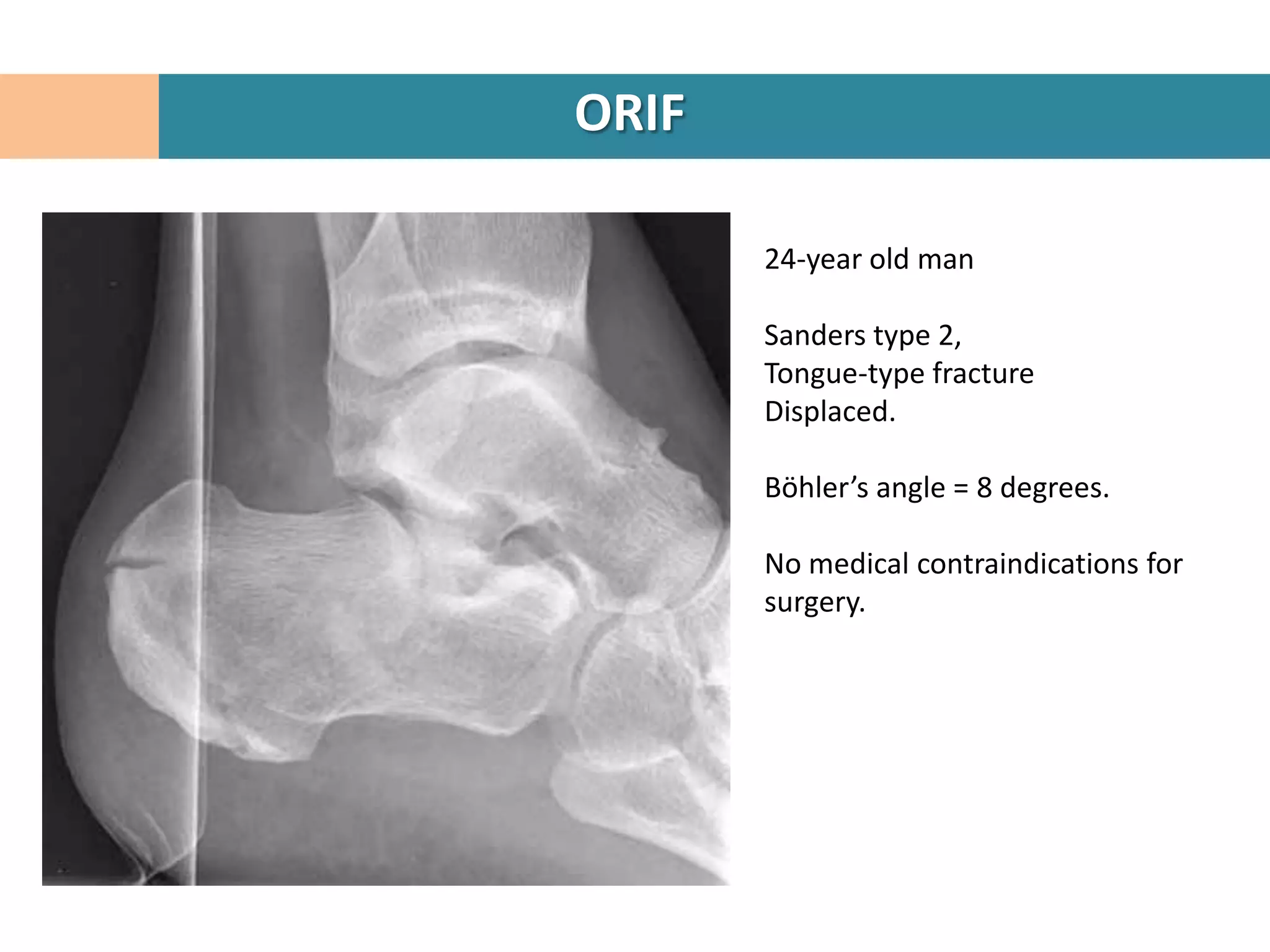
Here are the key steps in the ORIF procedure:
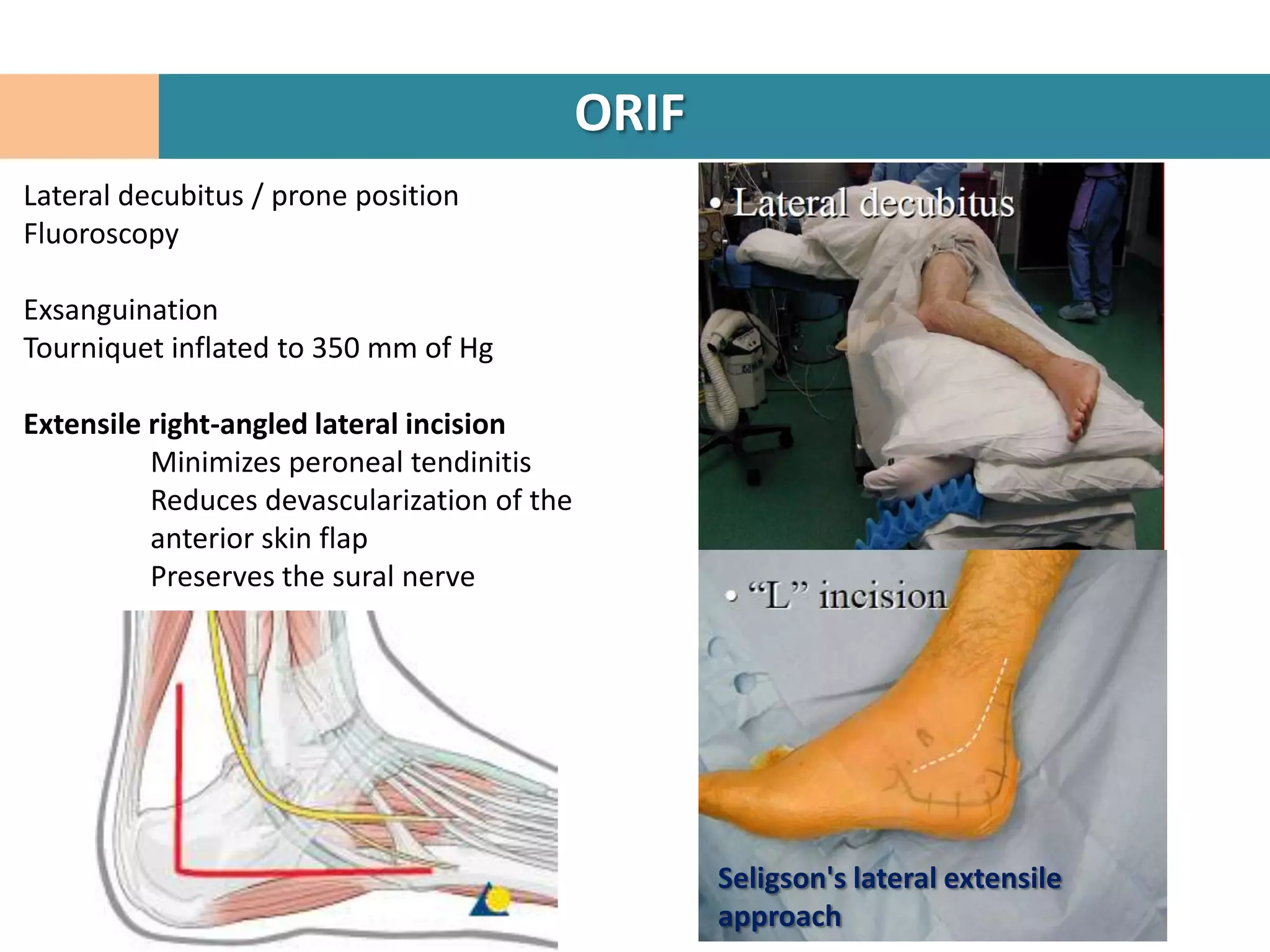
1. Patient is placed in lateral decubitus position and a right-angled lateral incision is made to minimize soft tissue damage.
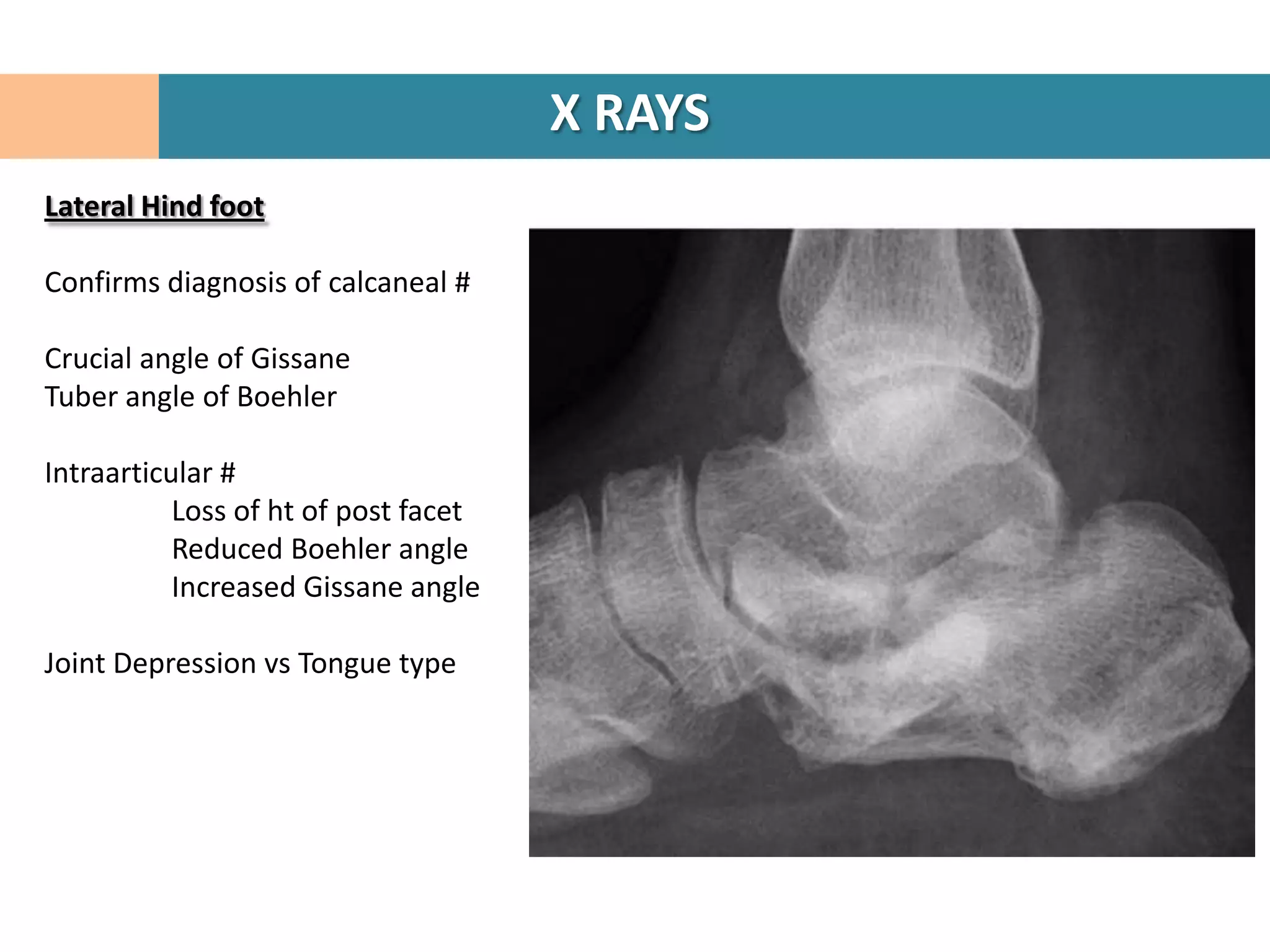
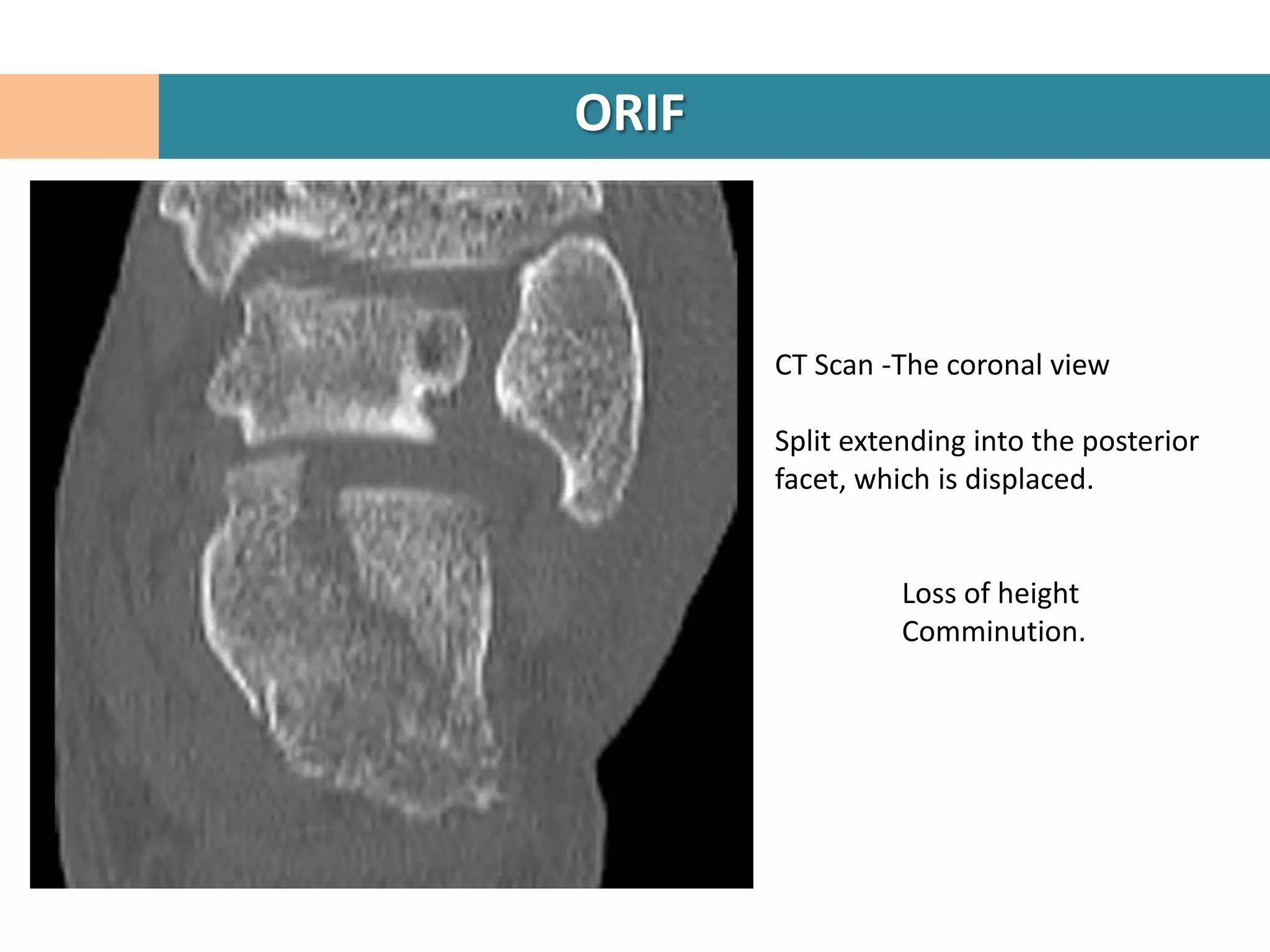
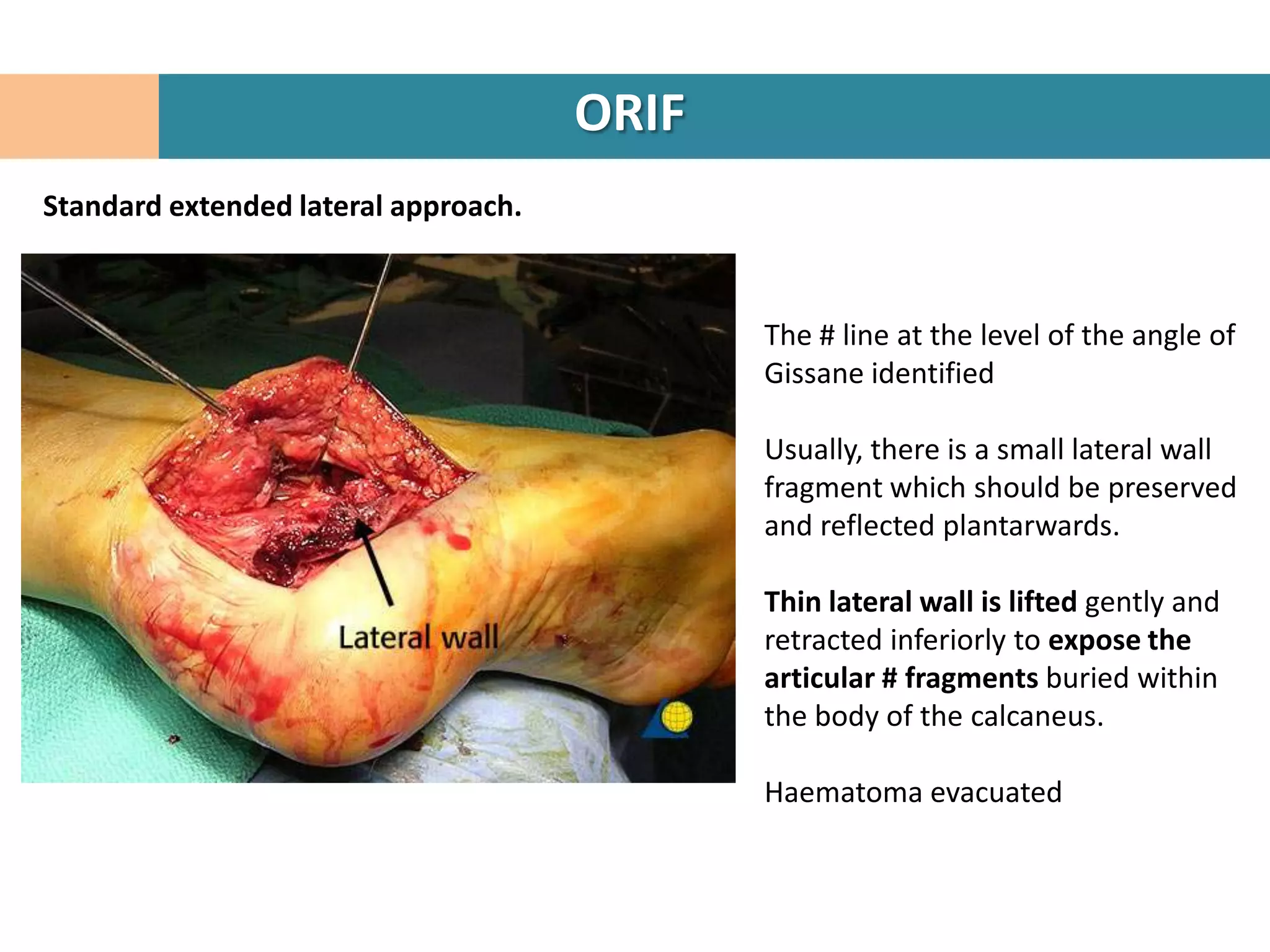
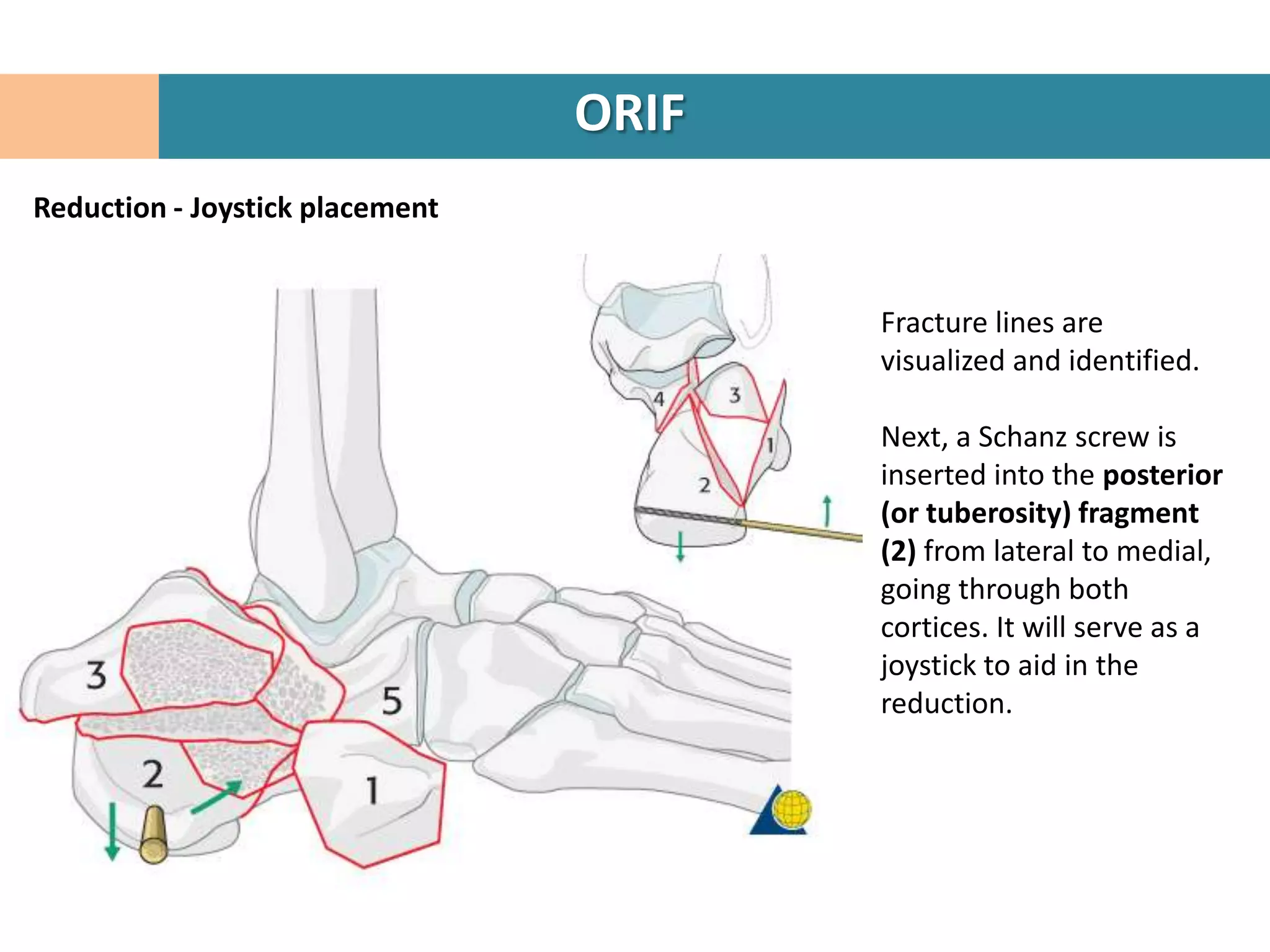
2. The fracture line at the angle of Gissane is identified.
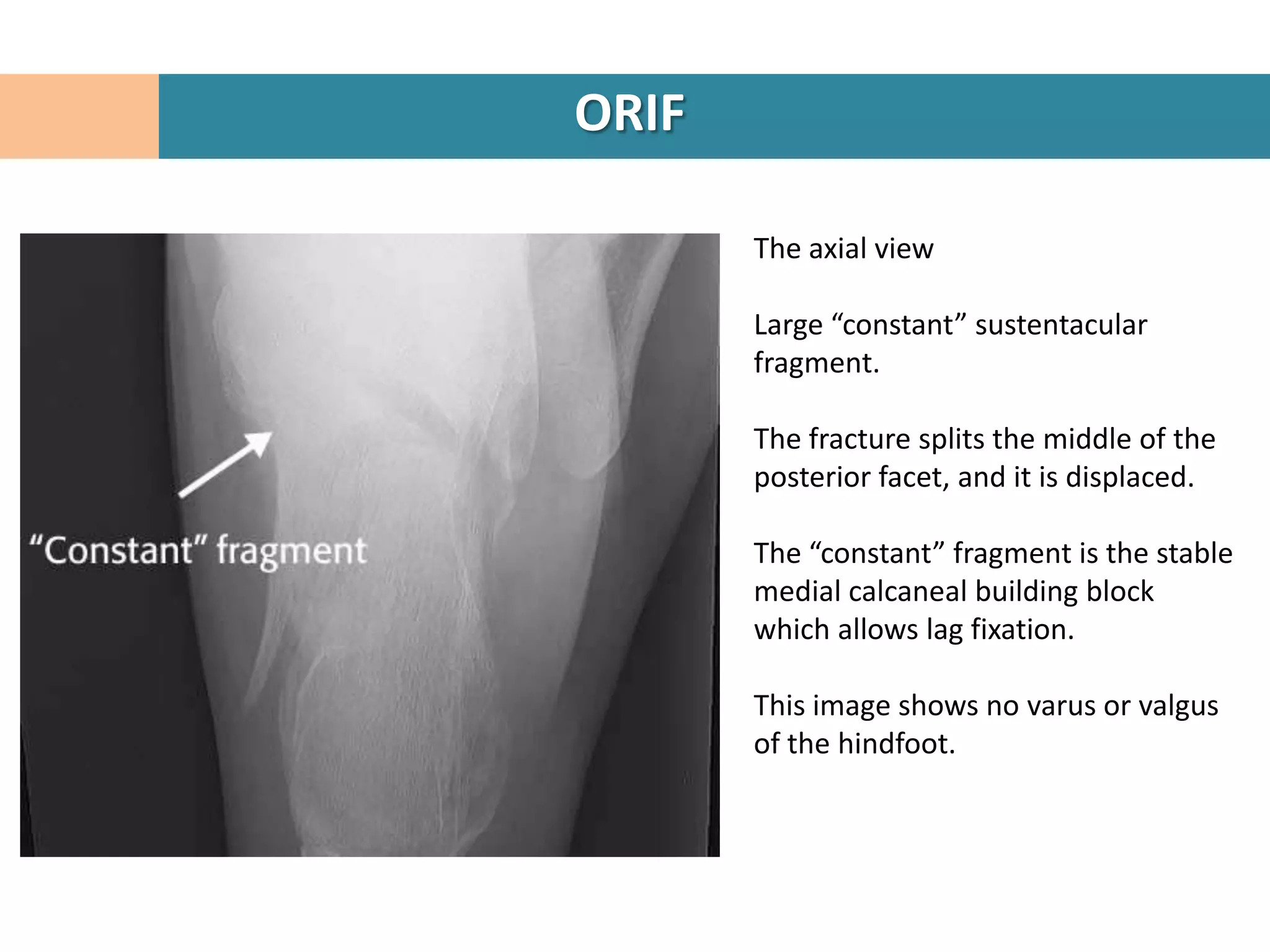
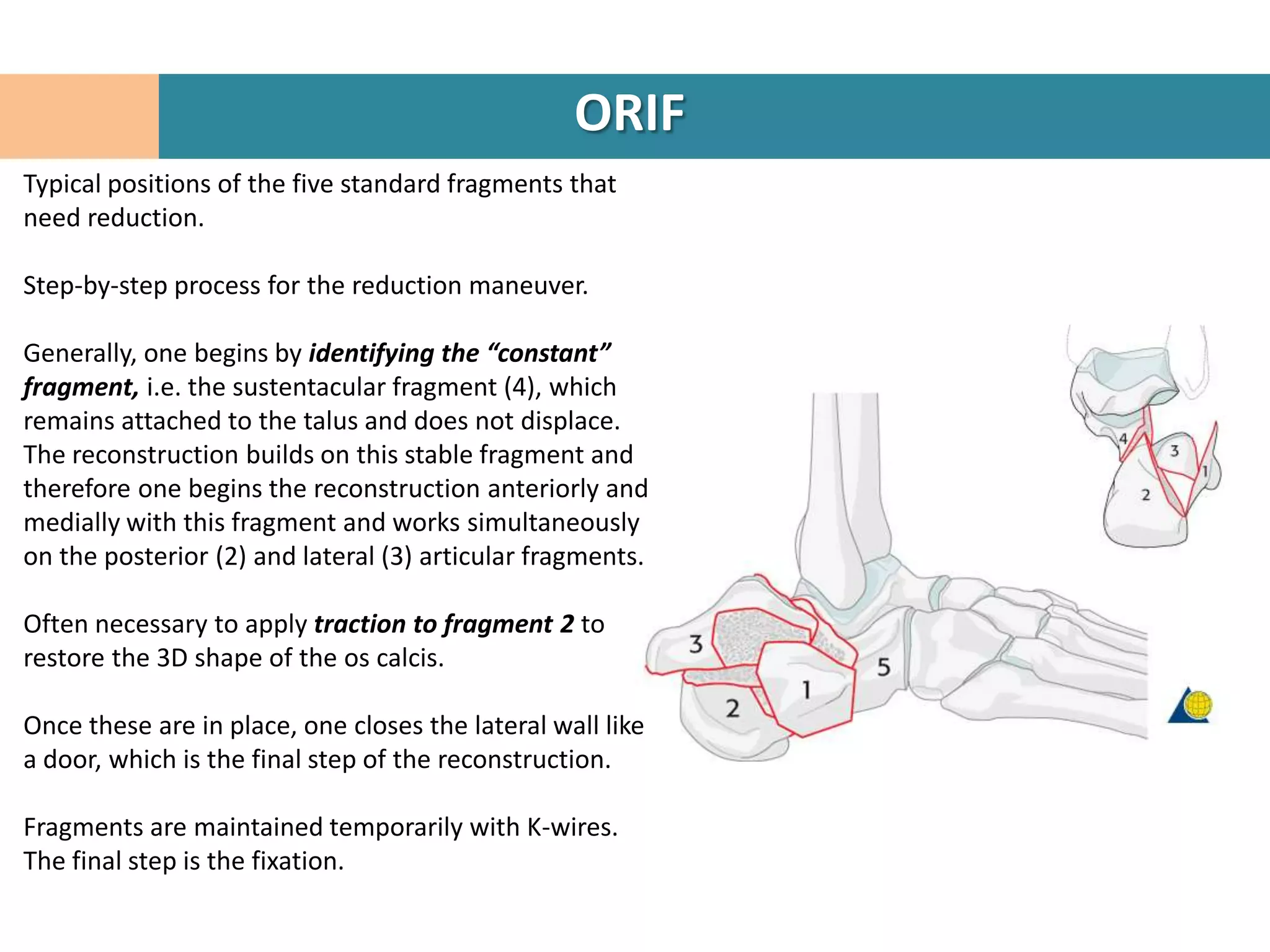
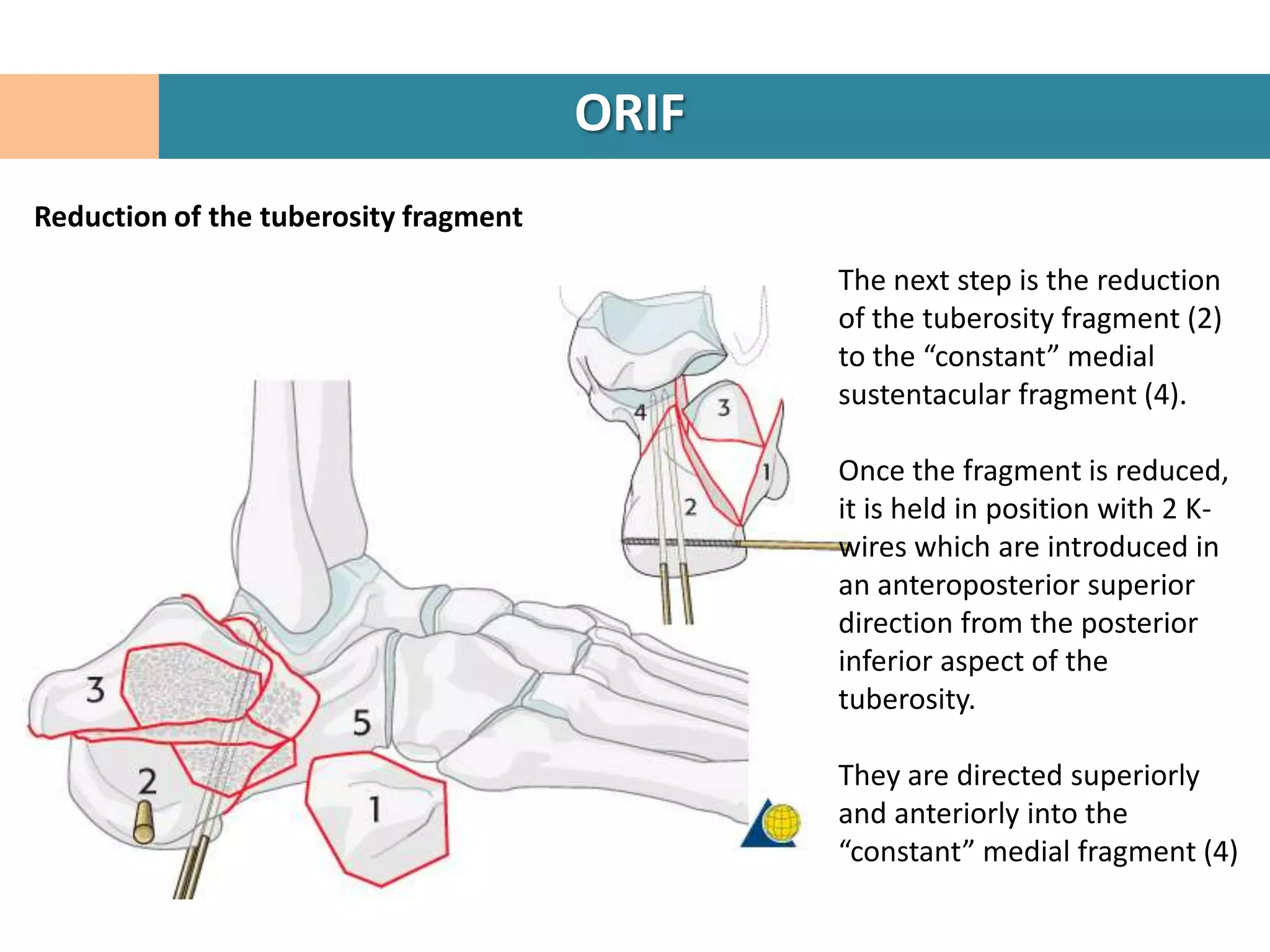
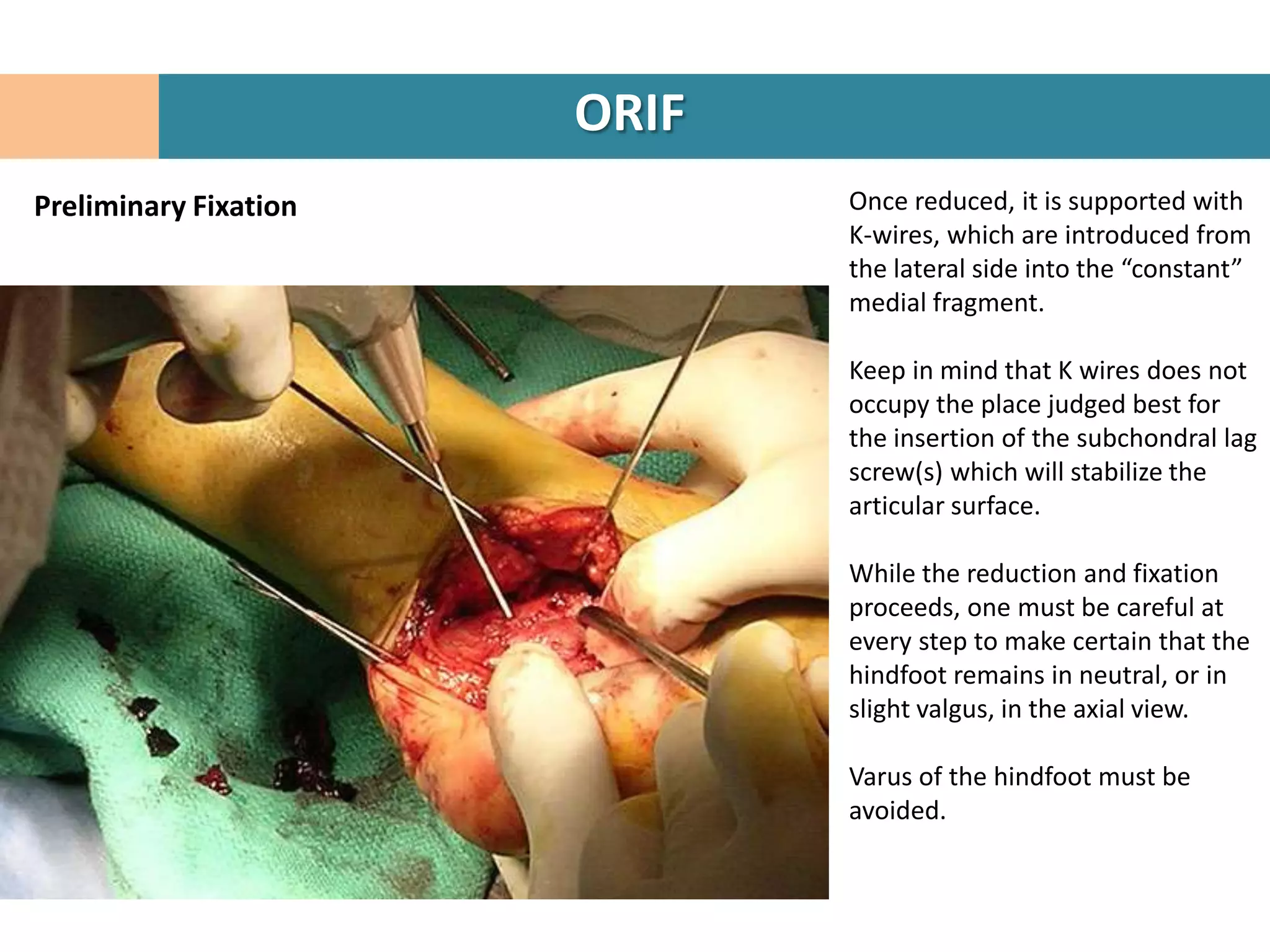
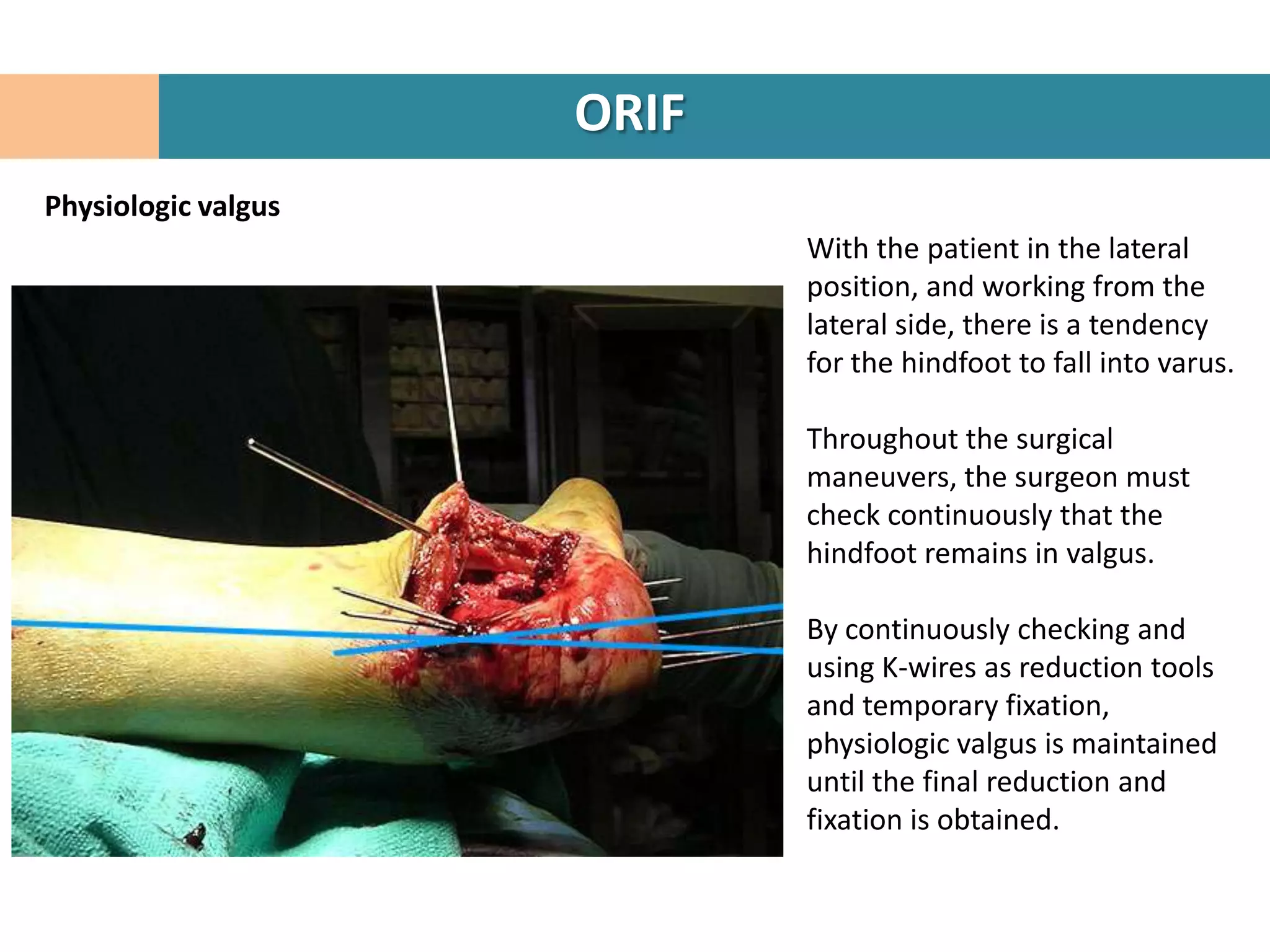
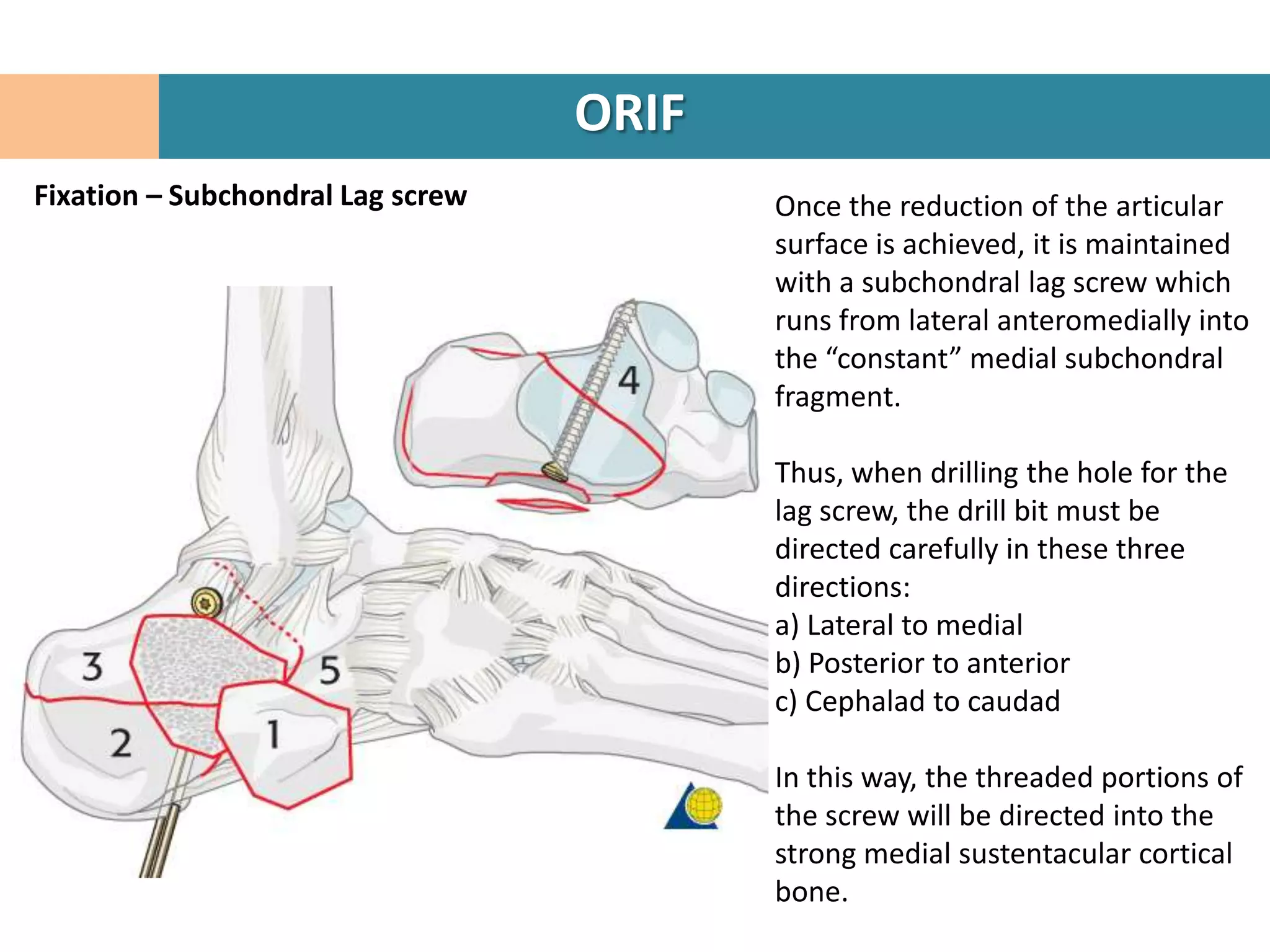
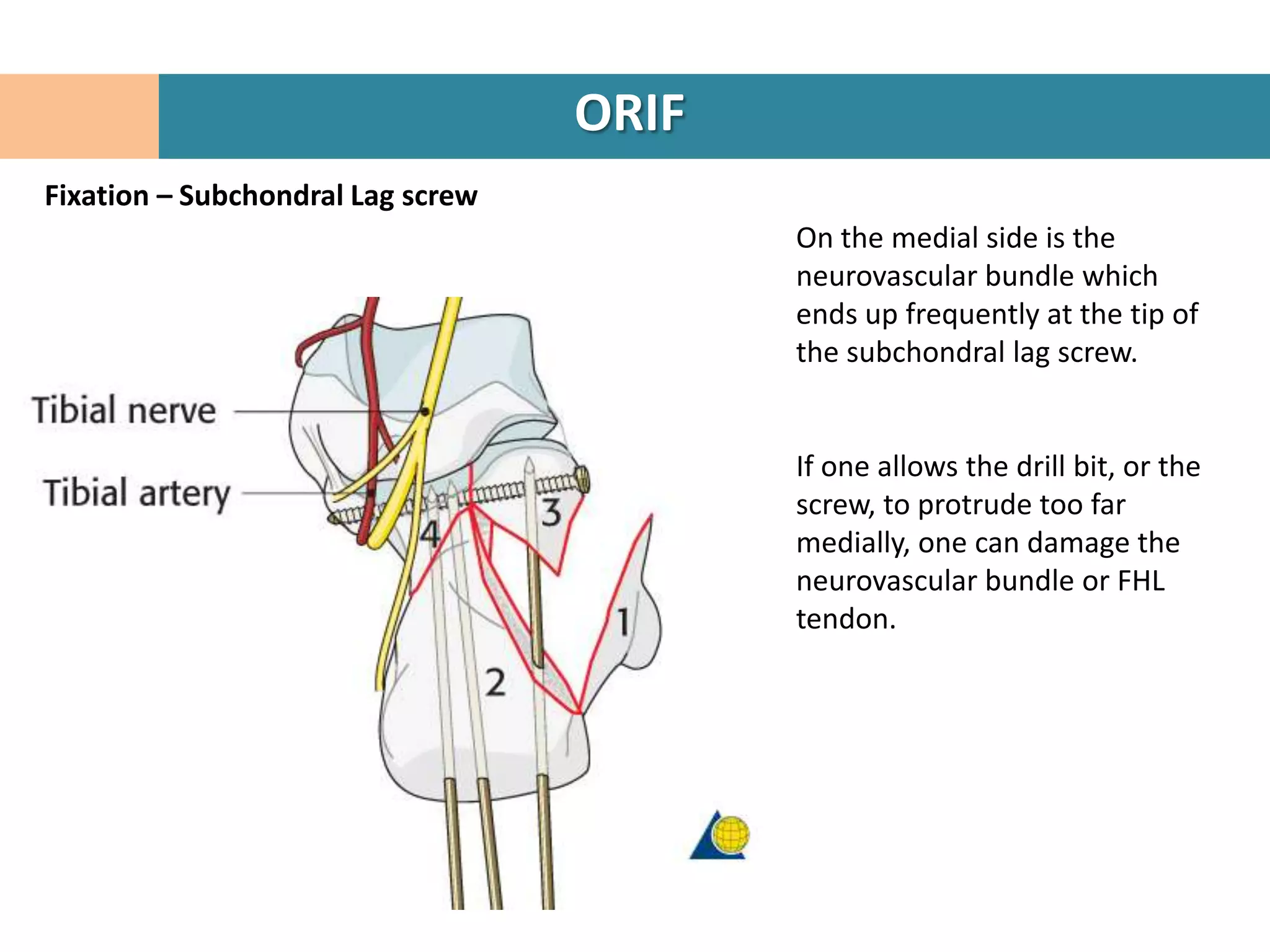
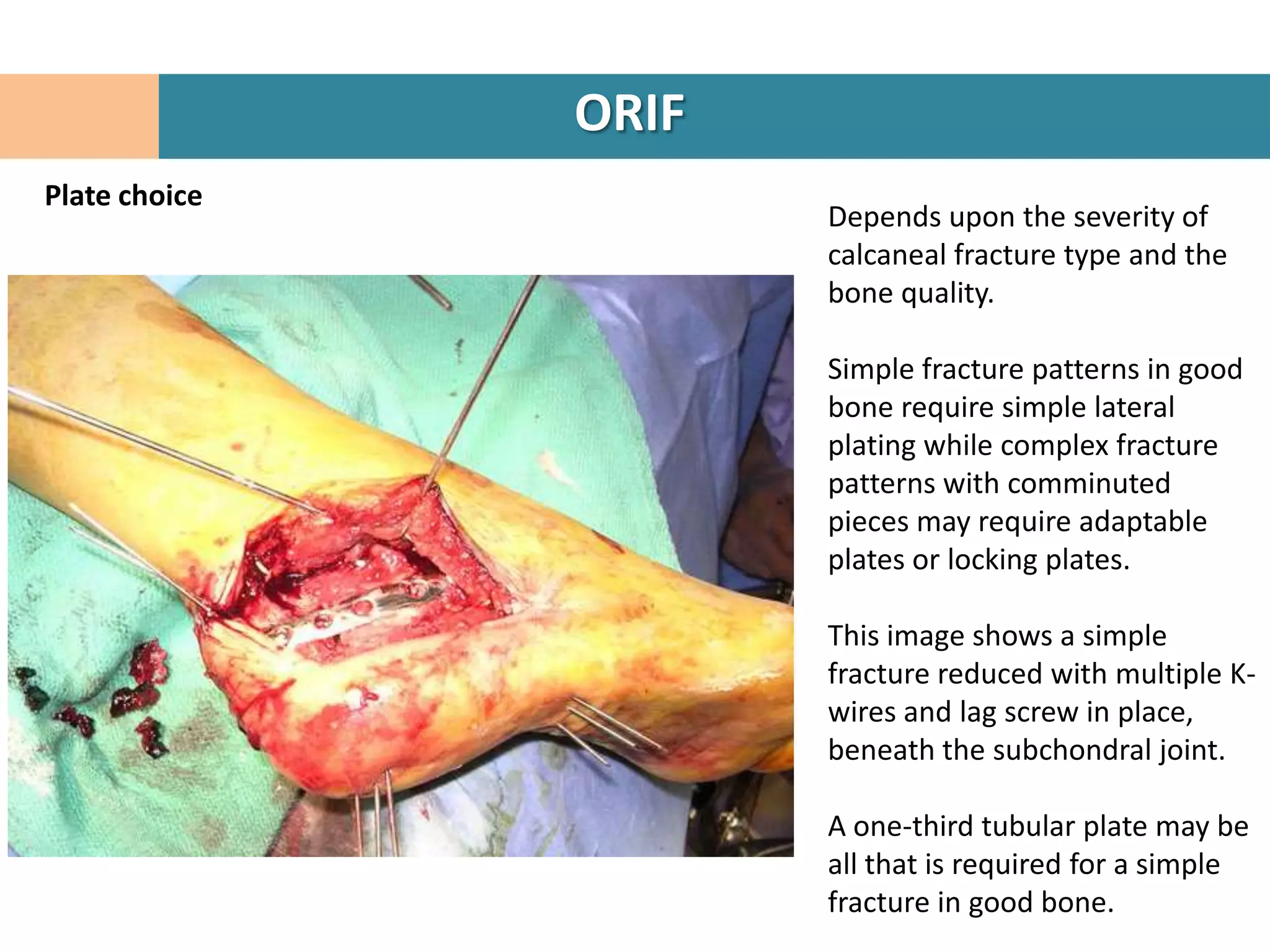
3. Fragments are temporarily held in place with K-wires under fluoroscopy while the reconstruction restores the 3D shape of the calcaneus.
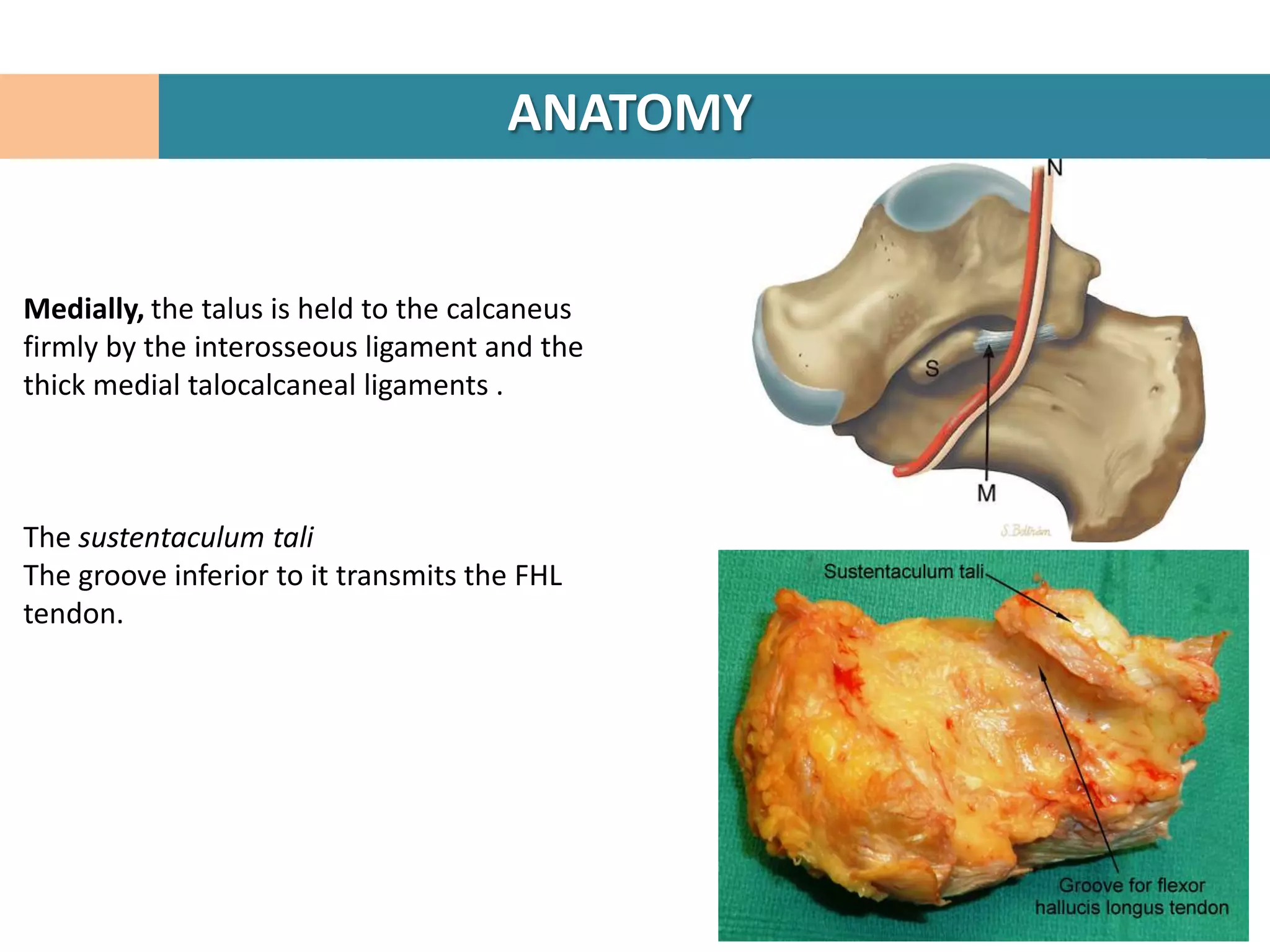
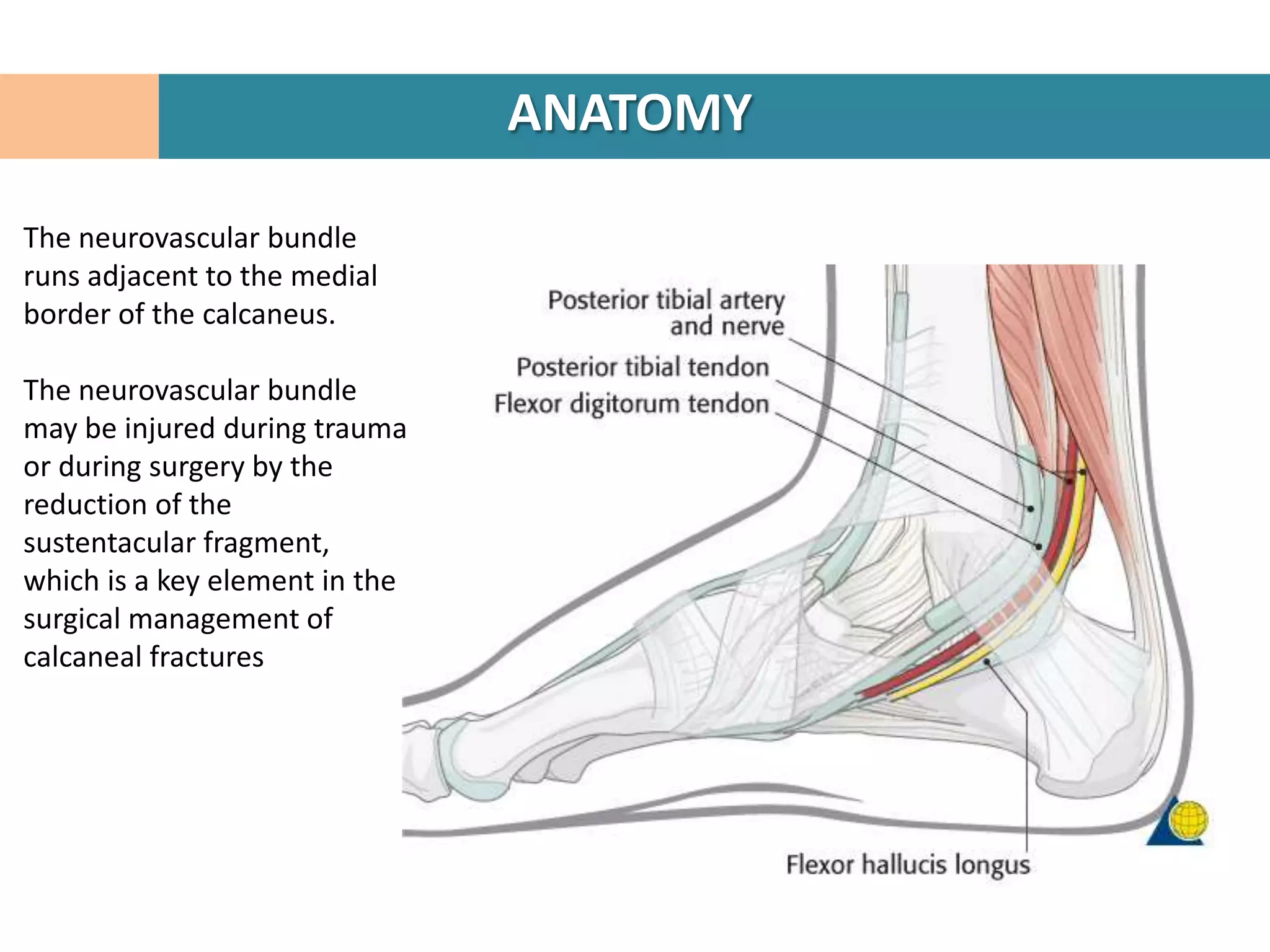
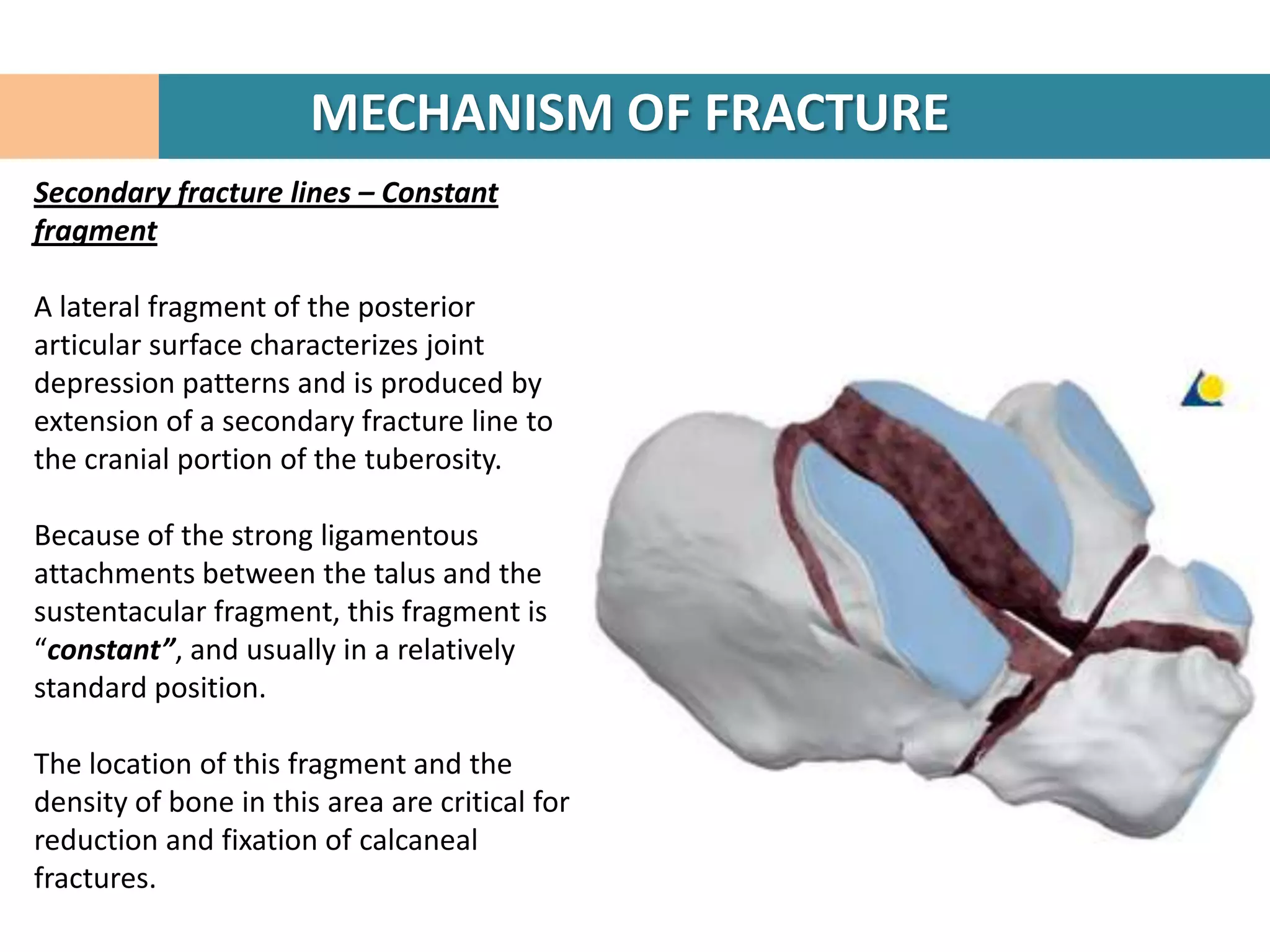
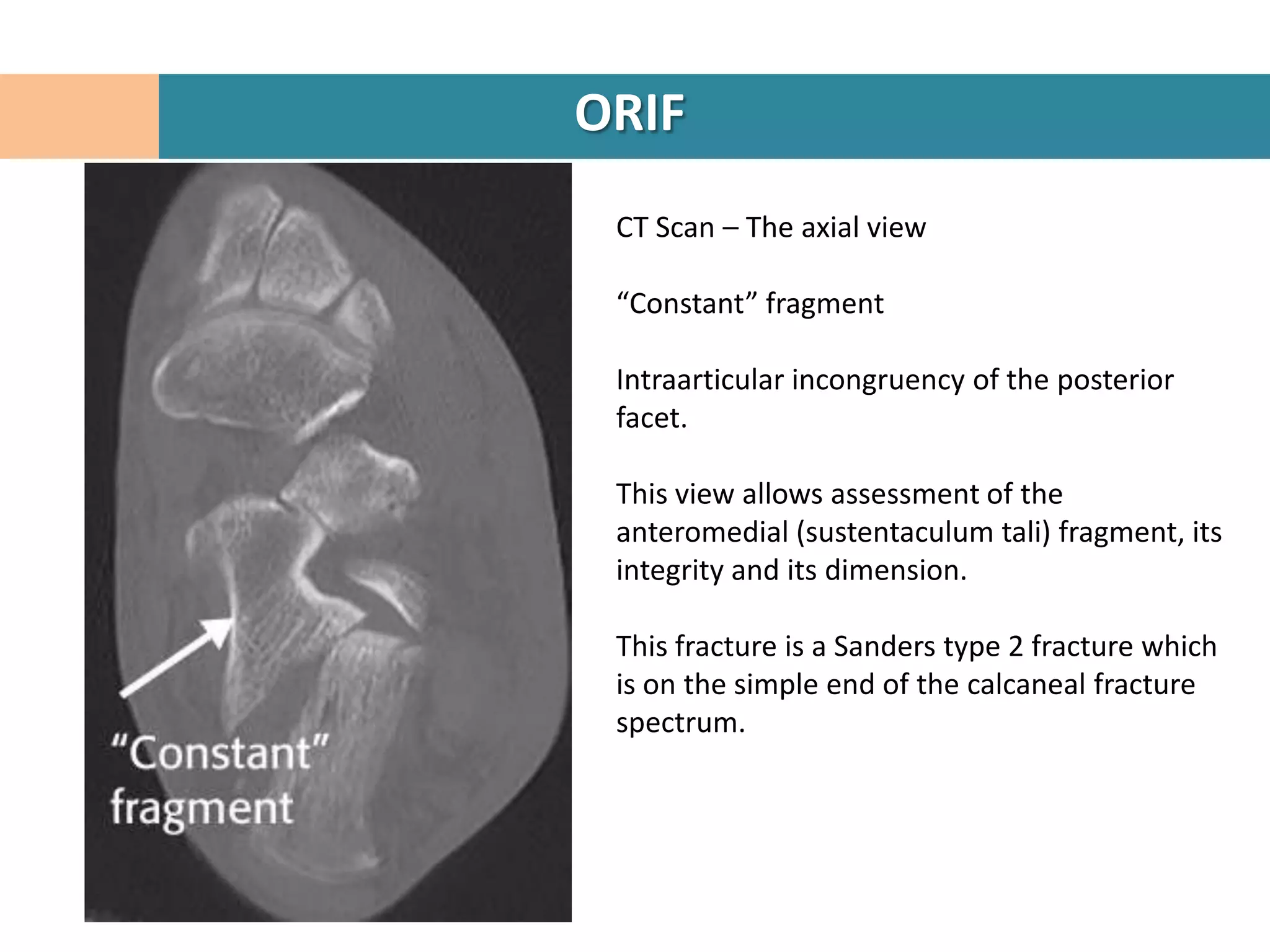
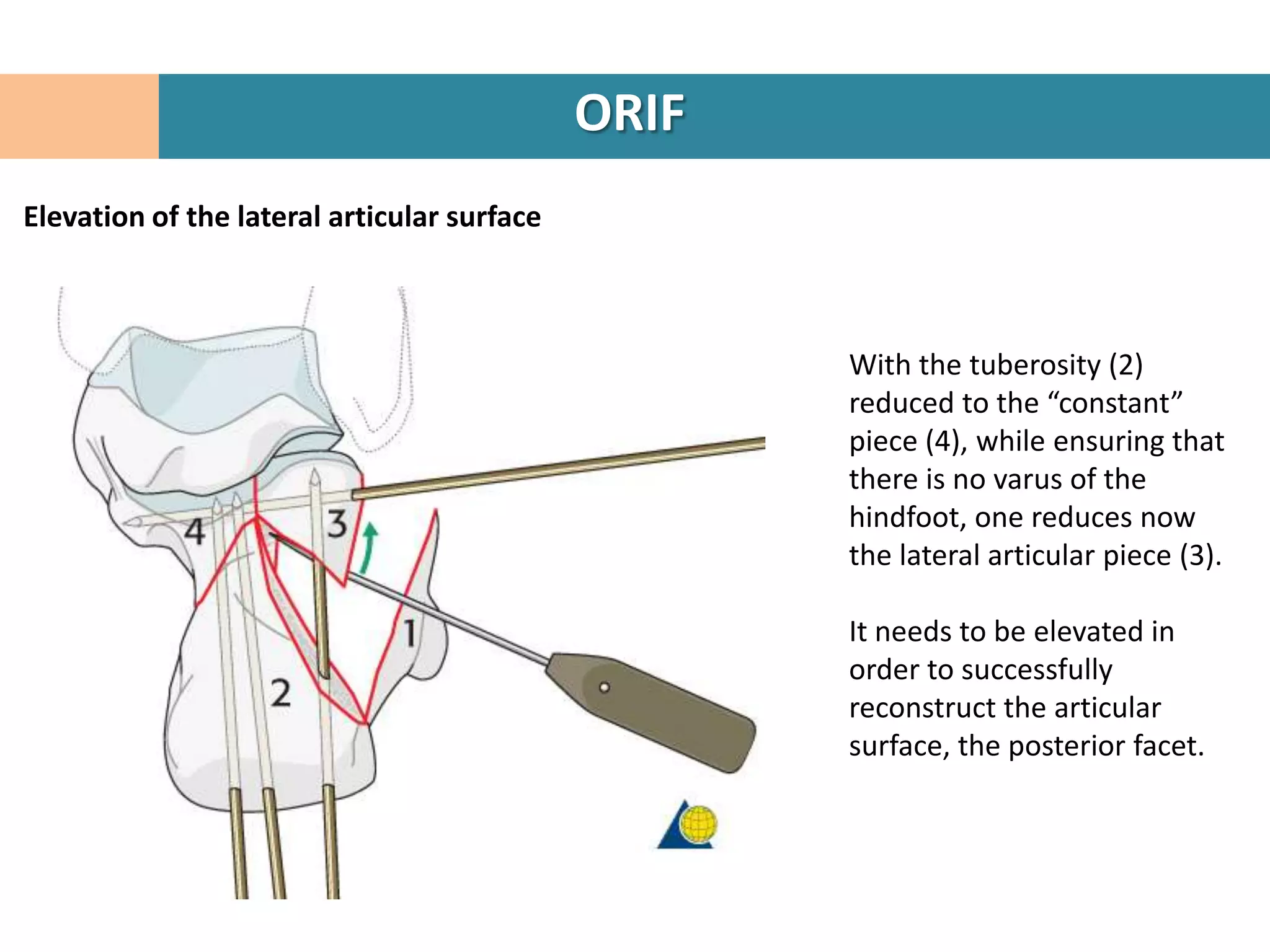
4. The "constant" sustentacular fragment is used to begin the reconstruction, working anteriorly and medially.
5. Traction may be needed to restore the posterior facet.
6. The lateral wall fragment is closed like a door last to complete the