time consuming, expensive More valid information on exposure Measurements on potential confounders Retrospective Cohort Studies Quick, cheap Appropriate to examine outcome with long latency periods Admission to exposure data Difficult to obtain information of exposure Risk of confounding 46
- 47. Selection of the Exposed Population Sample of the general population: Geographically area, special age groups, birth cohorts (Framingham Study) A group that is easy to identify: Nurses health study Special population (often occupational epidemiology): Rare and special exposure Permits the evaluation of rare outcomes 47
- 48. Selection of the Comparison Population Internal Control Group Exposed and non-exposed in the same study population (Framingham study, Nurses health study) Minimise the differences between exposed and non-exposed External Control Group Chosen in another group, another cohort (Occupational epidemiology: Asbestosis vs. cotton workers) The General Population 48
- 49. Applications of different observational designs Application Ecological X-sectional Cohort Case-control Rare disease ++++ - - +++++ Rare exposure ++ - +++++ - Test multiple + ++ +++++ - effects Study multiple ++ ++ +++ ++++ exposures Time relationship ++ - +++++ + Direct measure - - +++++ + of incidence 49
- 50. Bias, Cost, and Time Ecological X-sectional Cohort Case-control Probability of; Selection bias - medium low high Recall bias - high low high Loss of follow up - - high low Confounding high medium low medium Time required low medium high medium Cost low medium high medium 50
- 51. Experimental/Intervention studies Longitudinal in design There is random allocation of subjects to either group Treatment & Control group Individuals are allocated by the investigator Artificial manipulation of study factors Can produce high quality data 51
- 52. Classification based on the population studied 1. Clinical trial • Usually performed in clinical settings and the subjects are patients 2. Field trial • Used in testing medicine for preventive purpose • Subjects are healthy people e.g. vaccine trial 3. Community trial • Unit of the study is group of people/community e.g. Fluoridation of water to prevent dental caries 52 Experimental/ Intervention studies
- 53. Classification based on objective 1. Phase I Trial on small subjects to test a new drug with small dosage to determine the toxic effect 2. Phase II Trial on small group to determine the therapeutic effect 3. Phase III Study on large population Usually randomized controlled trial 53 Experimental/ Intervention studies
- 54. Source population Randomisation Index group Control group Follow-up Follow-up Outcome Outcome In- and exclusion criteria Method, blinding Prognostically comparable Treatment Double blind Loss-to-follow-up Blinded measurement of outcome 54
- 55. Experimental/ Intervention studies In a clinical trial, the experimental group receives the drug or treatment to be evaluated, while the control group receives A placebo, no treatment, or The standard of care. Both groups are followed for the outcome(s) of interest. Hawthorne effect: Even “inert” treatments might result in significant improvements in the patient’s condition. 55
- 56. Crossover Design A crossover study is a special design of controlled intervention study that is sometimes used in drug trials. In this design, half of the participants are randomly assigned to start with the placebo and then switch to active treatment, while the other half does the opposite. 56
- 57. Advantages and Disadvantages of Crossover Study design (RCT) Advantages: It reduces the number of subjects required, since each subject serves as both an experimental subject and a control It decreases the biological variability inherent in comparing different subjects by comparing each subject with himself or herself Disadvantages: Increases the duration of the study Carry-over effect Fatigue 57
- 58. Quasi-Experimental Designs Artificial manipulation of the study factor without randomization (e.g. program evaluation) One group (Internal) comparison Each experimental unit serves as its own control The control will be past experience historical (before and after study) Multiple group (External) comparison Treatment or intervention group compared to control or comparison groups. 58
- 59. Quasi-Experimental Designs Designs with Historic Control A before and after study is a method of control in which results from experimental subjects are compared with outcomes from patients treated before the new intervention was available. These are called historic controls. 59
- 60. Advantages and limitation of RCT (Experimental studies) Advantages Gold standard for therapeutic evaluation The Gold standard is achieved through Randomization Blindness Use of placebo Limitations Ethical considerations (e.g. smoking, birth defects) Feasibility/Practical issues (e.g. rare adverse effects) Cost 60
- 61. Table: Advantages and disadvantages of epidemiologic study designs 61
- 62. 2.3. Qualitative Research in Pharmacoepidemiology Presentation Outline 2.3.1. Introduction 2.3.2. Qualitative Research Designs and Methods 2.3.3. Methods of data collection 2.3.4. Sampling strategies in qualitative research 2.3.5. Qualitative Methods of Analysis 2.3.6. Trustworthiness 62
- 63. Learning Objectives Define qualitative research List key features of qualitative research Describe basic design questions in qualitative research methods, Identify different methods used for addressing different research questions Describe sampling strategies used in qualitative approaches Discuss on thrust worthiness of qualitative methods 63
- 64. 2.3.1. Introduction Definition Qualitative research is a type of formative research that offers specialized techniques for obtaining in- depth responses about what people think and how they feel. It enables programme management to gain insight into attitudes, beliefs, motives and behaviors of the target population. 64 Formative research is the process by which researchers or public health practitioners define a community of interest, determine how to access that community, and describe the attributes of the community that are relevant to a specific public health issue.
- 65. Why qualitative research? Qualitative research: Provides greater depth of response and, therefore, greater consequent understanding than can be acquired through quantitative techniques. Good source of descriptions and explanations of processes in identifiable local contexts. Describe chronological flow, which events led to which consequences and derive fruitful explanations. Could help researchers to get beyond initial conceptions and to generate or revise conceptual frameworks. Well suited for locating meanings people place on events, processes, and structures of their lives and for connecting these meanings to the social world. 65
- 66. Why qualitative research? Qualitative research (cont..) Deals with emotional and contextual aspects of human response rather than with objective measurable behaviors and attitudes. Can be designed to explore concepts, develop hypotheses or theories, develop research tools, and clarify the findings of a quantitative study. 66
- 67. Why qualitative research? There are three domains in which qualitative research tends to be used in public health: 1. First domain includes economic, political, social and cultural, environmental and organizational factors which influence health. 2. Second domain focuses on gaining understanding of how people make sense of their experiences of health and disease. 3. Third domain includes interaction of actors involved in different public health activities. 67
- 68. How is Qualitative research used? Qualitative research is used largely in four general ways as: 1. Tool to generate ideas 2. Step in developing a quantitative study 3. Aid in evaluating a quantitative study 4. Primary data collection method for a research topic 68
- 69. Difference between qualitative and quantitative researches Qualitative Quantitative Provides depth of understanding Measures level of occurrence Asks why? Asks how many? How often? Studies motivations Studies action Is subjective Is objective Enables discovery Provides proof Is exploratory Is definitive Allows insights into behavior, trends and so on Measures level of actions, trends, and so on Interprets Describes Inductive Deductive 69
- 70. Characteristics of qualitative research Qualitative research methods have many distinguishing characteristics. 1. Qualitative methods take the views of informants, whereas quantitative research takes the ideas of the researcher as points of departure. 2. Lines of reasoning in both methods differ. In quantitative research is deductive Typically starting with the generation of a hypothesis based on existing theory, then testing of hypothesis against existing reality In qualitative method is inductive Qualitative researchers may also test emerging hypotheses or theories against data, and thus oscillate between data and theory. 70
- 71. Characteristics of qualitative research 3.Concerned with reliability and validity. Strength of the quantitative approach lies in its reliability (repeatability) that is the same measurements should yield the same results time after time, Strength of qualitative research lies in validity (closeness to the truth) that is good qualitative research should touch the core of what is going on rather than just skimming the surface. Validity of qualitative methods is greatly improved by a process known as triangulation and by independent analysis of the data by two or more researchers. 71
- 72. 2.3.2. Qualitative Research Designs and Methods Qualitative research has its own designs and methods. There are four major types of qualitative research designs 1. Phenomenology 2. Ethnography 3. Grounded theory 4. Case study 72
- 73. Phenomenology Phenomenology literally means the study of phenomena. It is a way of describing something that exists as part of the world in which we live. Phenomena may be Events, Situations, Experiences or concepts. 73
- 74. Phenomenology Phenomenological research begins with the acknowledgement that there is a gap in our understanding and that clarification or illumination will be of benefit. Phenomenological research will not necessarily provide definitive explanations but it does raise awareness and increases insight. 74
- 75. Ethnography Ethnography is “[an] analytical description of social scenes and groups that recreate for the reader the shared beliefs, practices, artifacts, folk knowledge, and behaviors of those people.” Goetz and LeCompte (1984, pp. 2-3) Ethnography has a background in anthropology. The term means “portrait of a people” and it is a methodology for descriptive studies of cultures and peoples. The cultural parameter is that the people under investigation have something in common. 75
- 76. Ethnography Rooted in anthropology, ethnography involves the study of an intact group, logically defined, in its natural context for a sustained time interval. The researcher is typically an observer or a participant observer (Creswell, 1994, p. 11). Examples of parameters include: geographical - a particular region or country Religious Tribal shared experience 76
- 77. Ethnography In health care settings, researchers may choose an ethnographic approach because the cultural parameter is suspected of affecting the population’s response to care or treatment. For example, cultural rules about contact between males and females may contribute to reluctance of women from an Asian subgroup to take up cervical screening. Ethnography helps health care professionals to develop cultural awareness and sensitivity and enhances the provision and quality of care for people from all cultures. 77
- 78. Ethnography Ethnographic studies entail extensive fieldwork by the researcher. Data collection techniques include both formal and informal interviewing, often interviewing individuals on several occasions, and participant observation. Because of this, ethnography is extremely time consuming as it involves the researcher spending long periods of time in the field. 78
- 79. Ethnography Ethnographic research is very labor and time intensive, involving extensive fieldwork in a natural setting. Usually a general research question(s) is (are) identified. Once entry is gained and rapport (or trust) is established, the research questions are continually refined becoming more focused. It is not uncommon for the larger research question(s) to be segmented into more numerous, focused ones. 79
- 80. Grounded theory This methodology originated with Glaser and Strauss and their work on the interactions between health care professionals and dying patients. The main feature is the development of new theory through the collection and analysis of data about a phenomenon. It goes beyond phenomenology because the explanations that emerge are genuinely new knowledge and are used to develop new theories about a phenomenon. In health care settings, the new theories can be applied enabling us to approach existing problems in a new way. 80
- 81. Case study Case study research is used to describe an entity that forms a single unit such as a person, an organization or an institution. Some research studies describe a series of cases. 81
- 82. 82 Dimension Narrative Phenomenology Grounded Theory Ethnography Case Study Focus •Exploring the life of an individual • Understanding the essence of experiences about a phenomenon • Developing a theory grounded from data in the field • Describing and interpreting a cultural or social group • Developing an in-depth analysis of a single case or multiple cases Data Collection • Primary interviews and documents • Long interviews with up to 10 people • Interviews with 20-30 individuals to “saturate” categories and detail a theory • Primarily observations and interviews with additional artifacts during extended time in the field (e.g. 6 months to a year) • Multiple sources including documents, archival records, interviews, observations, • Physical artifacts Data Analysis • Stories • Epiphanies • Historical content • Statements • Meanings • Meaning themes • General description of the experience • Open coding • Axial Coding • Selective Coding • Conditional Matrix • Description • Analysis • Interpretation • Description • Themes • Assertions Narrative Form • Detailed picture of an individual’s life • Description of the “essence” of the experience • Theory or theoretical model • Description of the cultural behavior of a group or an individual • In-depth study of a “case” or “cases”
- 83. 2.3.3. Methods of data collection The most common methods of data collection in qualitative research are: 1. Participant observation Overt observation Covert observation 2. Interviews (Unstructured, Semi-structured, Structured) Face to face interviews Telephone interviews 3. Focus groups researcher(s) plus 2-10 participants - guided group discussion on topic(s) 4. Historical methods 83
- 84. Design questions in qualitative research Qualitative research can address questions What is the society like? Why do certain behaviors occur? What is this experience like? 84
- 85. Design questions in qualitative research The following points discuss some of the key design questions necessary in designing qualitative research 1. Defining an area of inquiry Drawn from personal experience, reviewing literature and auditing earlier studies. 2. Stating the research problem Entails gap in scientific knowledge Helps to describe what has been done so far and identify questions that have been unanswered. Forwards the ways in which the findings of the present study might be utilized 85
- 86. Design questions in qualitative research 3.Developing a conceptual framework It is an alternative way of depicting a set of related variables and outcomes in the study in an elaborative schematic diagram. It shows the key factors, presumed relationships and possible outcomes of the research problem. It helps to outline the research questions and core variables included in the data collection instrument. 86
- 87. Design questions in qualitative research 4. Formulating qualitative research questions A thoroughly defined research problem helps to examine the issue with more specific and relevant questions. Research questions serve to narrow the purpose. There are two types: 1. Central The most general questions you could ask 2. Sub-questions Subdivides central question into more specific topical questions Limited number 87
- 88. Design questions in qualitative research Use good qualitative wording for questions. Begin with words such as “how” or “what” Tell the reader what you are attempting to “discover,” “generate,” “explore,” “identify,” or “describe” Ask “what happened?” to help craft your description Ask “what was the meaning to people of what happened?” to understand your results Ask “what happened over time?” to explore the process 88
- 89. 2.3.4. Sampling strategies in qualitative research Does not need to be representative of population - not statistical Saturation – recruitment of additional cases no longer provides additional information or insights The sampling techniques used in qualitative research are: 1. Purposeful sampling 2. Homogeneous sampling 3. Theoretical sampling 4. Extreme or deviant 5. Maximum variation 6. Convenience sampling 7. Snowball or chain sampling 8. Opportunistic 89
- 90. Sampling strategies in qualitative research Purposive sampling Also known as judgemental sampling, purposive sampling is a non-probability technique that involves the conscious selection by the researcher of certain people to include in a study. Participants are selected because they have particular characteristics that are of interest to the researcher. For example, they have had the experience in which the researchers are interested, or there are certain aspects of their lives in which the researchers are interested. 90
- 91. Sampling strategies in qualitative research Homogeneous sampling includes people with basically similar characteristics to study the group in depth. The selection of participants is usually done within certain strata; participants with similar demographic or social characteristics being included in the same strata. Focus groups usually use this type of sampling. The group interaction stimulates people within the group to discuss their experiences. The main advantage of homogeneous sampling is that it focuses on a similar type of respondents thereby simplifying analysis and group interviewing 91
- 92. Sampling strategies in qualitative research Theoretical sampling It is the process of selecting "incidents, slices of life, time periods, or people on the basis of their potential manifestation or representation of important theoretical constructs" (Patton, 2001, p. 238). Theoretical sampling is an important component in the development of grounded theories. Glaser and Strauss (1967) describe an iterative sampling process that is based on emerging theoretical concepts. This sampling approach has the goal of developing a rich understanding of the dimensions of a concept across a range of settings and conditions. Extreme or deviant chooses extreme cases of outstanding successes or crisis events after knowing the typical case in order to highlight and understand the situation. For example, a researcher may be interested in studying two health facilities, one whose family planning clients are highly satisfied and another whose clients are not satisfied, in order to identify factors that favor or discourage the utilization of services. This type of sampling is valuable to test emerging theories by learning from highly unusual manifestations. 92
- 93. Sampling strategies in qualitative research Maximum variation Also known as heterogeneous sampling. Useful for obtaining maximum differences among information-rich informants or group. Subjects included in the study are different from each other based on predetermined criteria. E.g. A study of rural, urban and suburban or merchants and academicians or high activity/low activity college students, etc. Convenience sampling Study participants are selected based on their ease, accessibility and availability. Researcher selects those individuals who are most readily available. Helps to save time, money and effort. However, it may be the weakest sampling scheme due to its low credibility. 93
- 94. Sampling strategies in qualitative research Snowball or chain sampling depends on locating participants by asking others to identify individuals or groups with rich information on the phenomenon under study. implies that the first subject is used to identify the next person or group to facilitate the identification of cases of interest. the sample gradually increases in size, like a snowball being rolled down a hill. Valuable when the researcher is new to the study site, and also important for identifying individuals who have rich information but are difficult to reach. Opportunistic Additional study subjects may be selected to take advantage of unexpected opportunities at the field level. 94
- 95. 2.3.5. Qualitative Methods of Analysis 1. Thematic analysis Focuses on identifiable themes and patterns of living and/or behaviour. From the conversations that take place in a therapy session or those that are encouraged for the sake of researching a process, ideas emerge that can be better understood under the control of a thematic analysis. 2. Content Analysis Is doing the word-frequency count. assumption made is that the words that are mentioned most often are the words that reflect the greatest concerns. 3. Discourse Analysis Discourse analysis focuses on talk and texts as social practices, and on the resources that are drawn on to enable those practices. 95
- 96. 2.3.6. Trustworthiness Ensuring the quality of data based on certain established criteria is the main activity of the researcher both in qualitative and quantitative research traditions. Particularly for qualitative research, where the challenge of understanding and making meaning is put upon the researcher. 96
- 97. Trustworthiness There are four common criteria for assessing trustworthiness of qualitative research findings are: 1. Truth value/Credibility 2. Applicability/Transferability 3. Consistency/Dependability 4. Neutrality/Confirmability 97
- 98. Trustworthiness Truth value/Crediblity • It refers to the ability of the study to detect what the research really aimed at studying. • It asks whether the researcher has established confidence in the truth of the findings for the subjects or informants and the context in which the study was undertaken (Lincoln & Guba, 1985). 98
- 99. Trustworthiness Applicability/Transferability • Applicability refers to the ability to determine the extent to which the findings are applicable in other settings, situations, populations or circumstances. 99
- 100. Trustworthiness Consistency • The basic question asked by researchers while dealing with consistency is “can the findings be repeated with the same (or similar) respondents in the same context?” • Consistency of findings in both quantitative and qualitative research designs can be explained by reliability and dependability, respectively. 100
- 101. Trustworthiness Neutrality • It refers to the role of the researchers mainly during data collection. • It is assessed by objectivity in quantitative research and conformability in qualitative approach. 101
- 102. Trustworthiness 102 Conventional inquiry Naturalistic inquiry Methods to ensure quality Internal validity Credibility Member checks; prolonged engagement in the field; data triangulation External validity Transferability Thick description of setting and/or participants Reliability Dependability Audit– researcher’s documentation of data, methods and decisions; researcher triangulation Objectivity Confirmability Audit and reflexivity Table 1 – Lincoln and Guba’s translation of terms
- 103. Trustworthiness 103
- 104. Trustworthiness 104
- 105. 2.4. Measures of Association or Risk 2.4.1. Introduction to risk and harm 2.4.2. Methods of Risk Measures 105
- 106. Learning Objectives Define risk, harm, hazard and risk assessment List risk measure methods Differentiate types of risk measures Interpret and apply risk estimates 106
- 107. 2.4.1. Introduction to risk and harm Definitions Risk 1. It is the probability that an event will occur, e.g., that an individual will become ill or die within a stated period of time or by a certain age. Lasts Dictionary of Epidemiology 2. It is hazard probability that an event will occur at a time t when it has not occurred at time t-1. In pharmacoepidemiology, this term designates the probability that a subject (whether exposed to a drug or not) will present an event at any given time, knowing that the subject had not presented it in the preceding time interval. Dictionary of Pharmacoepidemiology 107
- 108. 2.4.1. Introduction …(continued) Harm Harm is the nature and extent of actual damage that could be caused by a drug. Hazard 1. It is the potential to cause harm. 2. It refers to a property or situation that in particular circumstances could lead to harm (Royal Society, 1992). Royal Society (1992). Risk Analysis, Perception and Management. The Royal Society, London 108
- 109. 2.4.1. Introduction …(continued) Risk assessment It is the procedure in which the risks posed by inherent hazards involved in processes or situations are estimated either quantitatively or qualitatively. 109
- 110. 2.4.2. Methods of Risk Measures Risk measures are estimates that describe amount of risk associated with particular exposure in sample population Risk estimates can Describe quantitatively risk associated with particular exposure and development or prevention of disease Quantify association between exposure to particular drug and adverse drug reaction 110
- 111. 2.4.2. Methods of Risk … Risk estimates are part of our daily lives Measures of risk are communicated to Patients via Newspapers Television Internet Practitioners via Studies published in medical journals Thus, risk measures are important in clinical decision-making process for both patients and practitioners. 111
- 112. 2.4.2. Methods of risk … Understanding of risk measures is important to Interpret appropriately Apply the estimates Risk measures are difficult to use for many reasons: 1. When conflicting results reported from different studies When conflicting information pertaining to risk is published It becomes difficult for both practitioners and patients to use risk estimates for clinical decision-making 2. When confusion in interpretation of results of study exists on risk estimates Two readers may interpret, communicate, and use the results of a study very differently 112
- 113. Risk Measure Types 1. Prevalence 2. Incidence 3. Relative Risk 4. Odds Ratio 5. Attributable Risk (Risk difference) 6. Attributable Risk Percent 7. Number Needed to Treat 113
- 114. Prevalence Prevalence (P) is defined as the number of existing cases of disease (or any outcome, e.g., adverse drug reaction, drug use) in a population at a particular point in time. 114 P = 𝑵𝒖𝒎𝒃𝒆𝒓 𝒐𝒇 𝒆𝒙𝒊𝒔𝒕𝒊𝒏𝒈 𝒄𝒂𝒔𝒆𝒔 𝒊𝒏 𝒂 𝒑𝒐𝒑𝒖𝒍𝒂𝒕𝒊𝒐𝒏 𝑻𝒐𝒕𝒂𝒍 𝒏𝒖𝒎𝒃𝒆𝒓 𝒐𝒇 𝒑𝒆𝒐𝒑𝒍𝒆 𝒊𝒏 𝒕𝒉𝒂𝒕 𝒑𝒐𝒑𝒖𝒍𝒂𝒕𝒊𝒐𝒏
- 115. Prevalence Types of prevalence 1. Point prevalence rate comprises all the cases of a disease that exist at a point in time. 2. Period prevalence Numerator is all cases whether old, new or recurrent, arising over a defined period, say a year or two. Denominator is the average population over the period (or mid-point estimate) 3. Lifetime prevalence Proportion of the population who have ever had the disease 115
- 116. Incidence Incidence refers the number of new cases of disease that develop in a population at risk over a specified time period. Incidence is used to determine how often the disease is occurring. Incidence is typically described as either Cumulative incidence (CI) or incidence rate Person-time rate 116
- 117. Incidence Cumulative incidence (CI) CI assumes that all of the subjects were followed for the entire study period. CI does not reflect study dropouts or losses to follow-up. 117 CI = 𝑵𝒖𝒎𝒃𝒆𝒓 𝒐𝒇 𝒏𝒆𝒘 𝒅𝒊𝒔𝒆𝒂𝒔𝒆 𝒄𝒂𝒔𝒆𝒔 𝒅𝒖𝒓𝒊𝒏𝒈 𝒈𝒊𝒗𝒆𝒏 𝒕𝒊𝒎𝒆 𝑻𝒐𝒕𝒂𝒍 𝒑𝒐𝒑𝒖𝒍𝒂𝒕𝒊𝒐𝒏 𝒂𝒕 𝒓𝒊𝒔𝒌
- 118. Incidence Incidence Rate IR is also referred as incidence density It is more accurate means of measuring disease occurrence. IR takes into account actual observation time of each subject during study period It does not assume all subjects were followed for the entire study period. 118 IR = 𝑵𝒖𝒎𝒃𝒆𝒓 𝒐𝒇 𝒏𝒆𝒘 𝒄𝒂𝒔𝒆𝒔 𝒅𝒖𝒓𝒊𝒏𝒈 𝒈𝒊𝒗𝒆𝒏 𝒕𝒊𝒎𝒆 𝑻𝒐𝒕𝒂𝒍 𝒑𝒆𝒓𝒔𝒐𝒏 𝒕𝒊𝒎𝒆 𝒐𝒇 𝒐𝒃𝒔𝒆𝒓𝒗𝒂𝒕𝒊𝒐𝒏 𝒊𝒏 𝒑𝒐𝒑𝒖𝒍𝒂𝒕𝒊𝒐𝒏 𝒂𝒕 𝒓𝒊𝒔𝒌 × 𝟏𝟎𝒏 n- 1, 2, 3
- 119. Incidence Example: Sample of population recruited= 100 persons Incidence of side effects Study period- 3years After one year- 5 persons- 100 person year (py) After two years-10 persons- 95 py After three years-15 persons- 85 py 119 IR = 𝟓+𝟏𝟎+𝟏𝟓 𝟏𝟎𝟎+𝟗𝟓+𝟖𝟓 × 𝟏𝟎𝟑 = 𝟑𝟎 𝟐𝟖𝟎 𝒑𝒆𝒓𝒔𝒐𝒏 𝒚𝒆𝒂𝒓 × 𝟏𝟎𝟑 = 𝟏𝟎𝟕 per 1000 person-year 107 people on side effects per 1000 person-year of observation
- 120. Incidence 2 by 2 Contingency Table 120 Disease/ Outcome Yes No Total Exposure Yes A B A + B No C D C + D Total A + C B + D A+ B + C +D
- 121. Relative Risk Relative risk (RR) is the likelihood of developing the disease in the exposed group relative to the unexposed group; It measure association between exposure and disease. Once incidence of an outcome or disease has been measured in both exposed and unexposed groups, useful to know relationship between exposure and development of disease 121
- 122. Relative Risk RR is simply a ratio of CI in exposed group over unexposed group It can be calculated as follows: Ho in a comparison of two groups states that proportion of subjects with outcome of interest is equal in exposed and unexposed groups. In other words, RR equals 1. 122 𝑹𝑹 = 𝑪𝑰 𝒆𝒙𝒑𝒐𝒔𝒆𝒅 𝑪𝑰𝒖𝒏𝒆𝒙𝒑𝒐𝒔𝒆 = 𝑨/(𝑨+𝑩) 𝑪/(𝑪+𝑫)
- 123. Relative risk RR can be used to measure association between exposure and outcome in Cohort studies Clinical trials RR is not used in context of a case-control study. 123
- 124. Relative risk Table. Interpretation of Relative Risk Relative Risk Risk Association between Exposure and Outcome 1 No association < 1 Negative association/Decreased risk > 1 Positive association/Increased risk 124
- 125. Odds Ratio Odds is the ratio of the probability of occurrence of an event to that of nonoccurrence. Odds ratio (OR) is a means of estimating the relative risk in case-control studies. In case-control studies, subjects are chosen based on disease status and then compared for rates of exposure. 125
- 126. Odds ratio OR is used to estimate RR in a case-control study. The odds ratio is calculated as follows: Null hypothesis when using the OR states, H0: OR =1. 126 𝑶𝑹 = odds of exposure among cases odds of exposure among controls = 𝑨/𝑩 𝑪/𝑫 = 𝑨𝑫 𝑩𝑪
- 127. Odds ratio Table. Interpretation of Odds Ratio Odds Ratio Association between Exposure and Outcome 1 No association between exposure and outcome < 1 Negative association/Decreased risk/ Protective effect > 1 Positive association/Increased risk -an increased risk of outcome associated with the exposure. 127
- 128. Confidence Intervals (CI) Confidence intervals are defined as the range within which the true effect lies with a certain degree of assurance. Confidence intervals determine the reliability of the risk estimate obtained in the sample. 128
- 129. Confidence intervals The 95% confidence intervals of the relative risk and odds ratio can be calculated as follows: 129 𝑪𝑰 𝒇𝒐𝒓 𝑶𝑹 = 𝒆𝒙𝒑 𝒍𝒏(𝑶𝑹) ± 𝒁𝜶/2 𝟏 𝒂 + 𝟏 𝒃 + 𝟏 𝒄 + 𝟏 𝒅 𝑪𝑰 𝒇𝒐𝒓 𝑹𝑹 = 𝒆𝒙𝒑 𝒍𝒏(𝑹𝑹) ± 𝒁𝜶/2 𝟏 − 𝒂 𝒂 + 𝒃 𝒂 + 𝟏 − 𝒄 𝒄 + 𝒅 𝒄
- 130. Confidence intervals (CI) The confidence interval can be calculated at various degrees of confidence (e.g. 90%, 95%,99%). Confidence intervals are most frequently reported at the 95% level, corresponding with a z-value of 1.96. 130 Confidence interval Z-value (Z/2) 90% ( = 0.1) 1.64 95% ( = 0.05) 1.96 99% ( = 0.01) 2.58
- 131. Confidence intervals (CI) Consider the results of three different studies. The relative risk and the corresponding 95% confidence interval for each study were as follows: Studies 1 and 2 shows statistically significant result because the number 1 is not included within the bounds of the 95% confidence interval 131 Study 1 RR = 2.2; 95% CI (1.8, 2.6) Study 2 RR = 2.2; 95% CI (1.1, 3.3) Study 3 RR = 2.2; 95% CI (0.9, 3.0)
- 132. Attributable Risk or Risk difference Attributable risk (AR) or risk difference (RD) is another measure of risk used in studies. AR provides information on absolute effect of the exposure. AR describes excess risk of disease in those exposed compared with those who were unexposed. 132
- 133. Attributable risk or risk difference AR is calculated as follows: AR allows to determine how morbidity and mortality are affected by removing the exposure. AR of 0 is equal to the null hypothesis and means there is no association between exposure and outcome. AR provides information on the type of effect that can be achieved by decreasing or eliminating the exposure. 133 𝑨𝑹 = 𝑪𝑰 𝒆𝒙𝒑𝒐𝒔𝒆𝒅 − 𝑪𝑰 𝒖𝒏𝒆𝒙𝒑𝒐𝒔𝒆𝒅 = 𝐴 𝐴+𝐵 - 𝐶 𝐶+𝐷
- 134. Attributable Risk Percent AR can be converted to the attributable risk percent (AR%), which may be easier to interpret. AR% provides an estimate of the proportion of the disease among the exposed that is attributable to the exposure. Like the AR, it provides information pertaining to the proportion of the disease in the exposed group that could be prevented by eliminating the exposure. 134
- 135. Attributable Risk Percent The attributable risk percent is calculated as follows: 135 𝐀𝐑% = CIexposed − CI unexposed CIexposed × 100 AR% = A A+B − C C+D A A+B × 100
- 136. Number Needed to Treat (NNT) Refers number of patients who would need to be treated (NNT), to prevent one clinical event or adverse outcome such as one death. Like the attributable risk, the number needed to treat is used by administrators to allocate health resources. 136
- 137. Number needed to treat It can be calculated as follows: Example If the mortality rate because of disease A in the untreated group is 17% and mortality in the treated group by using Drug X is 12%. Calculate NNT to prevent one death. Solution: NNT = 1/ (17%- 12%) = 1/0.05 = 20 people 137 𝐍𝐍𝐓 = 𝟏 𝐀𝐑 = 𝟏 𝐂𝐈 𝐞𝐱𝐩𝐨𝐬𝐞𝐝 − 𝐂𝐈 𝐮𝐧𝐞𝐱𝐩𝐨𝐬𝐞𝐝 = 𝟏 𝐀 𝐀 + 𝐁 − 𝐂 𝐂 + 𝐃
- 138. Summary Measures of risk allow the quantification of degree of risk associated with any number of exposures. Risk estimates are point estimates, the estimates obtained in the particular study population. Risk estimates may or may not represent the true, or actual, risk that exists in the general population. When evaluating risk estimates, it is important to consider baseline risk of developing the disease. evaluate confidence intervals around the risk estimate to determine the stability of the risk estimate. consider other factors that may be responsible for the disease, including confounding variables. 138
- 139. 2.5. Evaluation of Evidence and Errors in Pharmacoepidemiology Studies 2.5.1. Types of Association Between Factors Under Study 2.5.2. Types of Errors That One Can Make in Performing a Study 2.5.3. Criteria for the Causal Nature of an Association 139
- 140. 2.5.1. Types of Association Between Factors Under Study There are four basic types of associations that can be observed in a study: 1. No Association (independent) 2. Artefactual Association (Spurious or False) a. Chance (Unsystematic Variation) b. Bias (Systematic Variation) 3. Indirect Association(Confounded Association) 4. Causal Association (Direct or True) The basic purpose of research is to differentiate among them. 140
- 141. Hypothesis Testing Establishing associations requires hypothesis testing There are Two Types of Hypothesis in the scientific investigation: Null Hypothesis (Ho) and Alternative Hypothesis (HA) The hypothesis we test statistically is called the null Hypothesis 141
- 142. Hypothesis Testing Example: Suppose we are testing the efficacy of a new drug on patients with myocardial infraction 1. We divide the patients in to two groups: drug and no drug 2. Measure Mortality in the two groups 3. We say our hypothesis That the drug makes no difference and What we hope to do is to reject the ‘no difference’ hypothesis, based on evidence from our sample patients 142
- 143. 4. We specify our test hypothesis as follows: Ho (hypothesis): death rate in group treated with Drug A = death rate in group treated with Drug B That is equivalent to say: Ho: death rate in group A – death rate in group B = 0 We test this against an alternate hypothesis known as HA, The difference in death rate between the two groups does not equal to 0 That is equivalent to say: HA: death rate in group A – death rate in group B 0 143
- 144. If the observed difference is sufficiently greater than zero difference, We reject the null hypothesis. If we reject the null hypothesis of no difference, We accept the alternate hypothesis We can never be certain that we are right in either accepting or rejecting a hypothesis because of errors that can be produced in a study 144
- 145. 2.5.2. Types Of Errors That One Can Make In Performing A Study There are three possible types of errors that can be produced in a study: 1. Chance or Random Error • Type I (alpha) error • Type II (beta) error 2. Bias 3. Confounding 145
- 146. Chance or Random Error The purpose of statistical testing in science is to Evaluate the role of chance and Estimate the probability that the result observed in a study could have happened purely by chance The two kinds of errors: Rejecting the null or test hypothesis incorrectly Type I error Fail to reject the null hypothesis incorrectly Type II error 146
- 147. Chance or Random Error Consider the hypothesis below: Null Hypothesis: Drug has no effect ↔ no difference in mortality between patients using drug and not using drug Alternate Hypothesis: Drug has effect ↔ reduces mortality 147
- 148. Chance or Random Error 148 Decision on the basis of the sample True state of nature Ho True HA True Reject Ho Type I Error No Error Do not reject Ho No Error Type II Error If we reject Ho and accept HA, we conclude that there is relationship between drug and mortality If we don’t reject Ho, and reject HA, we conclude that there is no relationship between drug and mortality.
- 149. Chance or Random Error Actions to be taken based on decisions: 1. If we reject null hypothesis in favor of the alternative hypothesis we will use the drug Type I error () → Consequence of wrong decision: Type I Error. We will use the drug but the patient don’t benefit. Presuming the drug is not harmful in itself, we do not directly hurt the patients but since we think that we have found the cure, we may no longer test other drugs 2. If we believe the null hypothesis (i.e., fail to reject null hypothesis) we will not use the drug Type II error () →Consequence of wrong decision: Type II Error. Since in reality the drug is beneficial, by withholding it, We will allow patients to die who might otherwise have survived. 149
- 150. Chance or Random Error We cannot eliminate the risk of making one of these types of errors but can lower the probabilities that we will make these errors The probability of making a Type I Error is known as the significance level of a statistical test To lower the probabilities of both the Type I and II Errors in a study It is necessary to increase the number of observations 150
- 151. Chance or Random Error Confidence Interval and P – value Two options to answer whether an observed association in a sample is large enough to be evidence of a true association in the population from which the sample was drawn. The 95% confidence interval P - value A 95% confidence interval It gives a plausible RANGE OF VALUES that should contain the true association in the population. A P-value It is the probability of getting the observed association, or more extreme, in the sample purely by chance from a population where the true association is one. 151
- 152. Bias (Systematic Variation) Bias refers to any systematic error in the design, conduct or analysis of a study that results in a mistaken estimate of an exposures effect on the risk of disease. Systematic variation in a consistent manner in which two study groups are treated or evaluated differently This consistent difference can create an apparent association where one actually does not exist It also masks true association Biases once present cannot be corrected They represent errors in the study design Proper study design is the only protection against biases 152
- 153. Bias (Systematic Variation) Two main types of bias 1. Selection bias Errors in the process of selecting the study population Factors that influence study participation 2. Information bias Occurs during data collection. Errors in the way the information is collected Some Types and Sources of Information Bias Bias in abstracting records Bias in interviewing Bias from surrogate (substitute or proxy) interviews Surveillance bias Recall bias Reporting bias 153
- 154. Bias (Systematic Variation) Selection Bias Occurs when selection of cases or control is related to exposure Selection of patients from hospitals, specialised centres Selection of “healthy” controls from hospitals Response rate bias Self selection bias Survival bias 154
- 155. Bias (Systematic Variation) Information Bias It is a systematic distortion or error that arises from the procedures used for classification or measurement of the disease, the exposure, or other relevant variables. Types of Information Bias 1. Misclassification 2. Observer Bias 3. Recall Bias 155
- 156. Bias (Systematic Variation) Information Bias – Misclassification bias Misclassification bias is a systematic error that can occur at any stage in the research process. It occurs when an individual is assigned to a different category than the one to which they should be assigned. For example, if a patient appears to be non- hypertensive because of medication-controlled blood pressure, resulting in systolic and diastolic measures that are within the ‘normal range’, this may constitute an incorrect classification. 156
- 157. Bias (Systematic Variation) Information Bias – Observer Bias Observer know the underlying hypothesis and ask more probing question to those exposed than controls Remedies for observer bias Blind the observer Use highly structured interview 157
- 158. Bias (Systematic Variation) Information Bias - Recall Bias Disease status affect patients’ response Patient with musculoskeletal diseases are more likely to remember minor trauma Particular problem with case control studies Remedies for recall bias Find reliable records Use control with other illnesses 158
- 159. Confounding Confounding refers to the mixing of the effect of an extraneous variable with the effects of the exposure and disease of interest. It arises when some causes other than the exposure under study is more, or less, prevalent in the exposed group than in the unexposed. Such variable is defined as an extraneous (third) variable which is associated with the exposure and, independent of that exposure, be a risk factor for the disease. 159 A C B Note: A - Exposure B - Outcome variable C - Confounder variable
- 160. 160 Whereas • A mediator is a factor in the causal chain (1), • A confounder is a spurious factor incorrectly implying causation (2)
- 161. Example The RR is determined from an observational study This raises the question whether the exposed and the reference groups are similar in all respects except the exposure under study RR- Relative Risk 161 Confounding
- 162. In addition to the two principal factors, which determine the RR, namely the outcome of the adverse event and the drug exposure status, We must also consider tertiary factors of potentially large importance These factors are related to both the outcome and exposure status – confounding factors Example: See table I and II next slide 162 Confounding
- 163. 163 Table I. Data from a cohort study by Careson et al. (1987) on the effects of NSAIDs on the risk of UGIB Exposed to NSAIDs No. of cases of UGIB Person-months Rate of UGIB/10000 person - months 155 1220000 1.27 Not exposed to NSAIDs No. of cases of UGIB Person-months Rate of UGIB/10000 persons-months Rate ratio 96 1157000 0.83 1.5 UGIB- Upper Gastrointestinal Bleeding Confounding
- 164. 164 Exposed to NSAIDs Alcohol consumption Heavy Light Exposed to NSAIDs No. of cases of UGIB Person-months Rate of UGIB/10000 person- month 143 12 492000 728000 2.91 0.16 Not exposed to NSAIDs No. of cases of UGIB Person-months Rate of UGIB/10000 person- months Rate ratio 95 1 982,000 175000 0.97 0.06 3.0 2.9 Table 2. Hypothesis stratification to illustrate confounding by alcohol consumption of data by Careson et al. (1987) on the effects of NSAIDs on the risk of UGIB Confounding
- 165. Characteristics of a Confounding Variable 1. Associated with the disease of interest in the absence of exposure. Risk factor for the study outcome among exposed group Risk factor for the study outcome among non exposed 2. Associated with the study exposure but not as a consequence of the exposure. 165 Confounding
- 166. Effect of Confounding 1. Totally or partially accounts for the apparent effect 2. Mask an underlying true association 3. Reverse the actual direction of the association 166 Confounding
- 167. Remedies to Confounding 1. In the DESIGN confounding could minimize by: Match (match case and control for gender and age) Restriction (limit study to certain groups) Randomisation (limit to treatment) 2. In the ANALYSIS Stratification Standardisation Statistical modelling (multivariate analysis) 167 Confounding
- 168. Probability of random error can be quantified using statistics. Bias needs to be prevented by designing the study properly and Confounding can be controlled in either the design of the study or in its analysis. If the three types of errors excluded, then one is left with a True Causal Association 168 Summary
- 169. 2.5.3. Criteria for the Causal Nature of an Association The “Criteria for the causal nature of an association” were first put forth by Sir Austin Bradford Hill But have been described in various forms since, Each with some modification. Probably the best known description of them was in the first Surgeon General’s Report on Smoking and Health, published in 1964. 169 https://profiles.nlm.nih.gov/NN/B/B/M/Q/_/nnb bmq.pdf
- 170. Criteria for the Causal Nature of an Association 1. Coherence with existing information (also called biological plausibility) 2. Consistency of the association 3. Time sequence 4. Specificity of the association 5. Strength of the association a. Quantitative strength b. Dose–response relationship c. Study design 170
- 171. 1. Coherence with existing information or biological plausibility Refers to whether the association makes sense, in light of other types of information available in the literature. These other types of information could include: Data from other human studies, Data from studies of other related questions, Data from animal studies, or Data from in vitro studies, as well as Scientific or pathophysiologic theory. Example: The association between cigarettes and lung cancer cigarette smoke is a known carcinogen based on animal data Cause cancers of the head and neck, the pancreas, and the bladder in human 171
- 172. 2. The Consistency of the Association Reproducibility of the association in different settings which includes Different geographic settings, Different study designs, Different populations For example, in the case of cigarettes and lung cancer, the association has now been reproduced In many different studies, In different geographic locations, Using different study designs. 172
- 173. 3. Time Sequence A cause must precede an effect. Although this may seem obvious, there are study designs from which this cannot be determined. Example: Cigarette smoking usually precedes the lung cancer 173
- 174. 4. Specificity Refers effect and whether the effect ever occurs without the presumed cause. This criterion is almost never met in biology, with the occasional exception of infectious diseases. It provides extremely strong support for a conclusion that an association is causal if the criteria met 174
- 175. 5. Strength of the Association 5a. Quantitative Strength of an Association Refers to the effect size. To evaluate this, One asks whether the magnitude of the observed difference between the two study groups is large. A quantitatively large association can only be created by a causal association or a large error, which should be apparent in evaluating the methodology of a study. A quantitatively small association may still be causal, but it could be created by a subtle error, which would not be apparent in evaluating the study. 175
- 176. 5b. Dose – Response Relationship Exists when an increase in the intensity of an exposure results in an increased risk of the disease under study. Equivalent to this is a duration–response relationship which exists when a longer exposure causes an increased risk of the disease. The presence of either a dose–response relationship or a duration–response relationship strongly implies that an association is, in fact, a causal association. 176
- 177. 5c. Study Design Used It refers whether the study was well designed, whether the study was subject to one of the three errors namely Random error, Bias, and Confounding. And which study design was used in the studies in question. 177
- 178. 2.6. Sample Size Consideration for Pharmacoepidemiology Studies 2.6.1. Background 2.6.2. Sample Size Determination 2.6.2.1. Factors That Affect Sample Size Calculations 2.6.2.2. Sample Size Calculations For Cohort Studies 2.6.2.3. Sample Size Calculations For Case-Control Studies 2.6.2.4. Sample Size Calculations For Case Series 2.6.2. Sampling Techniques 178
- 179. 2.6.1. Background In premarketing study Uses sample size between 500 and 3000 To be 95% certain to detect ADR between 1 and 6 in 1000 exposed respectively In post marketing studies Needs large sample size than premarketing To increase significance Requirement for large sample sizes raises Logistical obstacles to cost-effective studies Thus, Needs to know how to calculates the minimum sample size necessary for a pharmacoepidemiology study To avoid the problem of a study with a sample size that is too small 179
- 180. 2.6.1. Background Research studies are conducted with many different aims in mind. A study may be conducted to establish The difference, or conversely the similarity Between two groups defined in terms of a particular Risk factor or Treatment regimen. Alternatively, it may be conducted to estimate some quantity For example, the prevalence of disease In a specified population With a given degree of precision. Regardless of the motivation for the study It is essential that to have an appropriate size to achieve its aims. The most common aim is probably That of determining some difference between two groups 180
- 181. 2.6.1. Background The difference between two groups in a study will usually be explored in terms of An estimate of effect It is the size of the effect to be detected Appropriate P value or confidence interval The confidence interval indicates The likely range of values for the true effect in the population The P value determines How likely it is that the observed effect in the sample is due to chance. The statistical power of the study It is the probability of correctly identifying a difference between the two groups in the study sample When one genuinely exists in the populations from which the samples were drawn. 181
- 182. 2.6.2. Sample Size Determination 2.6.2.1. Factors That Affect Sample Size Calculations 2.6.2.2. Sample Size Calculations For Cohort Studies 2.6.2.3. Sample Size Calculations For Case-Control Studies 2.6.2.4. Sample Size Calculations For Case Series 182
- 183. 2.6.2.1. Factors that Affect Sample Size Calculations There are three main factors that must be considered in the appropriate sample size calculation. 183 Once these three factors have been established, there are tabulated values and formulae available for calculating the required sample size for different study designs.
- 184. 2.6.2.2. Sample Size Calculations for Cohort Studies The sample size required for a cohort study depends on what you are expecting from the study. To calculate sample sizes for a cohort study, one needs to specify five variables 1. Type I error () considered tolerable, and Whether it is one-tailed or two-tailed 2. Type II error () considered tolerable 3. Minimum relative risk (RR) to be detected 4. Incidence of the disease in the unexposed control group 5. Ratio of unexposed controls to exposed study subjects 184
- 185. Type I error That one is willing to tolerate in the study Probability of concluding there is a difference between the groups being compared when in fact a difference does not exist. Using diagnostic tests as an analogy A type I error is a false positive study finding 185
- 186. Type II error That one is willing to tolerate in the study. A type II error is the probability of concluding There is no difference between the groups being compared When in fact a difference does exist. A type II error is the probability of missing a real difference Using diagnostic tests as an analogy, A type II error is a false negative study finding. The complement of is the power of a study The probability of detecting a difference if a difference really exists. Power is calculated as (1− ). 186
- 187. The minimum effect size one wants to be able to detect. For a cohort study, this is expressed as a relative risk. The expected incidence of the outcome of interest in the unexposed control group. The number of unexposed control subjects to be included in the study for each exposed study subject. A study has the most statistical power for a given number of study subjects If it has the same number of controls as exposed subjects. However, sometimes the number of exposed subjects is limited and, therefore, inadequate to provide sufficient power to detect a relative risk of interest. In that case, additional power can be gained by increasing the number of controls alone. Doubling the number of controls, that is including two controls for each exposed subject, results in a modest increase in the statistical power, but it does not double it. Including three controls for each exposed subject increases the power further. 187
- 188. Example: Sample Size Formula For Cohort Study where p is the incidence of the disease in the unexposed, R is the minimum relative risk to be detected, is the type I error rate which is acceptable, is the type II error rate which is acceptable, Z 1 − and Z 1− refer to the unit normal deviates corresponding to and , K is the ratio of number of control subjects to the number of exposed subjects, and Z 1 − is replaced by Z 1 − /2 if one is planning to analyze the study using a two-tailed 188
- 189. 2.6.2.3. Sample Size Calculations for Case-Control Studies The approach to calculating sample sizes for case– control studies is similar to the approach for cohort studies. There are five variables that need to be specified 1. Type I error () considered tolerable, and whether it is one-tailed or two-tailed 2. Type II error () considered tolerable 3. Minimum odds ratio to be detected 4. Prevalence of the exposure in the un-diseased control group 5. Ratio of un-diseased controls to diseased study subjects 189
- 190. In a case–control study one selects subjects based on the presence or absence of the disease of interest, And then investigates the prevalence of the exposure of interest in each study group. This is in contrast to a cohort study, In which one selects subjects based on the presence or absence of an exposure, And then studies whether or not the disease of interest develops in each group. Therefore, the fourth variable to be specified for a case–control study is The expected prevalence of the exposure in the un-diseased control group, Rather than the incidence of the disease of interest in the unexposed control group of a cohort study. 190
- 191. Example: Sample Size Formula For Case– control Study 191
- 192. NB. Sample size determinations in cohort and Case–control studies Assume one is able to obtain information on each of the five variables that factor into these sample size calculations. But it is unrealistic Four of the variables are totally in the control of the investigator, subject to his or her specification: α, β, the ratio of control subjects to study subjects, and the minimum relative risk to be detected. Only one of the variables requires data derived from other sources. For Cohort Studies, This is the expected incidence of the disease in the unexposed control group. For Case–Control Studies, This is the expected prevalence of the exposure in the un-diseased control group. 192
- 193. 2.6.2.4. Sample size calculations for Case series Case series are usually used in pharmacoepidemiology to quantitate better incidence of a particular disease in patients exposed to a newly marketed drug. Example 1: In the “Phase IV” post marketing drug surveillance study conducted for prazosin, the investigators collected a case series of 10 000 newly exposed subjects recruited through the manufacturer’s sales force, to quantitate better the incidence of first-dose syncope, which was a well-recognized adverse effect of this drug. 193
- 194. Case series are usually used to determine Whether a disease occurs more frequently than some predetermined incidence in exposed patients. Most often, the predetermined incidence of interest is zero. And one is looking for any occurrences of an extremely rare illness. 194
- 195. Example 2: When CIMETIDINE was first marketed, there was a concern over whether it could cause agranulocytosis, since it was closely related chemically to METIAMIDE, another H-2 blocker, which had been removed from the market in Europe because it caused agranulocytosis. This study collected 10 000 subjects. It found only two cases of neutropenia, one in a patient also receiving chemotherapy. There were no cases of agranulocytosis. 195
- 196. Poisson Distribution Method To establish drug safety, a study must include a sufficient number of subjects to detect an elevated incidence of a disease, if it exists. Generally, this is calculated by assuming the frequency of the event in question is vanishingly small, so that the occurrence of the event follows a Poisson distribution, and then one generally calculates 95% confidence intervals around the observed results. 196 μ - The mean number of successes (occurrence of an event) that occur in a specified period of time, μ = λ x t X = The actual number of successes that occur in a specified period of time.
- 197. In order to apply Poisson Distribution, one first calculates the incidence rate observed from the study’s results 𝑰𝑹 𝒐𝒃𝒔𝒆𝒓𝒗𝒆𝒅 = 𝒏𝒐. 𝒐𝒇 𝒔𝒖𝒃𝒆𝒋𝒄𝒕𝒔 𝒅𝒆𝒗𝒆𝒍𝒐𝒑 𝒅𝒊𝒔𝒆𝒂𝒔𝒆 𝒅𝒖𝒓𝒊𝒏𝒈 𝒔𝒑𝒆𝒄𝒊𝒇𝒊𝒆𝒅 𝒕𝒊𝒎𝒆 𝒊𝒏𝒕𝒆𝒓𝒗𝒂𝒍 𝒕𝒉𝒆 𝒕𝒐𝒕𝒂𝒍 𝒏𝒐. 𝒐𝒇 𝒊𝒏𝒅𝒊𝒗𝒊𝒅𝒖𝒂𝒍𝒔 𝒊𝒏 𝒕𝒉𝒆 𝒑𝒐𝒑𝒖𝒍𝒂𝒕𝒊𝒐𝒏 𝒂𝒕 𝒓𝒊𝒔𝒌 For example, If three cases of liver disease were observed in a population of 1000 patients exposed to a new nonsteroidal anti-inflammatory drug during a specified period of time, the incidence would be 0.003. The number of subjects who develop the disease is the “Observed number on which estimate is based (n)” in Table A17. In this example, it is 3. 197
- 198. The lower boundary of the 95% confidence interval for the incidence rate is then the corresponding “Lower limit factor (L)” multiplied by the observed incidence rate. In the example above, it would be 0.206 ×0.003 =0.000 618. Analogously, the upper boundary would be the product of the corresponding “Upper limit factor (U)” multiplied by the observed incidence rate. In the above example, this would be 2.92 × 0.003 =0.00876. In other words, the incidence rate (95% confidence interval) would be 0.003 (0.000618 − 0.00876). Thus, the best estimate of the incidence rate would be 30 per 10 000, but there is a 95% chance that it lies between 6.18 per 10 000 and 87.6 per 10 000. 198
- 199. 199
- 200. “Rule of threes” Method Simple guide which is useful in the common situation where no events of a particular kind are observed. Specifically, if no events of a particular type are observed in a study of X individuals, Then one can be 95% certain that the event occurs no more often than 3/X. N = 3/x 200
- 201. “Rule of threes” Method Example, If 500 patients are studied prior to marketing a drug, then one can be 95% certain that any event which does not occur in any of those patients may occur with a frequency of 3 or less in 500 exposed subjects, or that it has an incidence rate of less than 0.006. If 3000 subjects are exposed prior to drug marketing, then one can be 95% certain that any event which does not occur in this population may occur no more than 3 in 3000 subjects, or the events have an incidence rate of less than 0.001. If 10 000 subjects are studied in a post-marketing drug surveillance study, then one can be 95% certain that any events which are not observed may occur no more than 3 in 10 000 exposed individuals, or that they have an incidence rate of less than 0.0003. In other words, events not detected in the study may occur less often than 1 in 3333 subjects. 201