Embed presentation
Download as PDF, PPTX
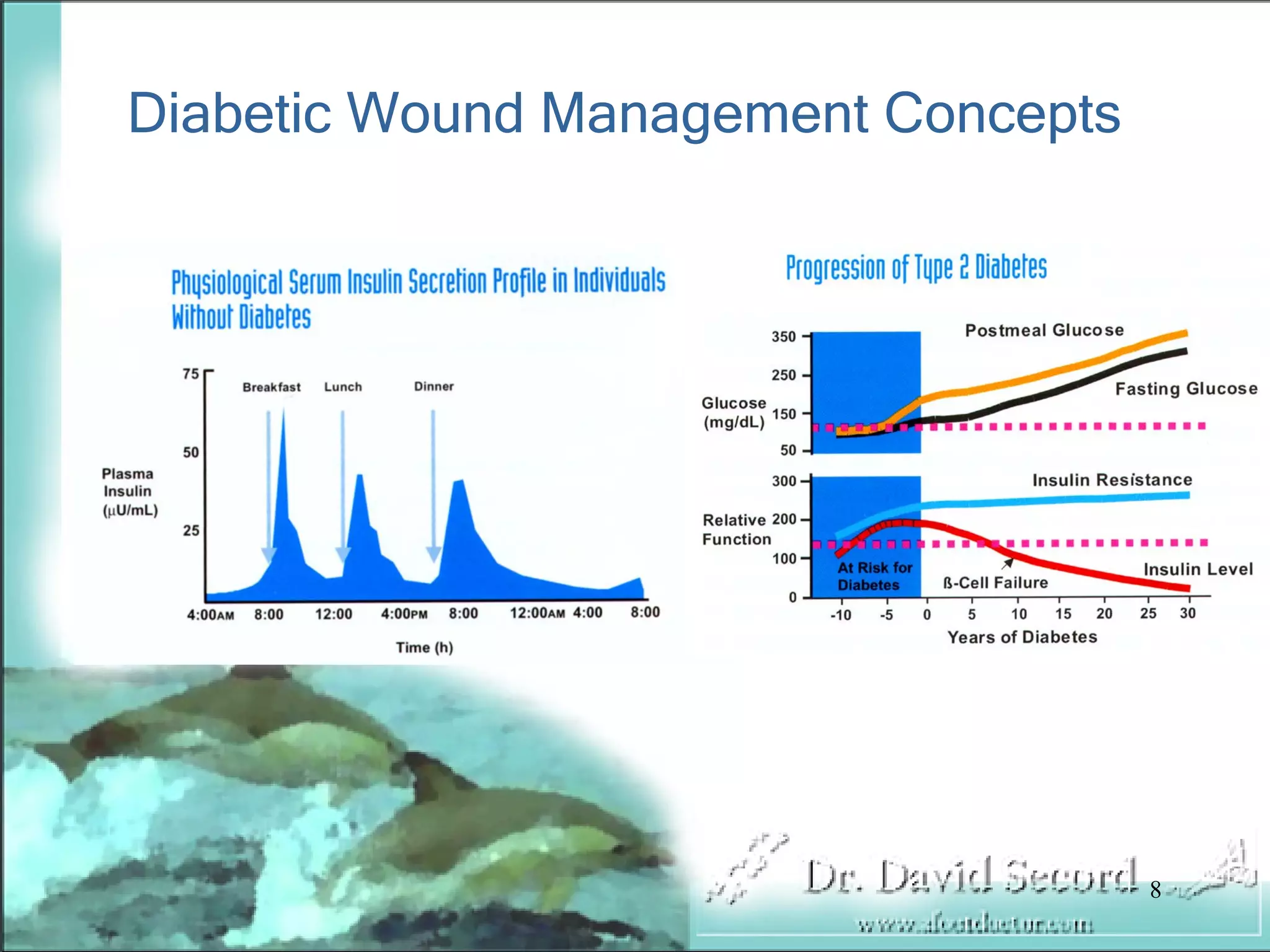

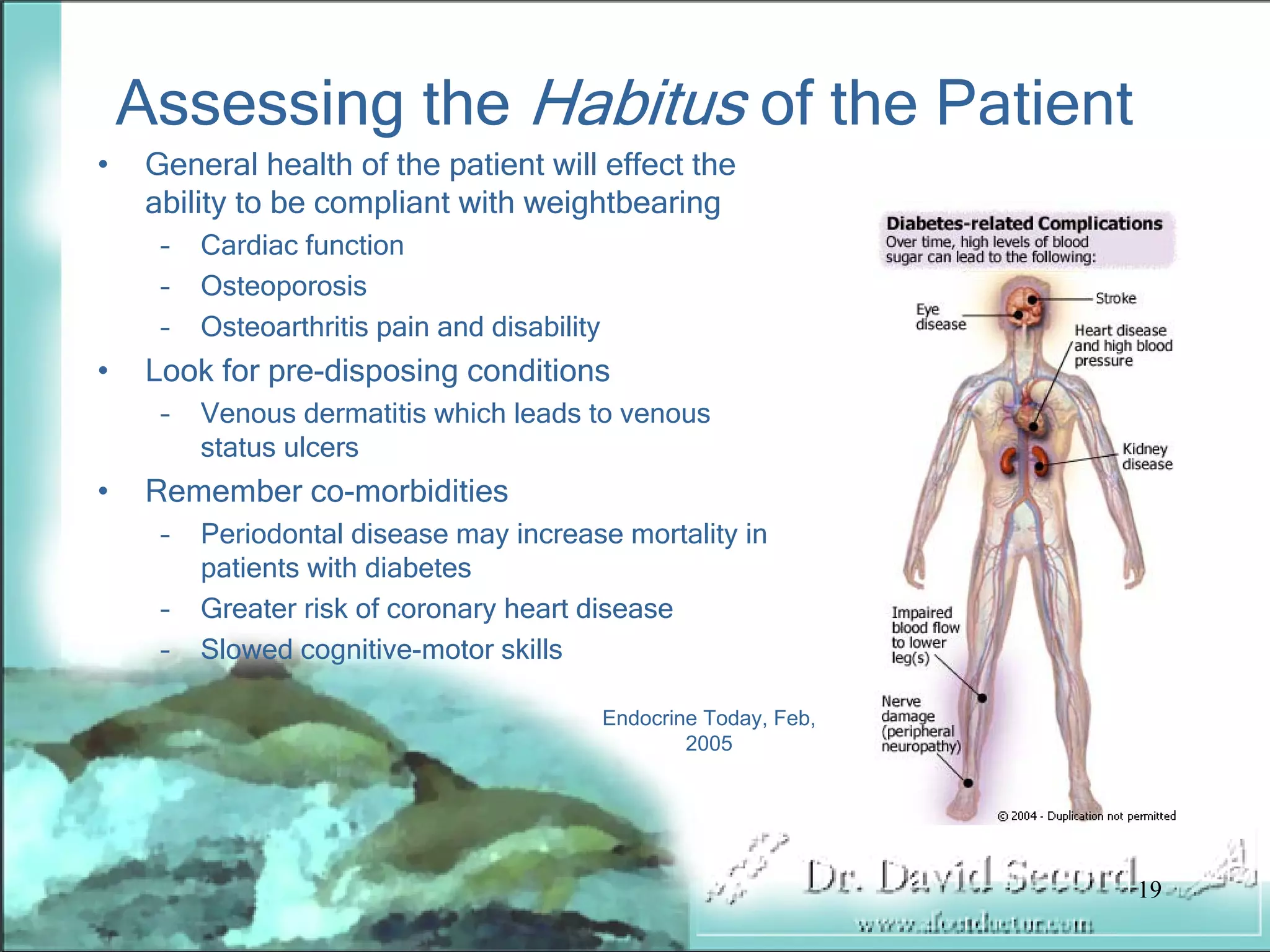
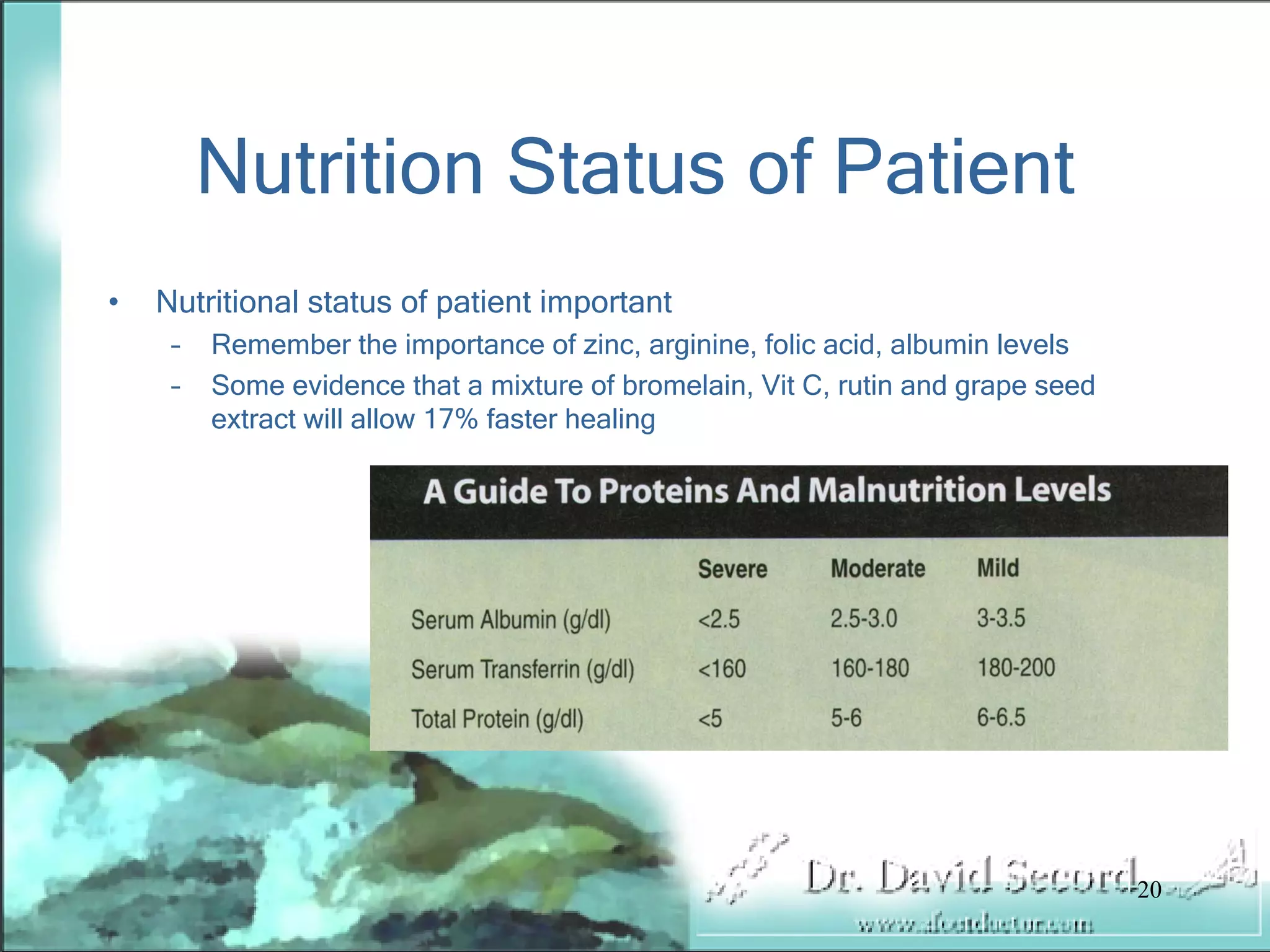
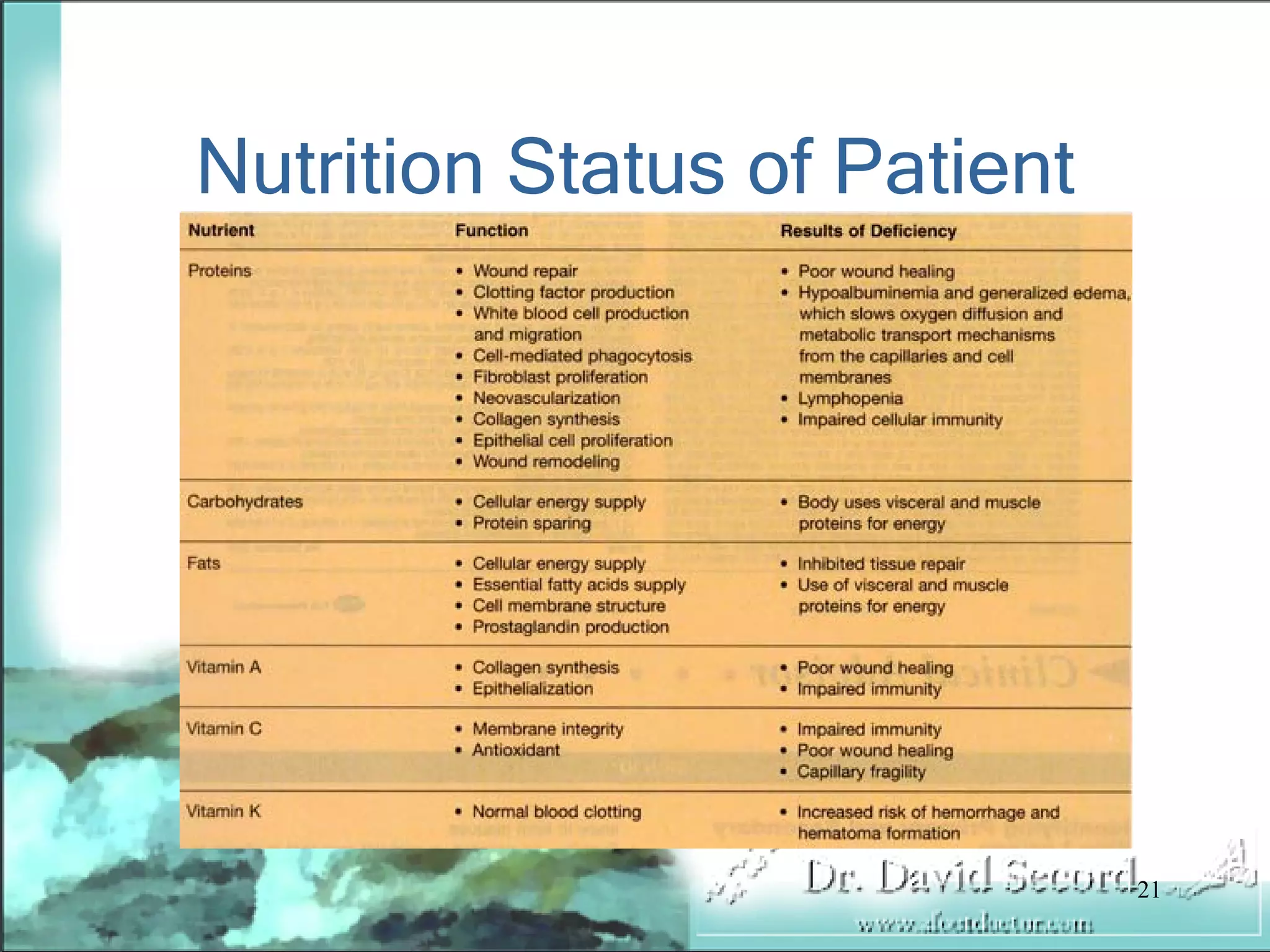
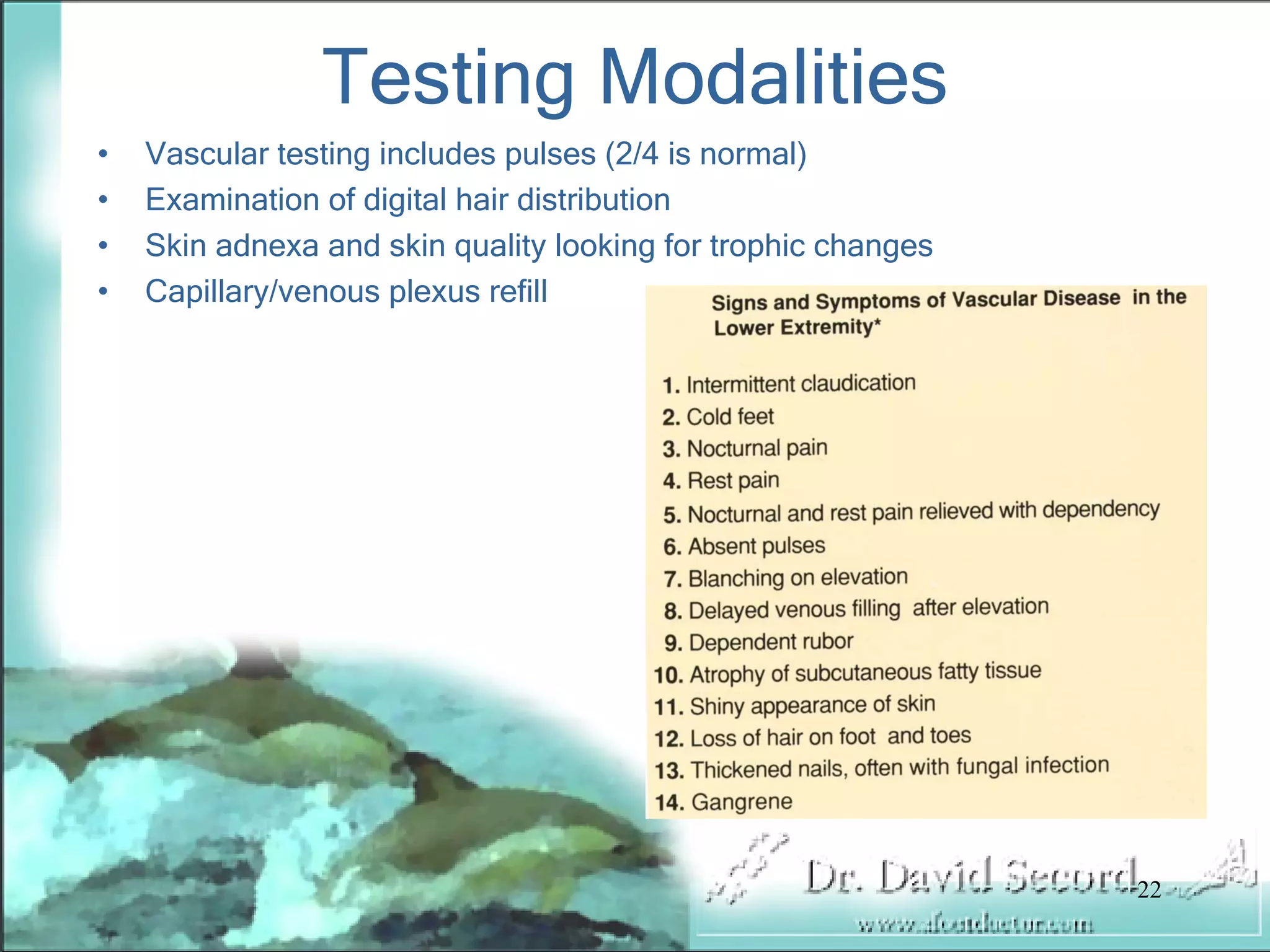
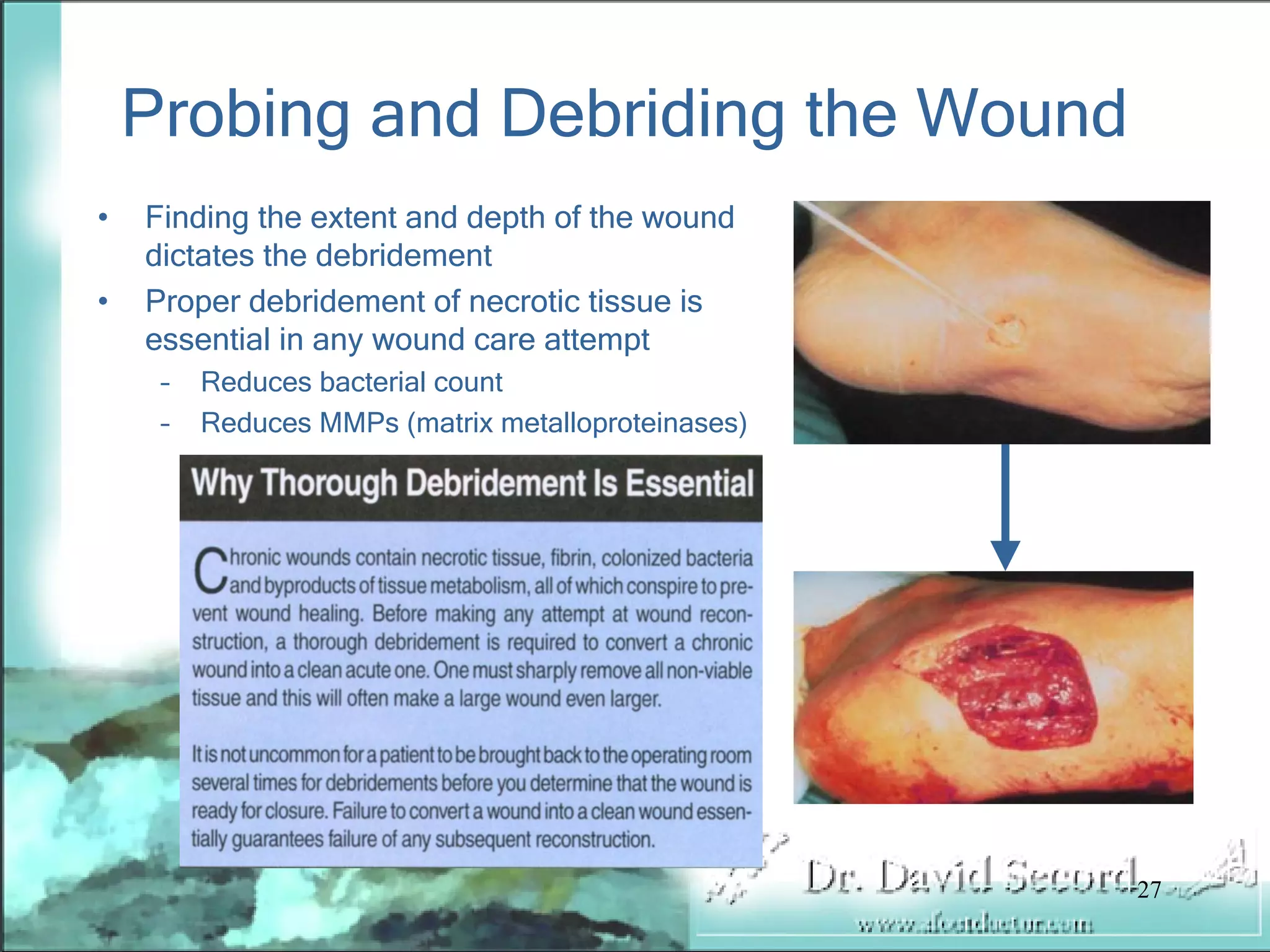
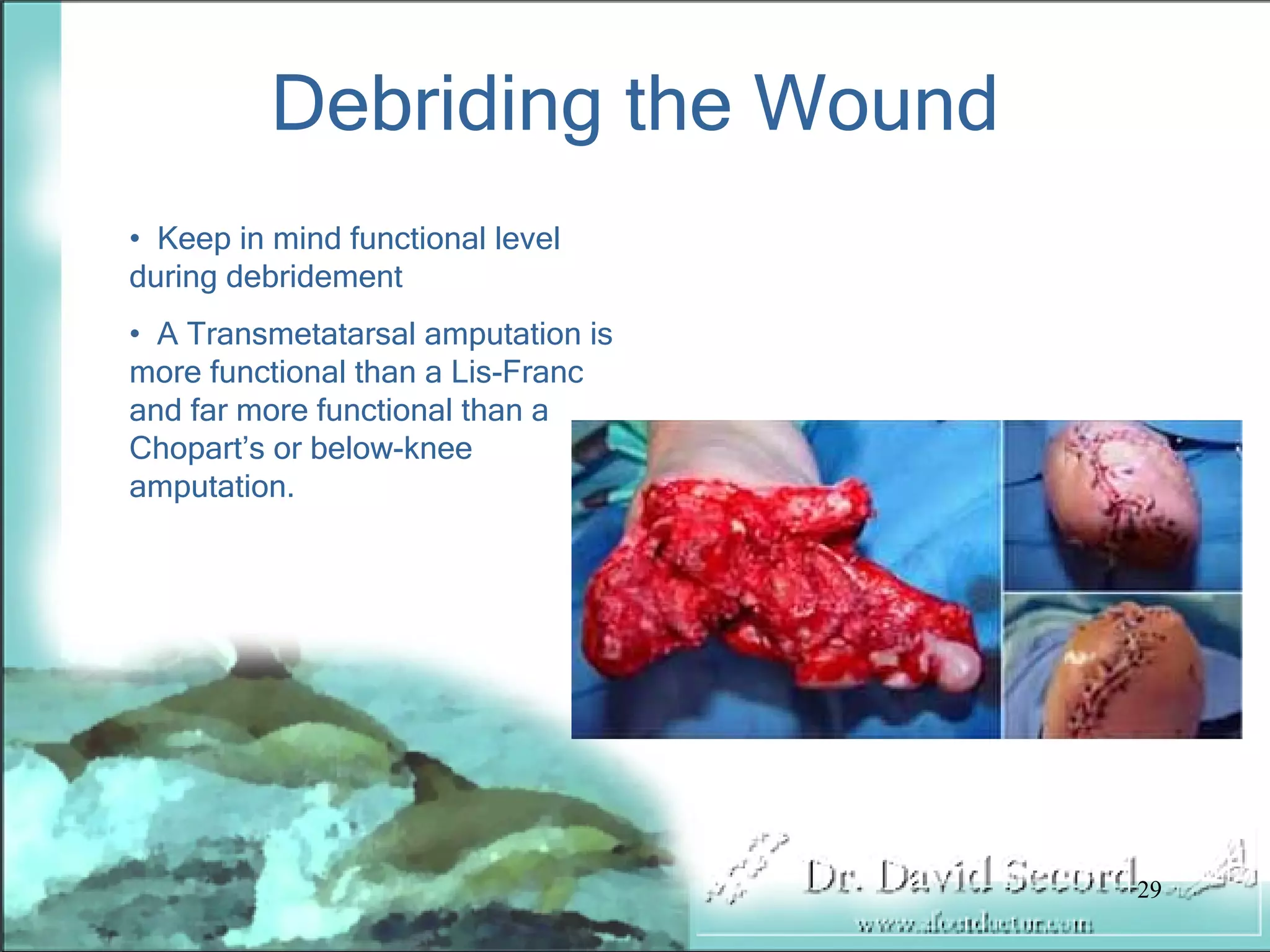

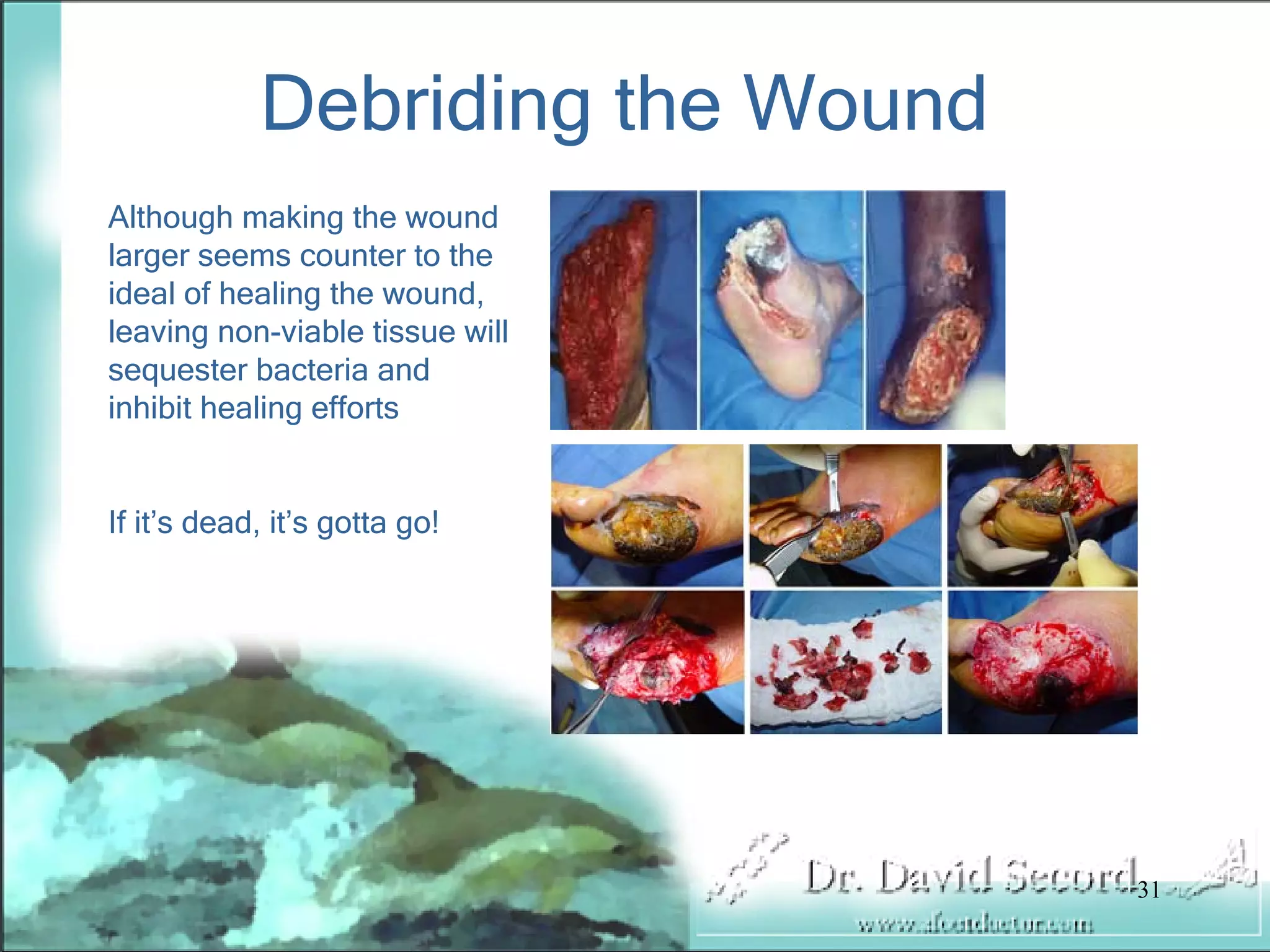
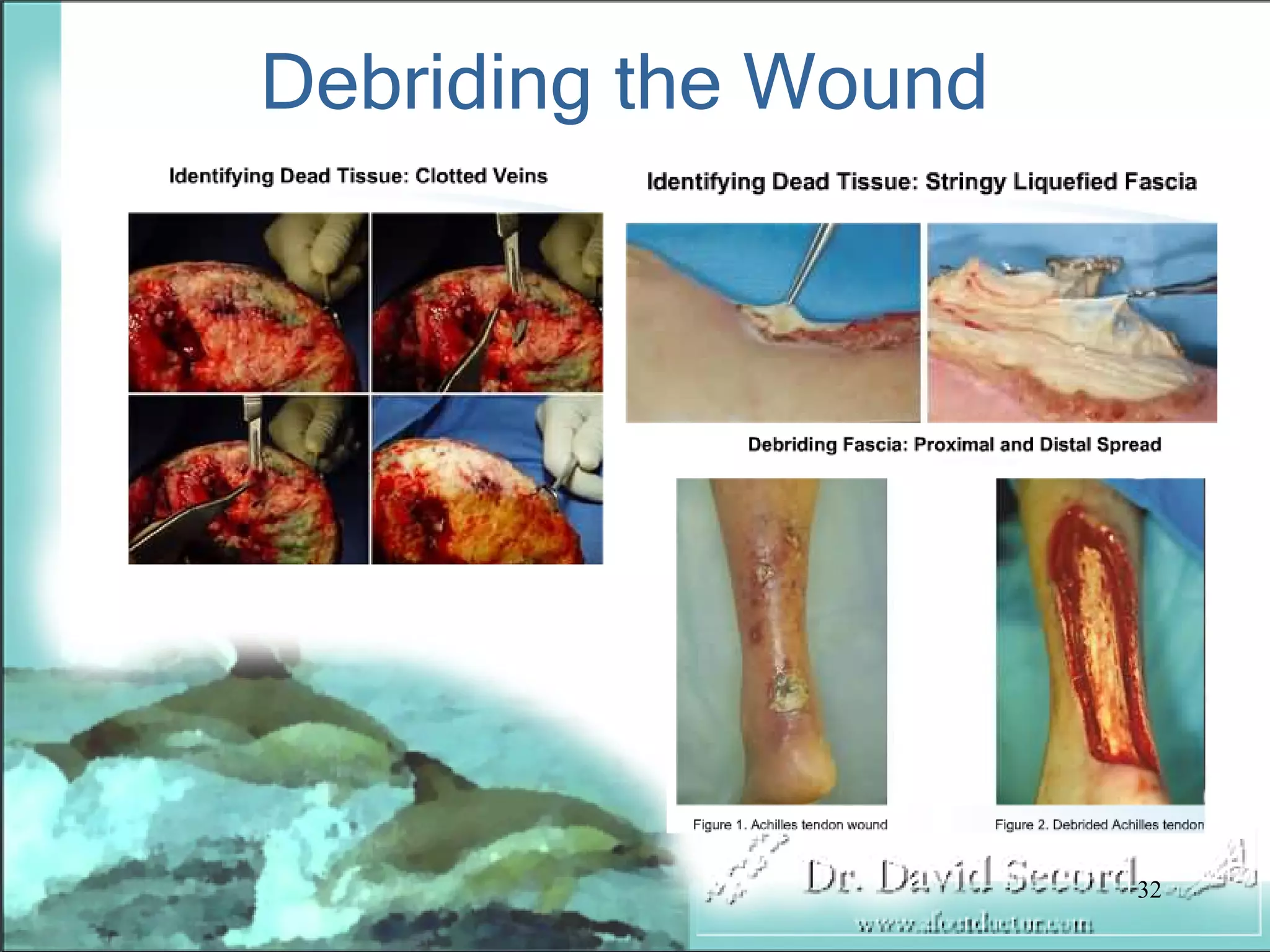
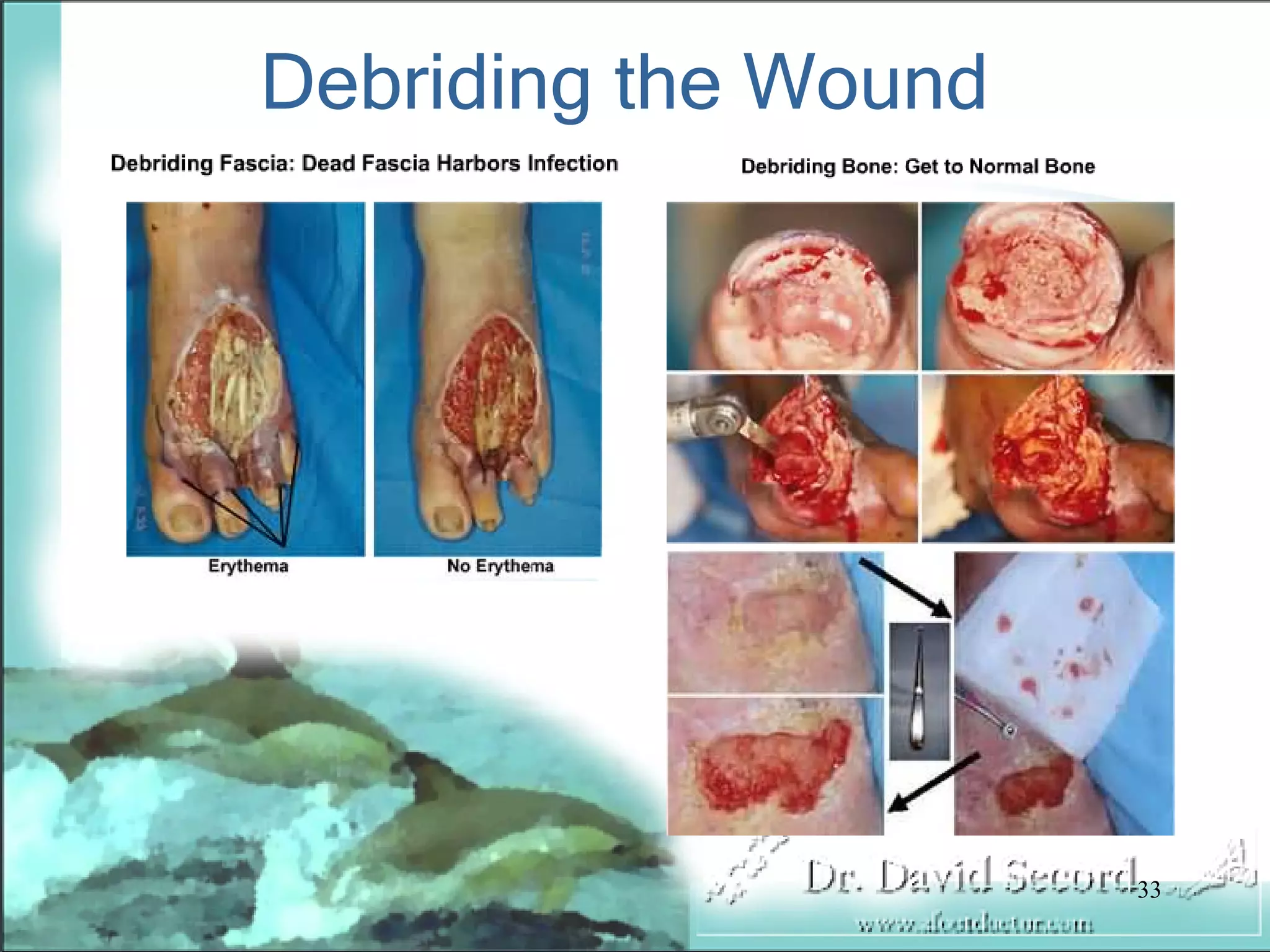
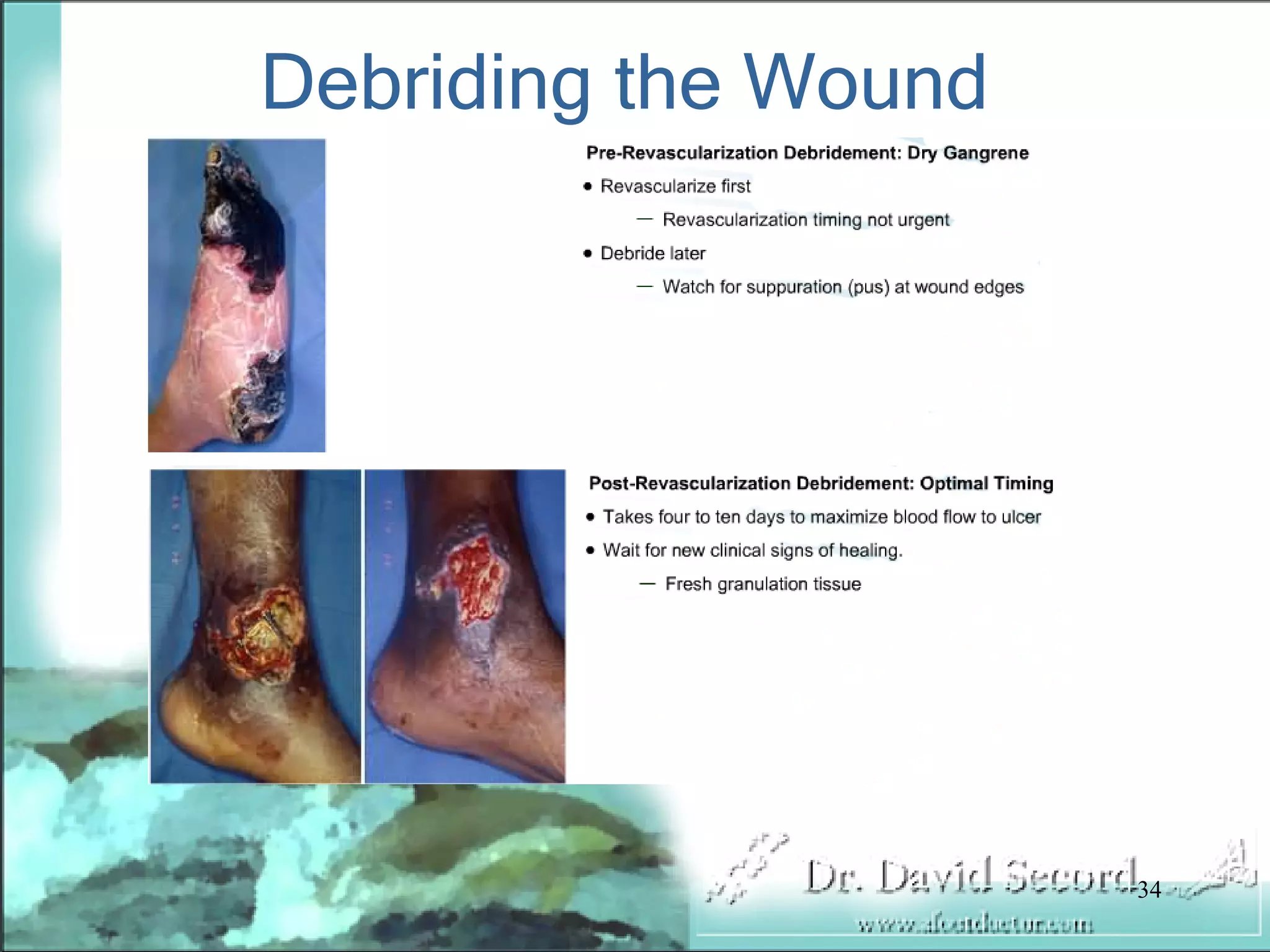
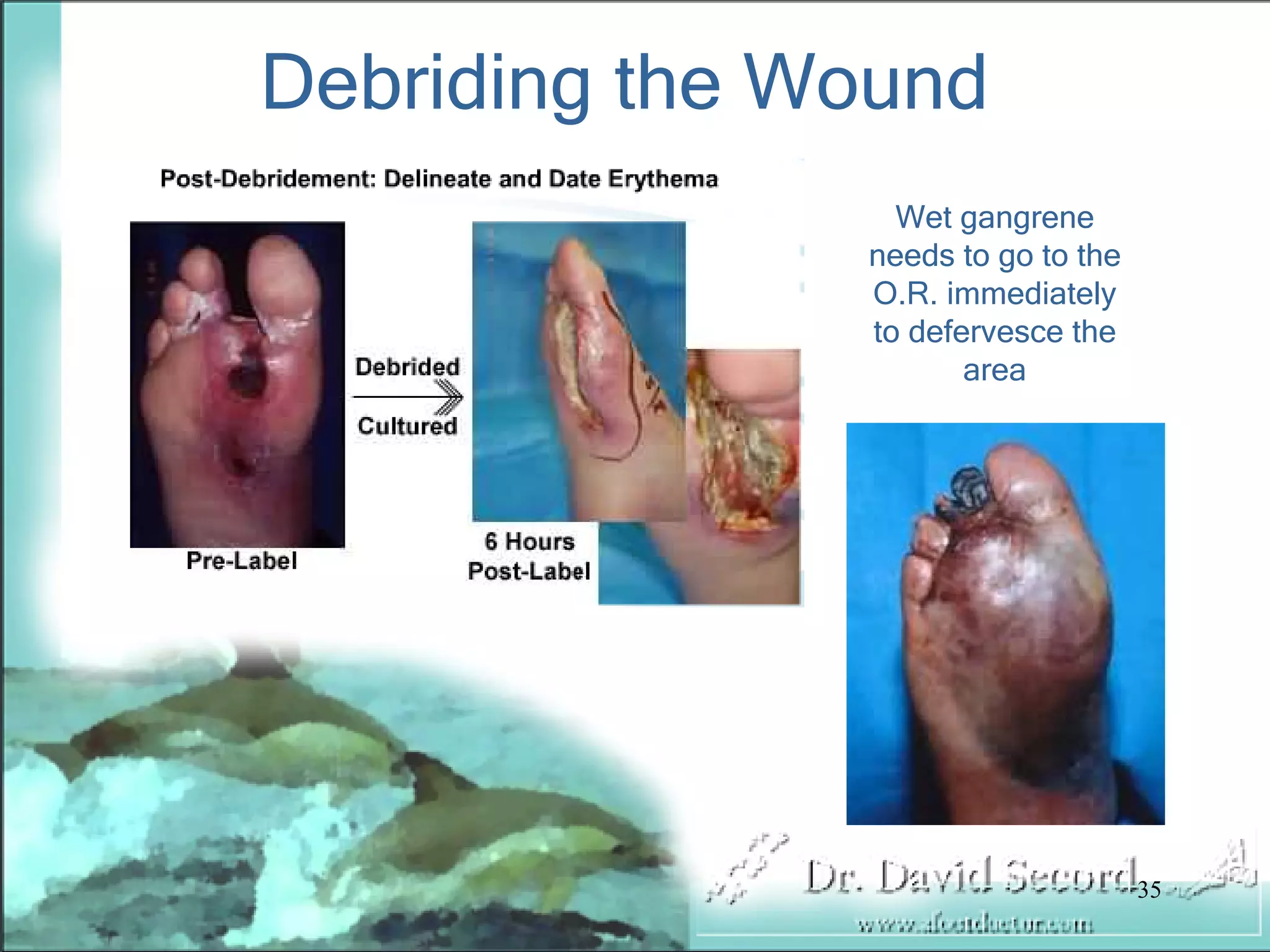
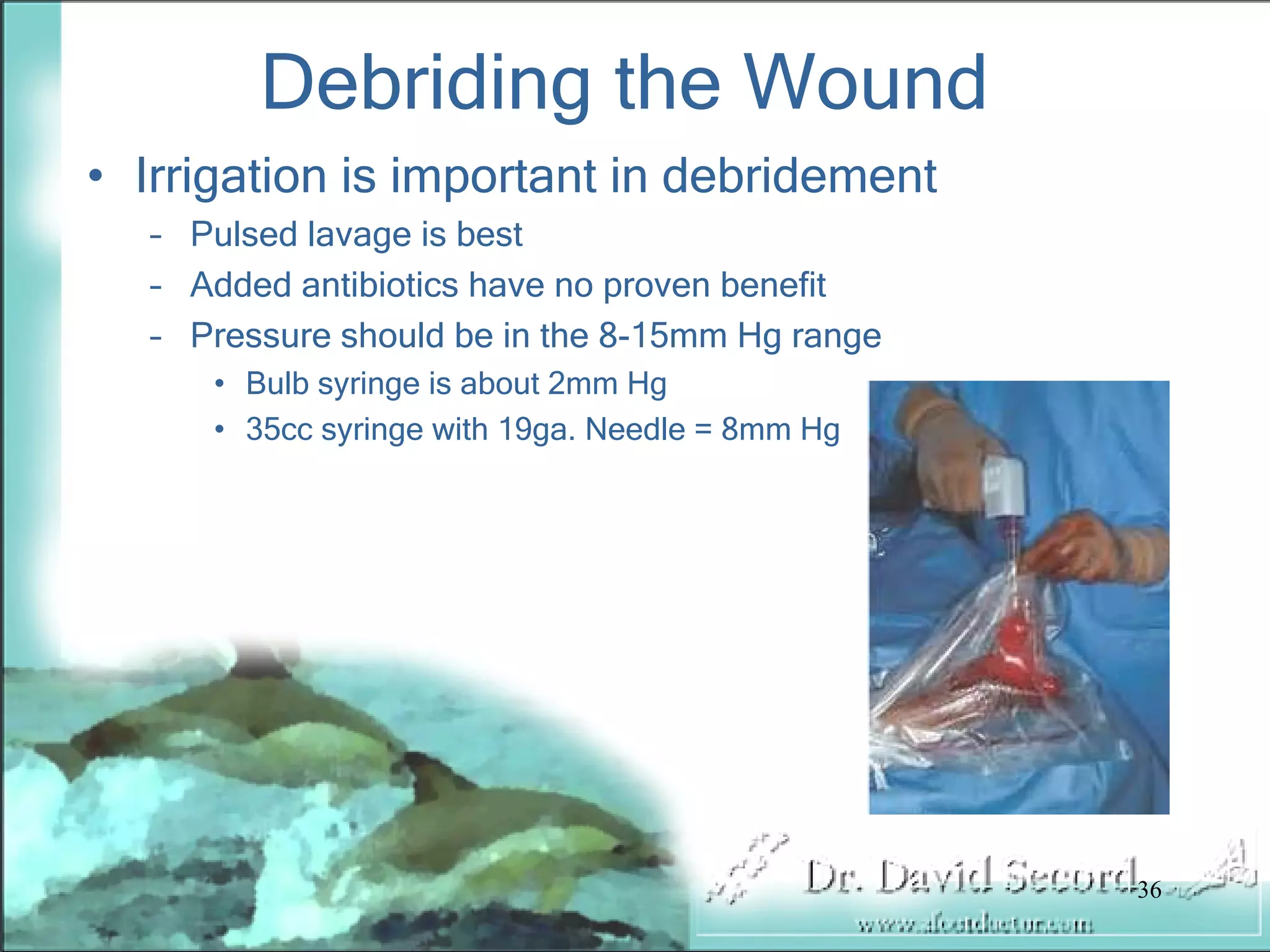

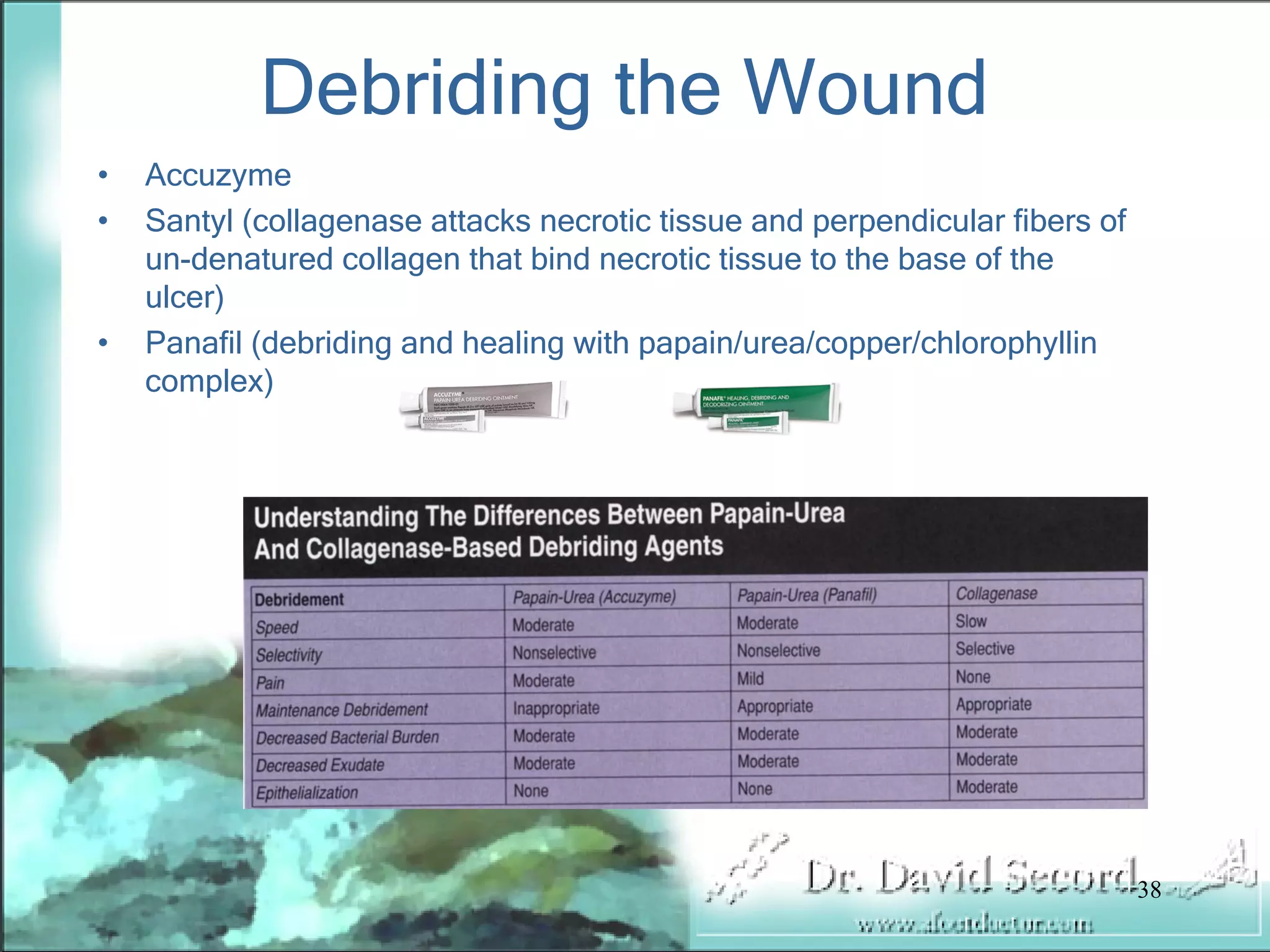
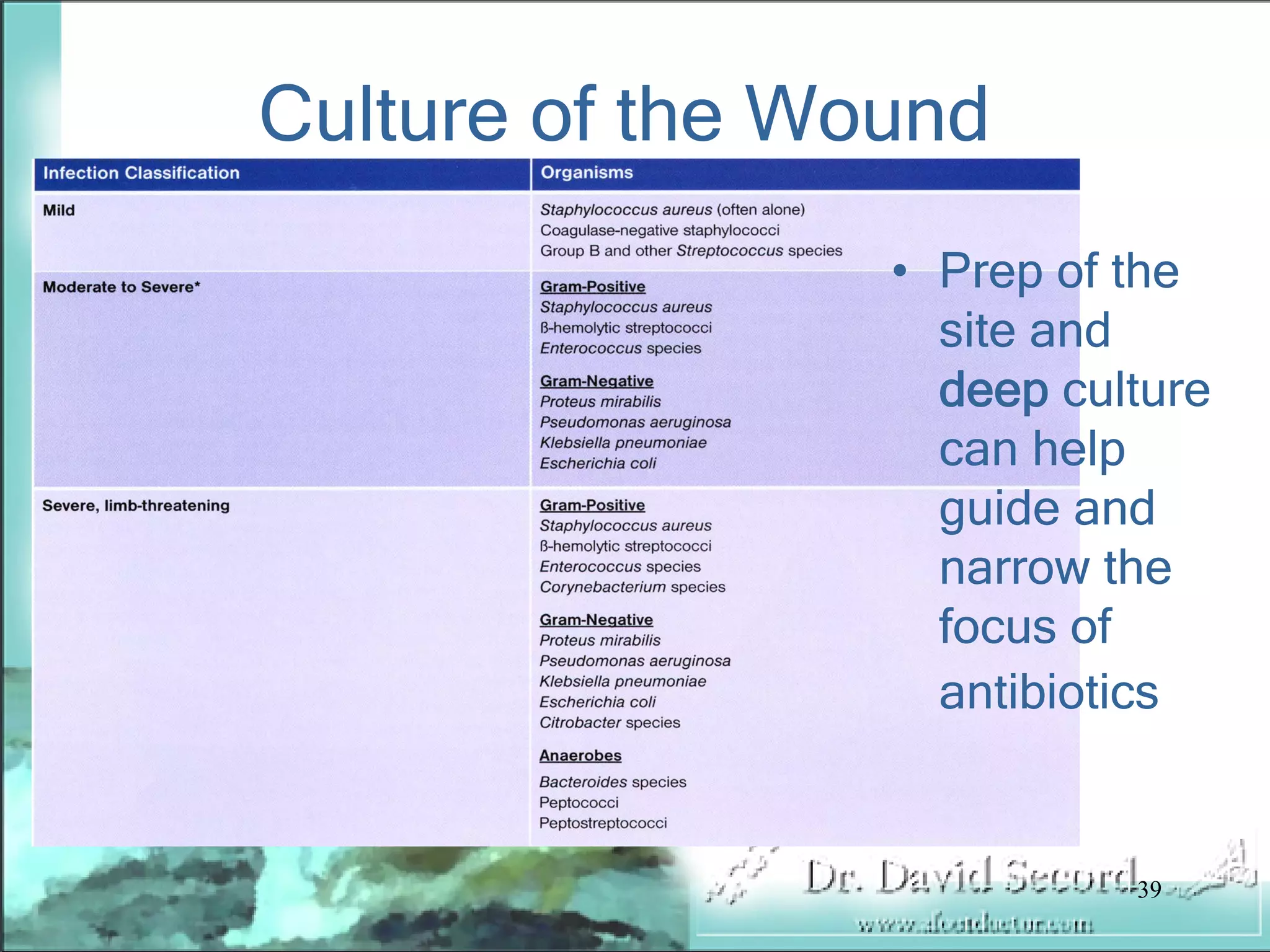
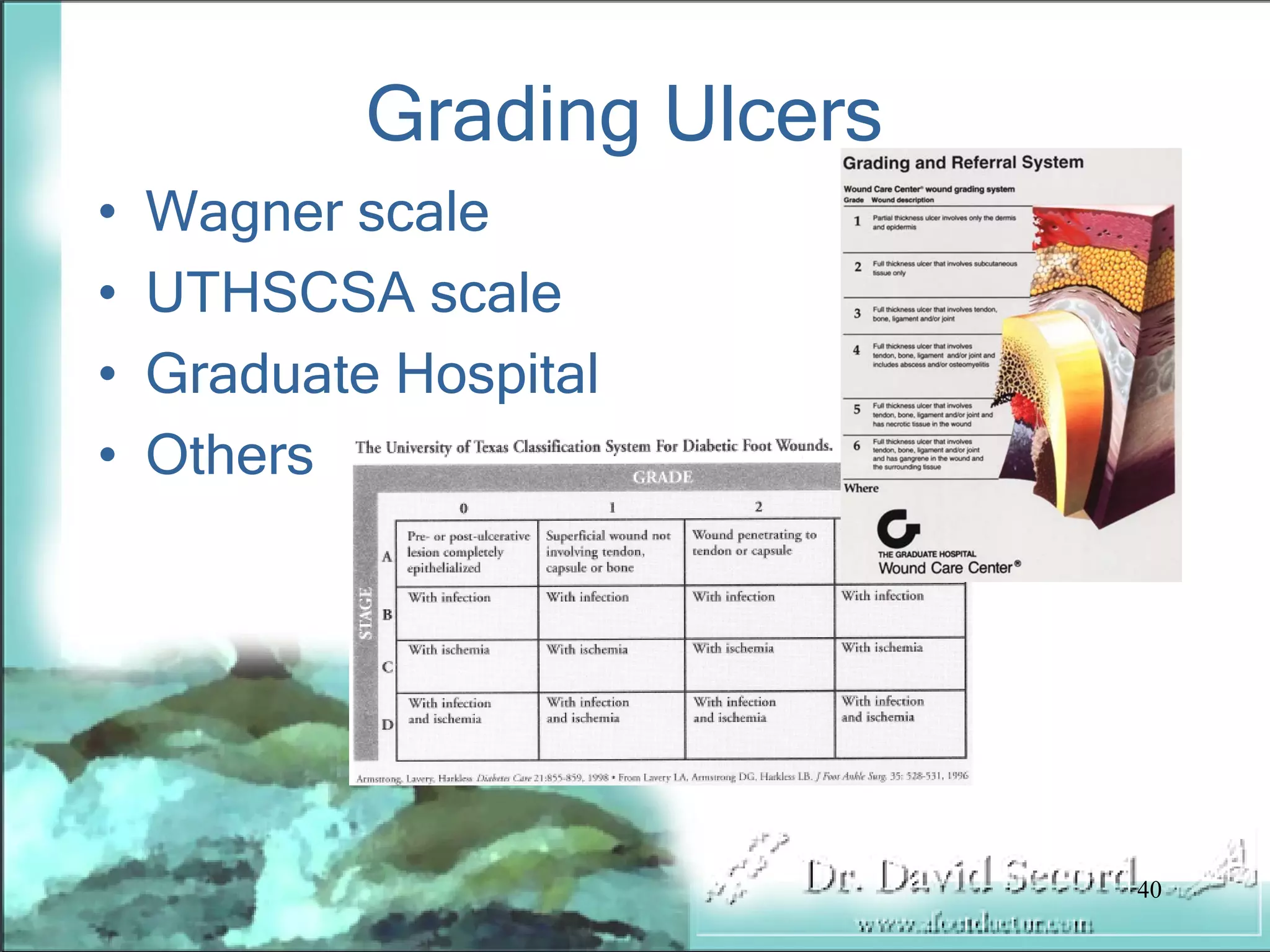
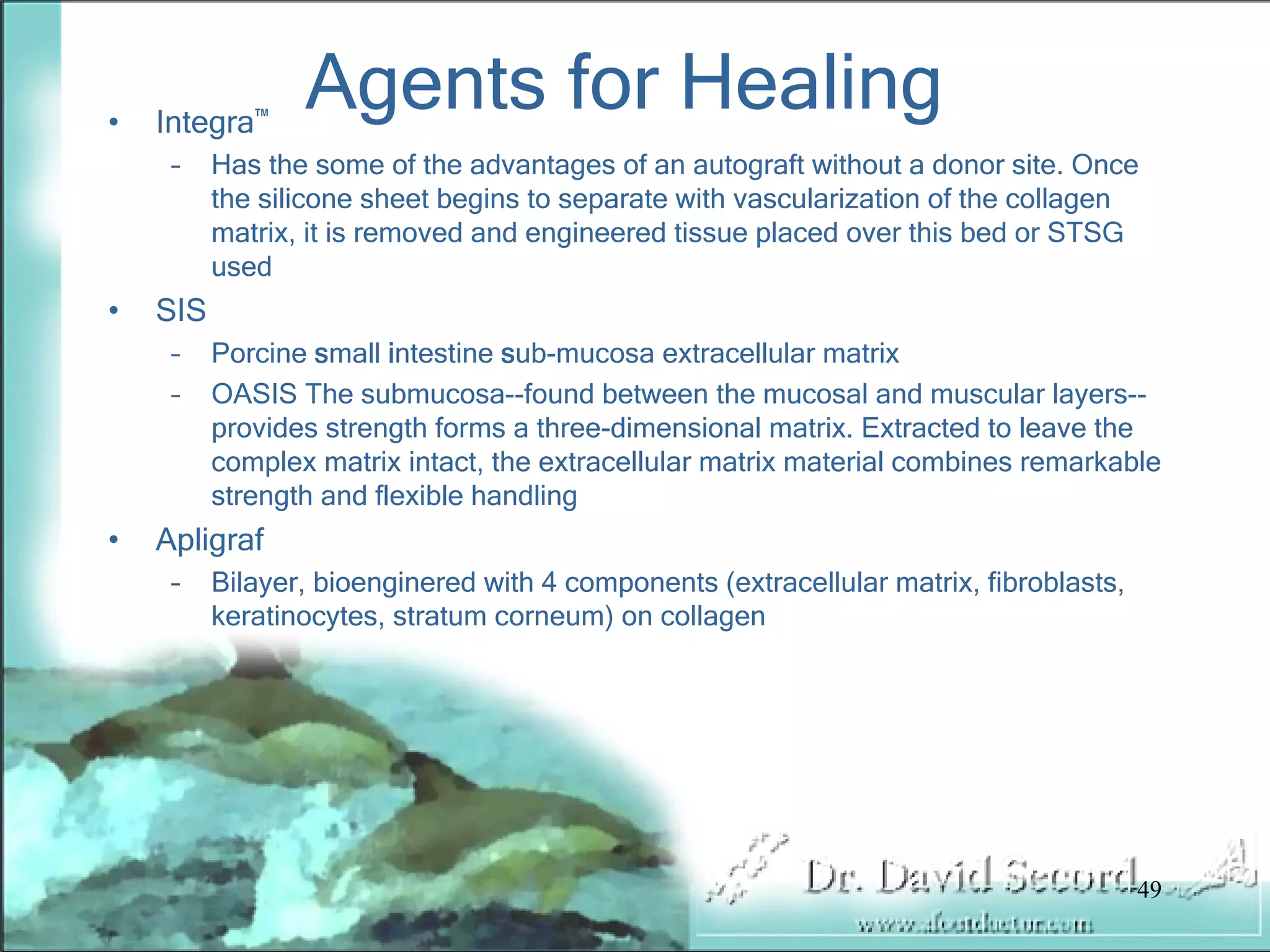
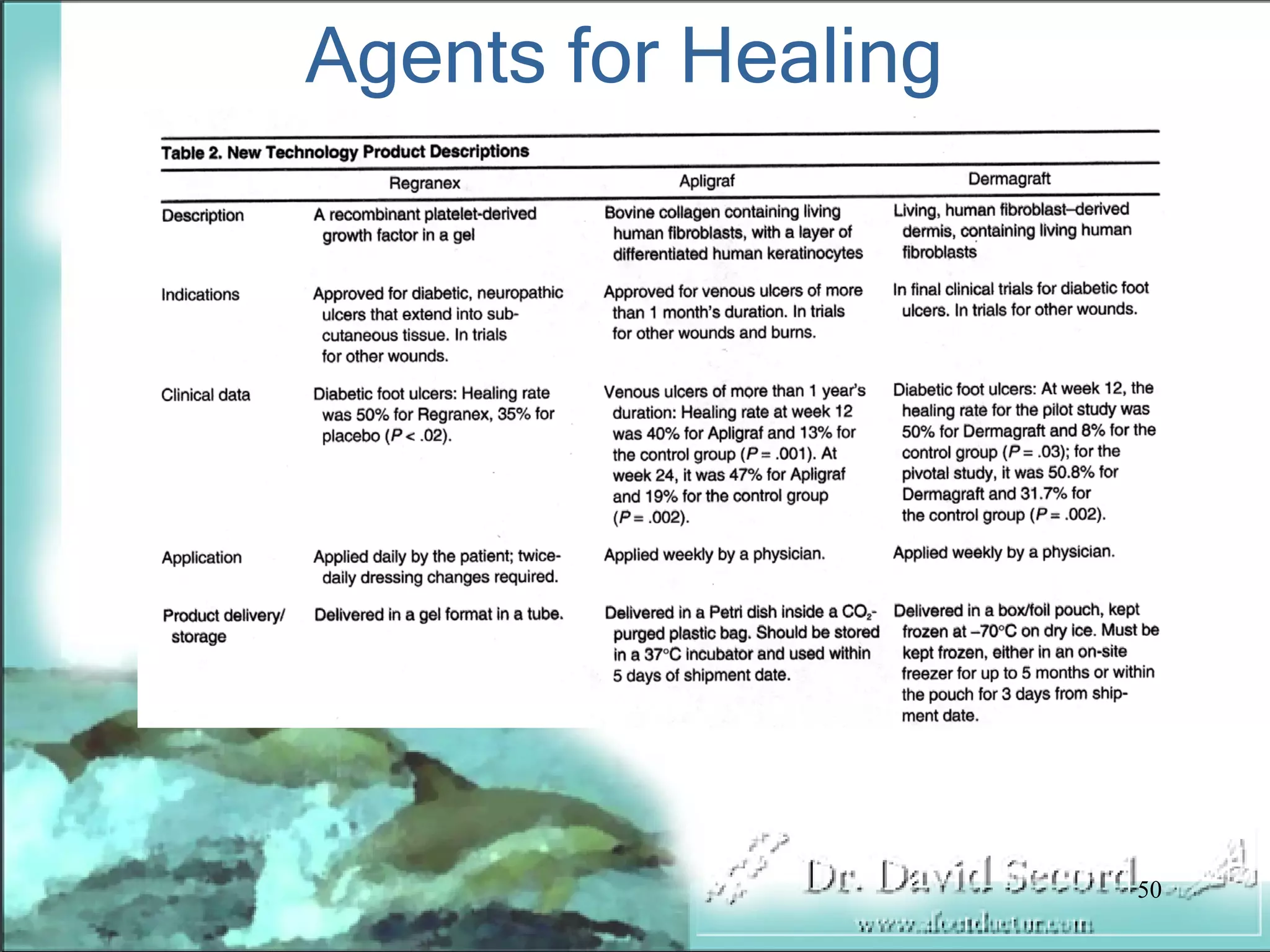

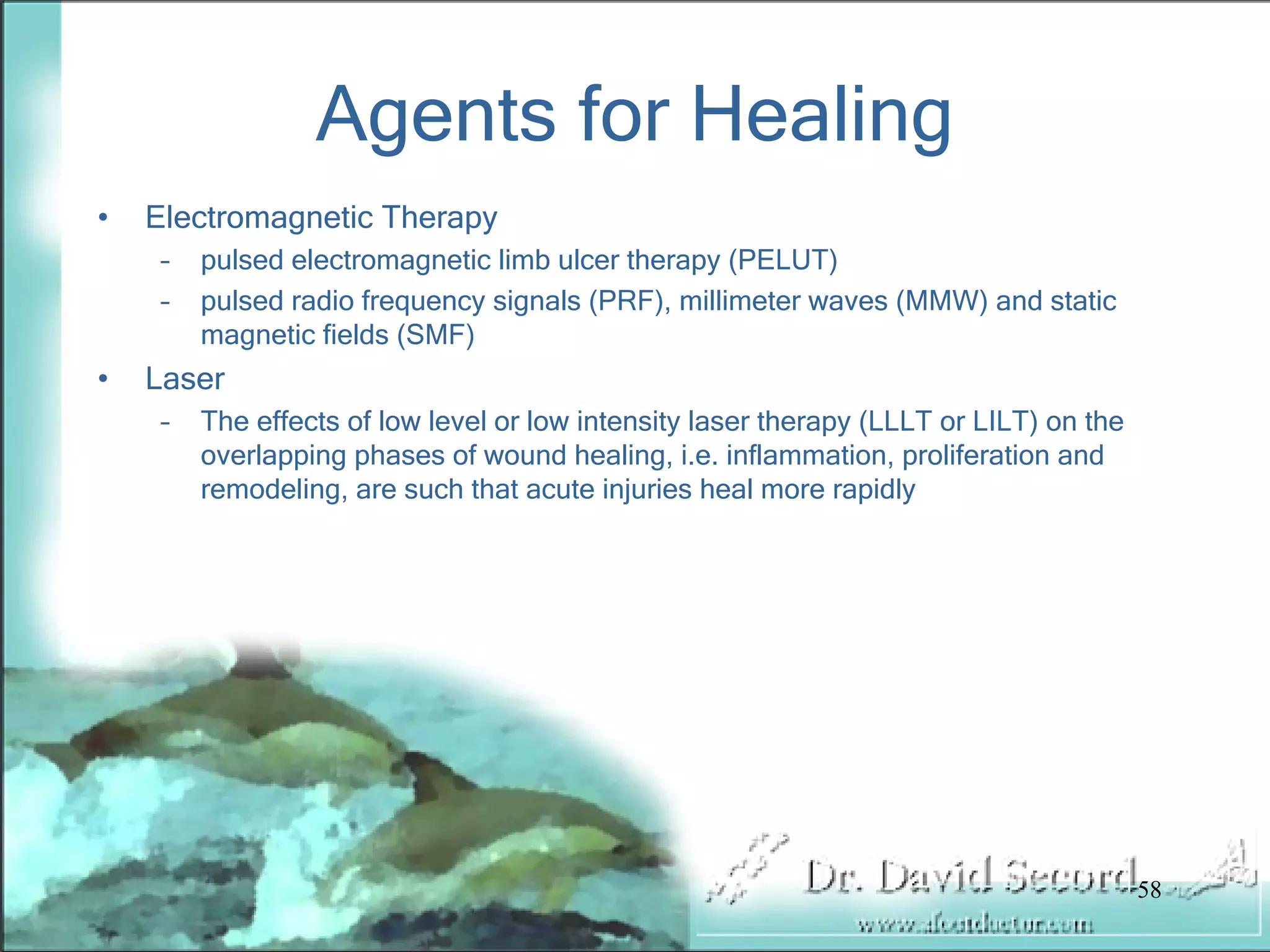

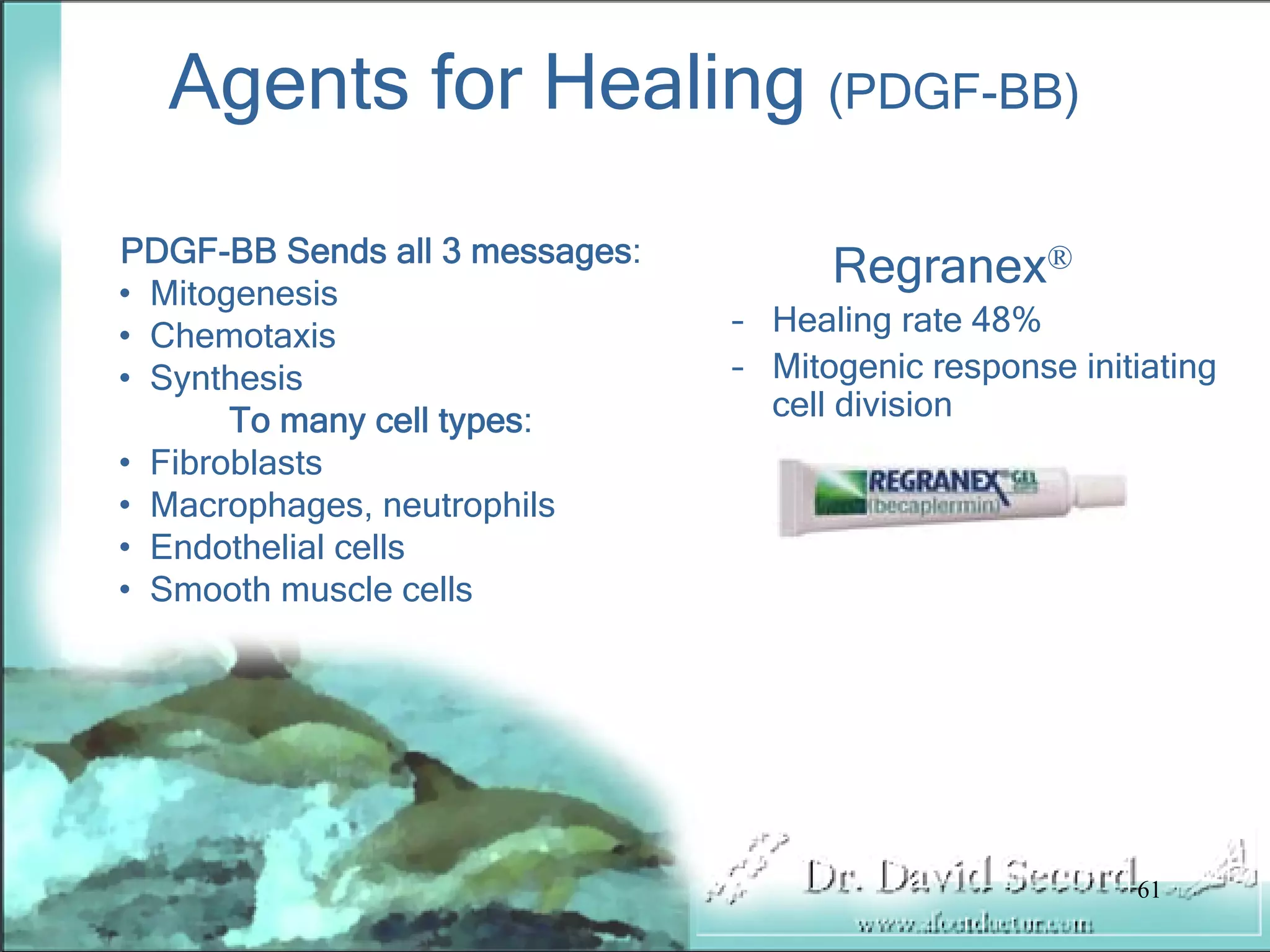
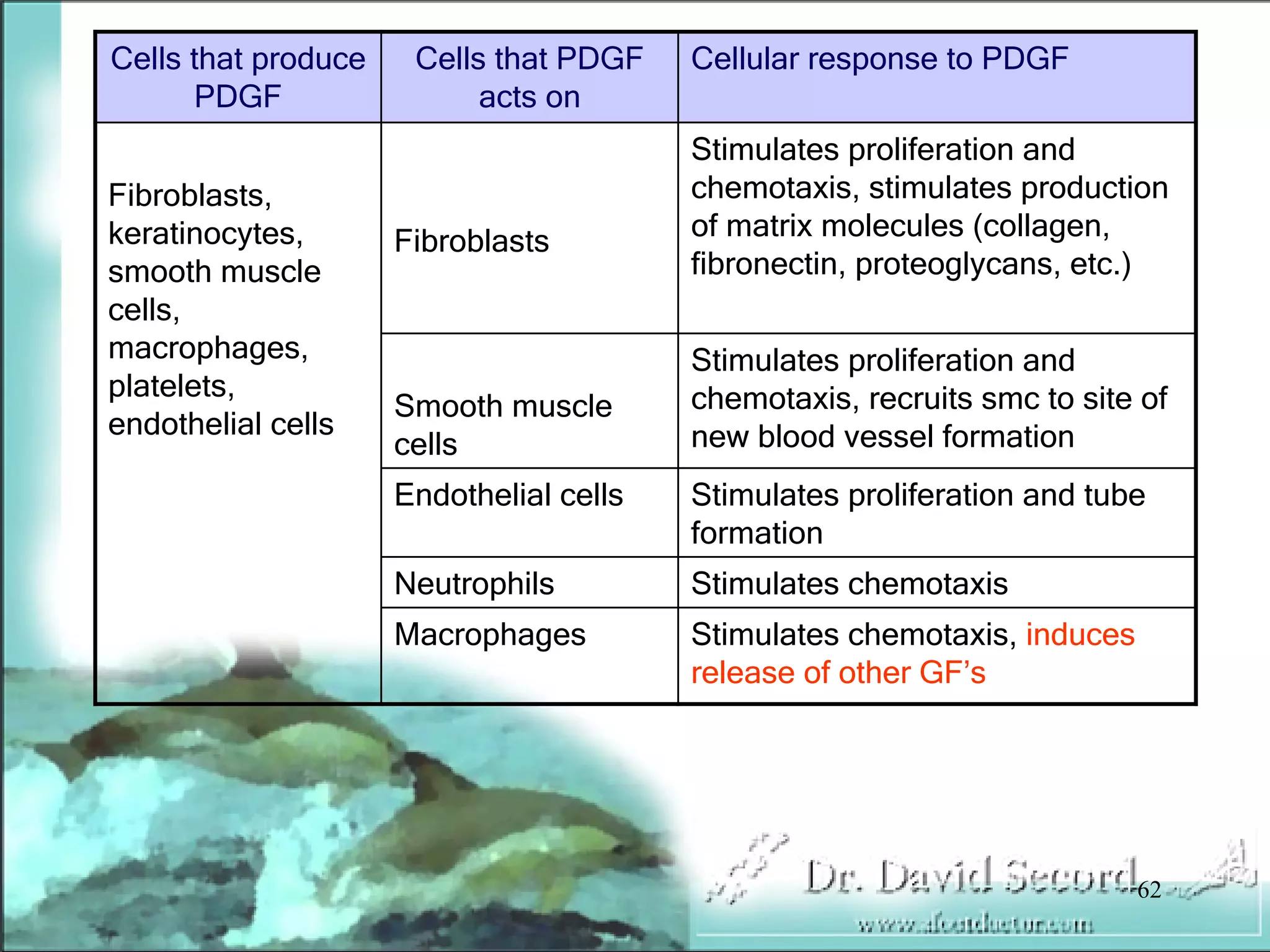
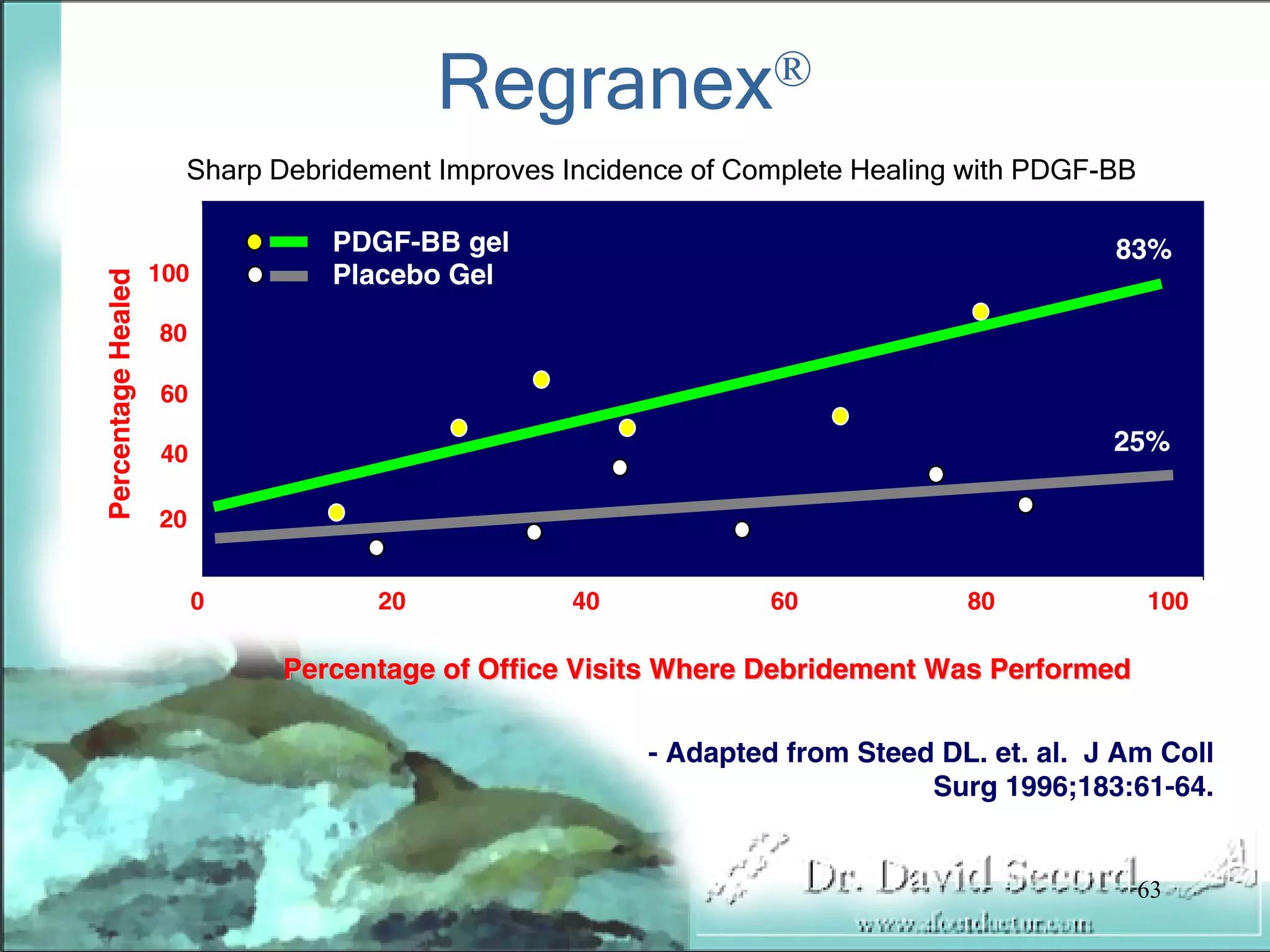
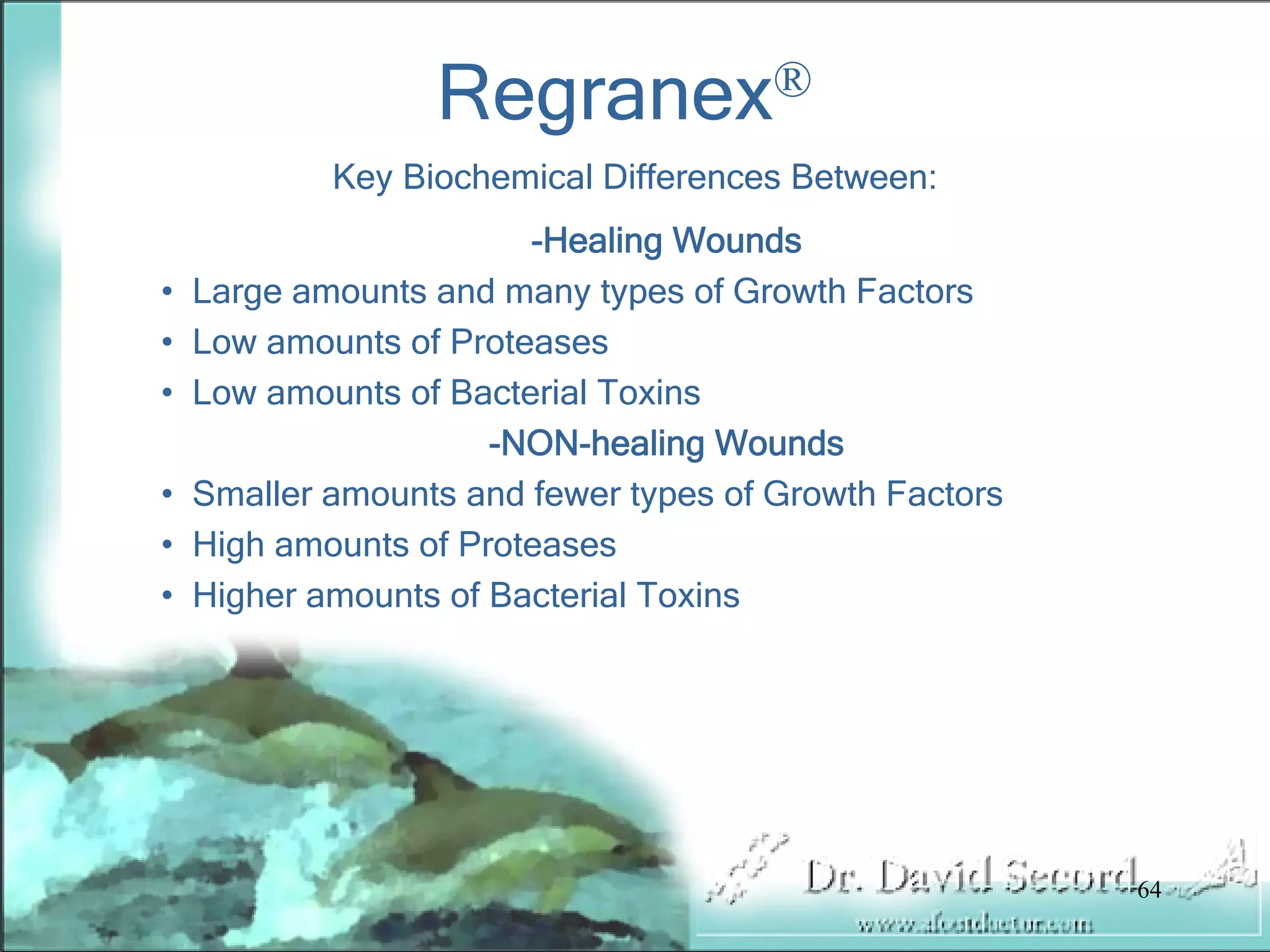
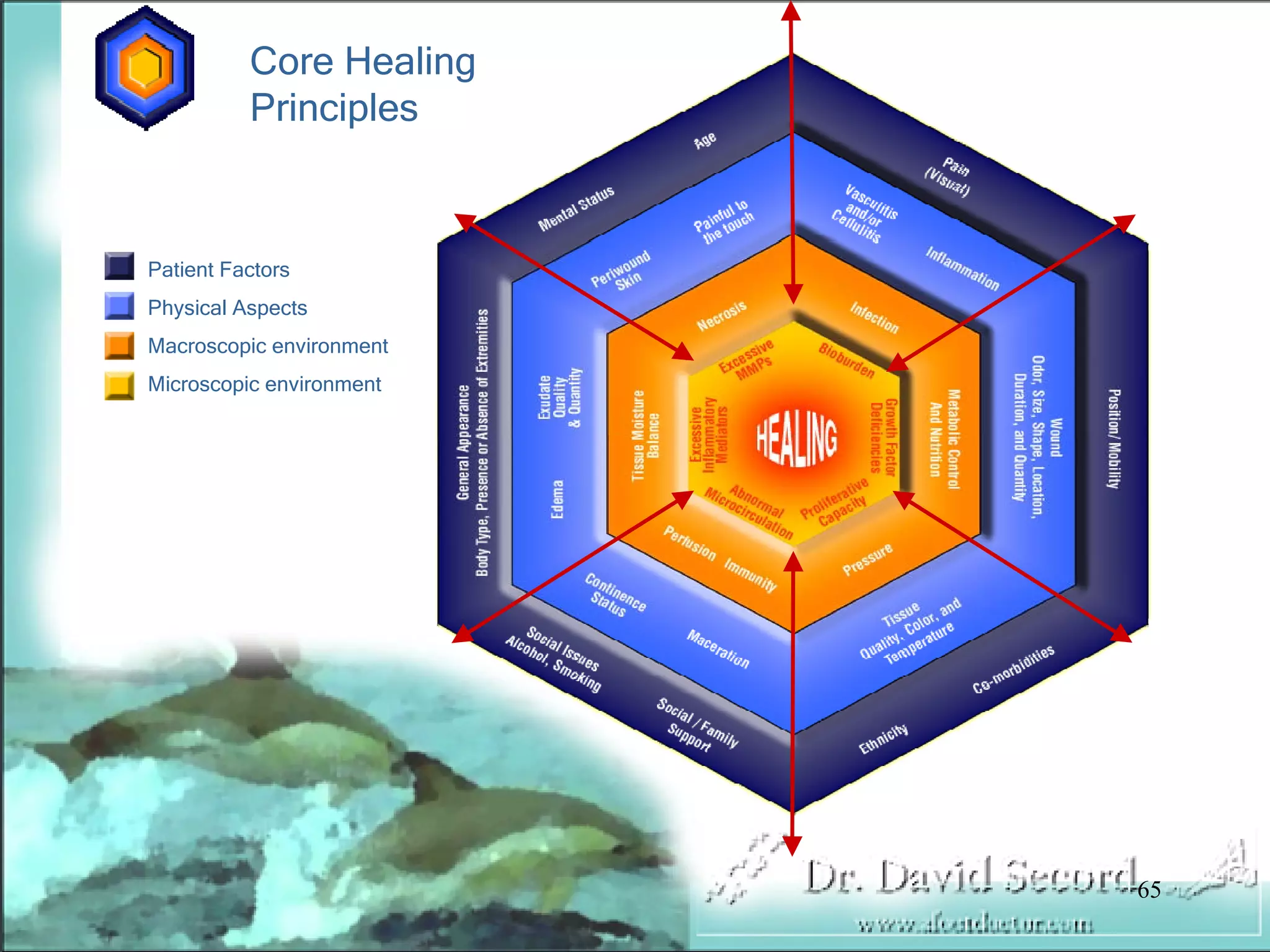
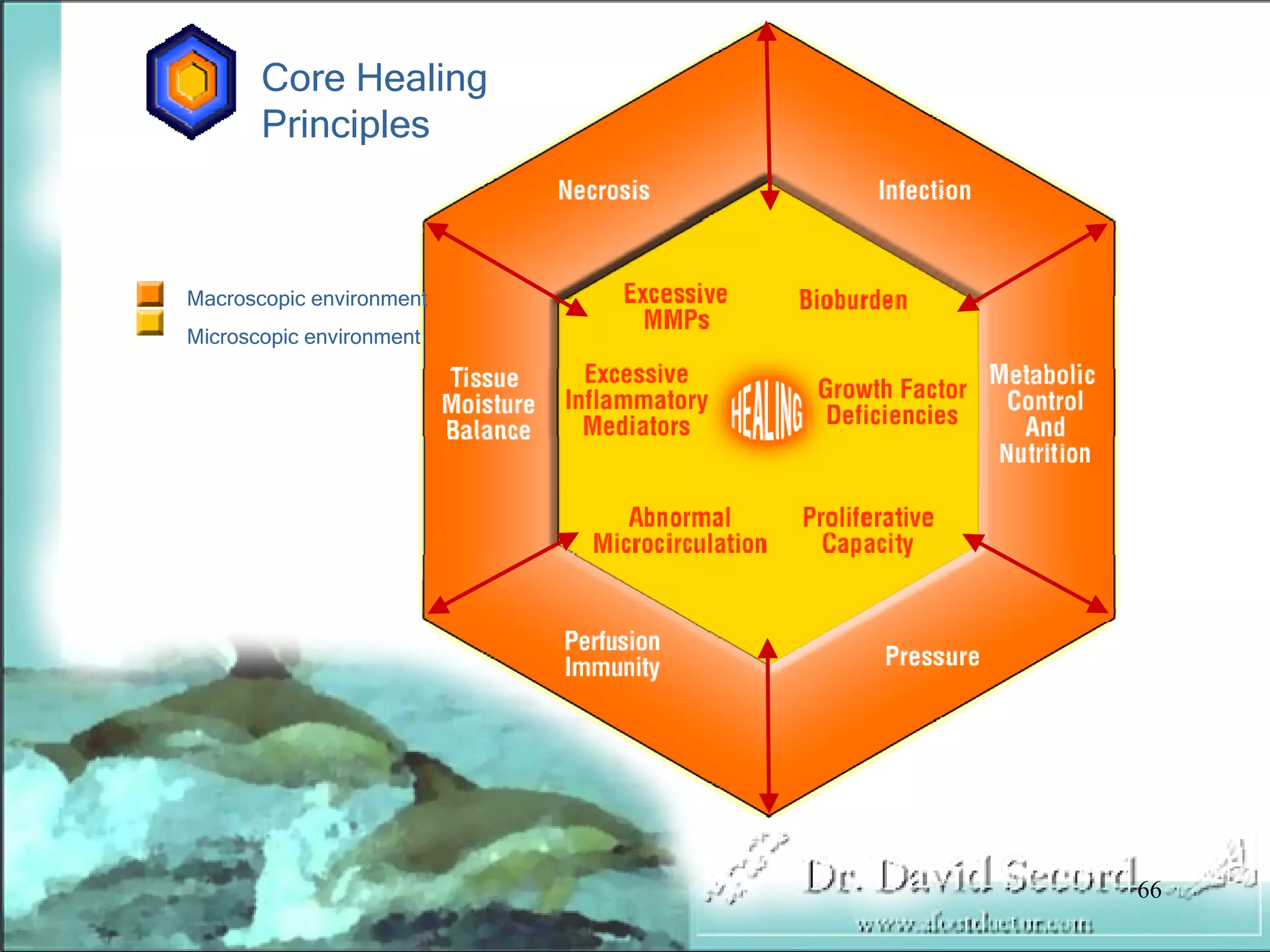
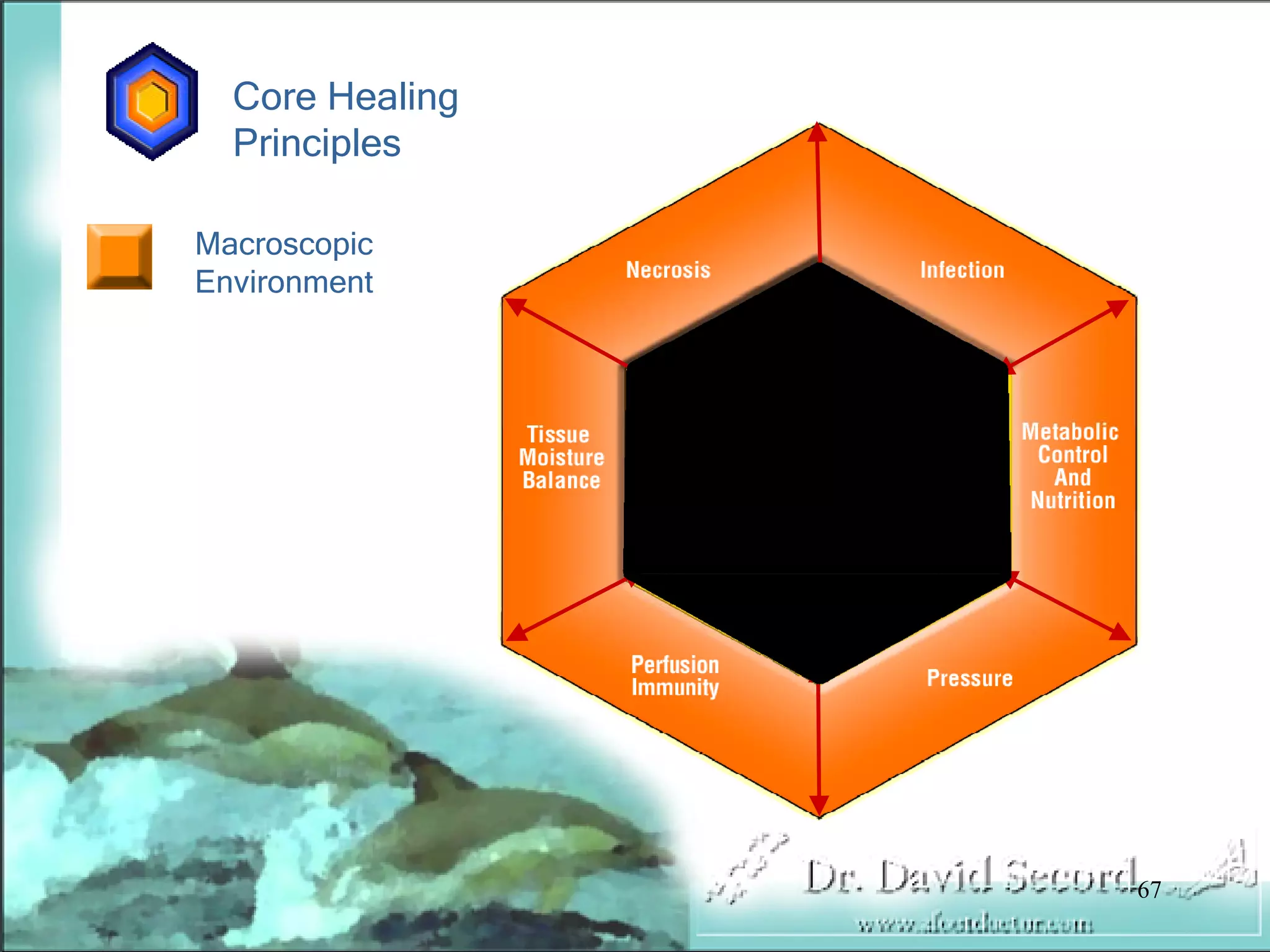
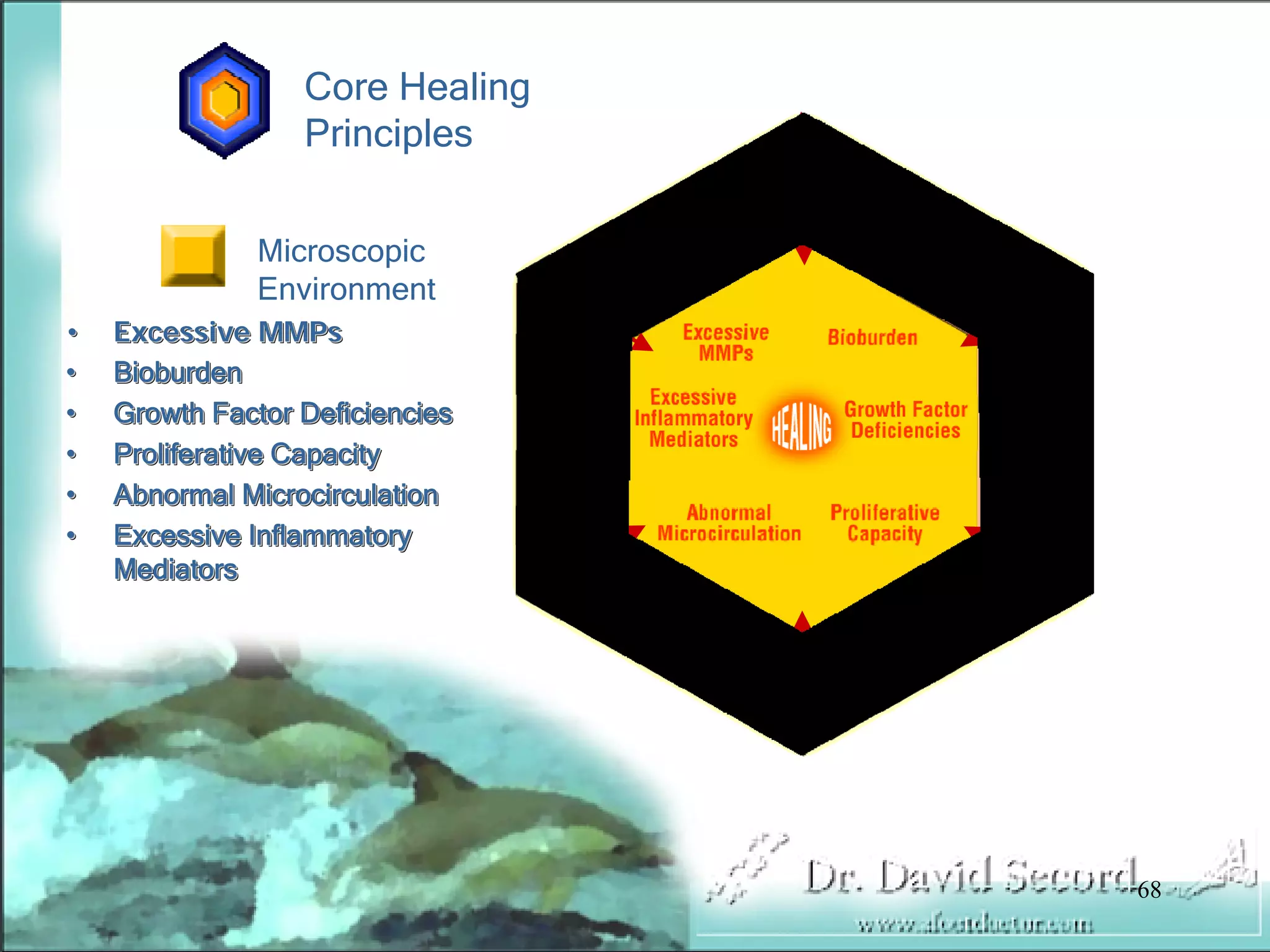

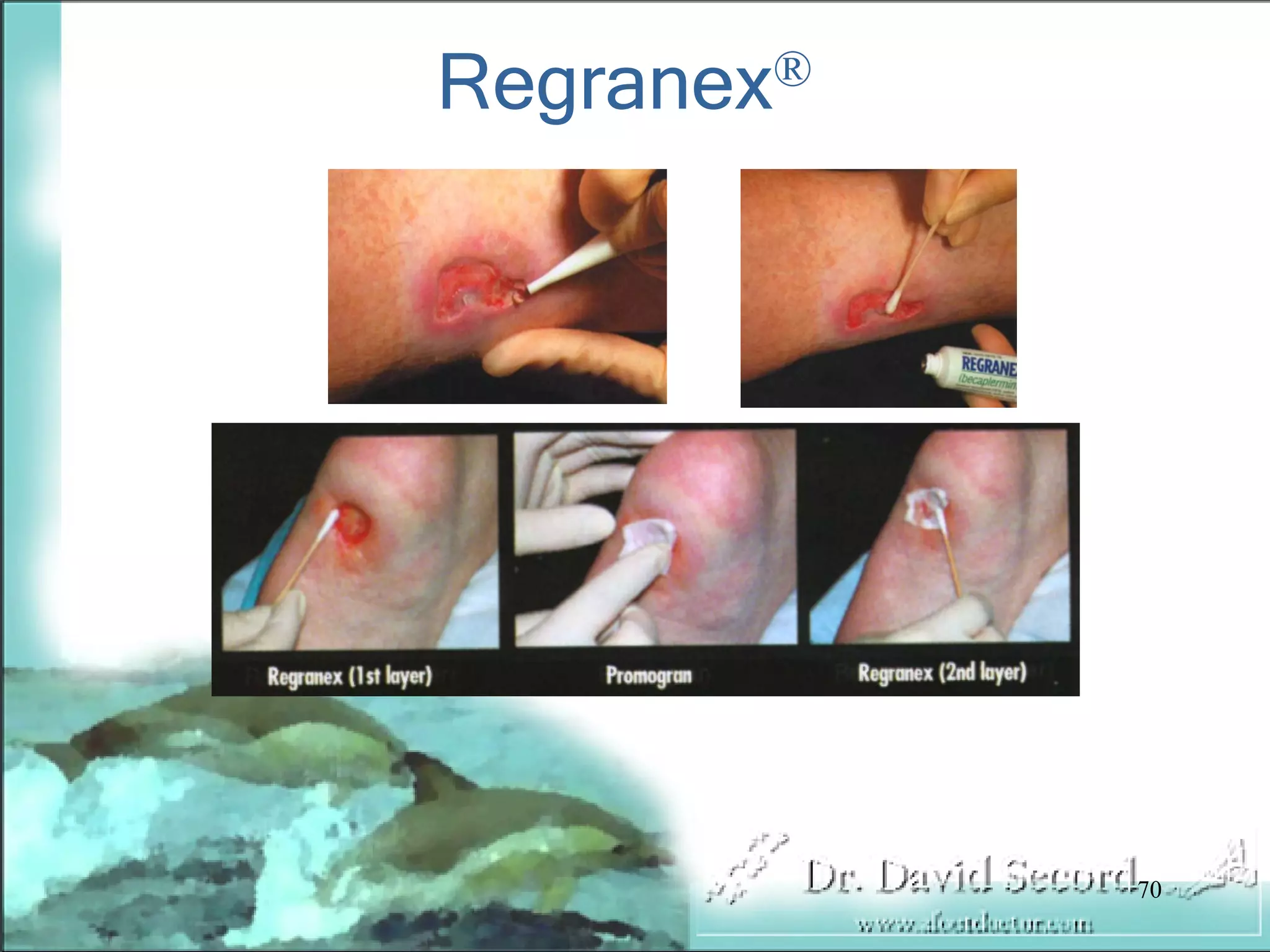
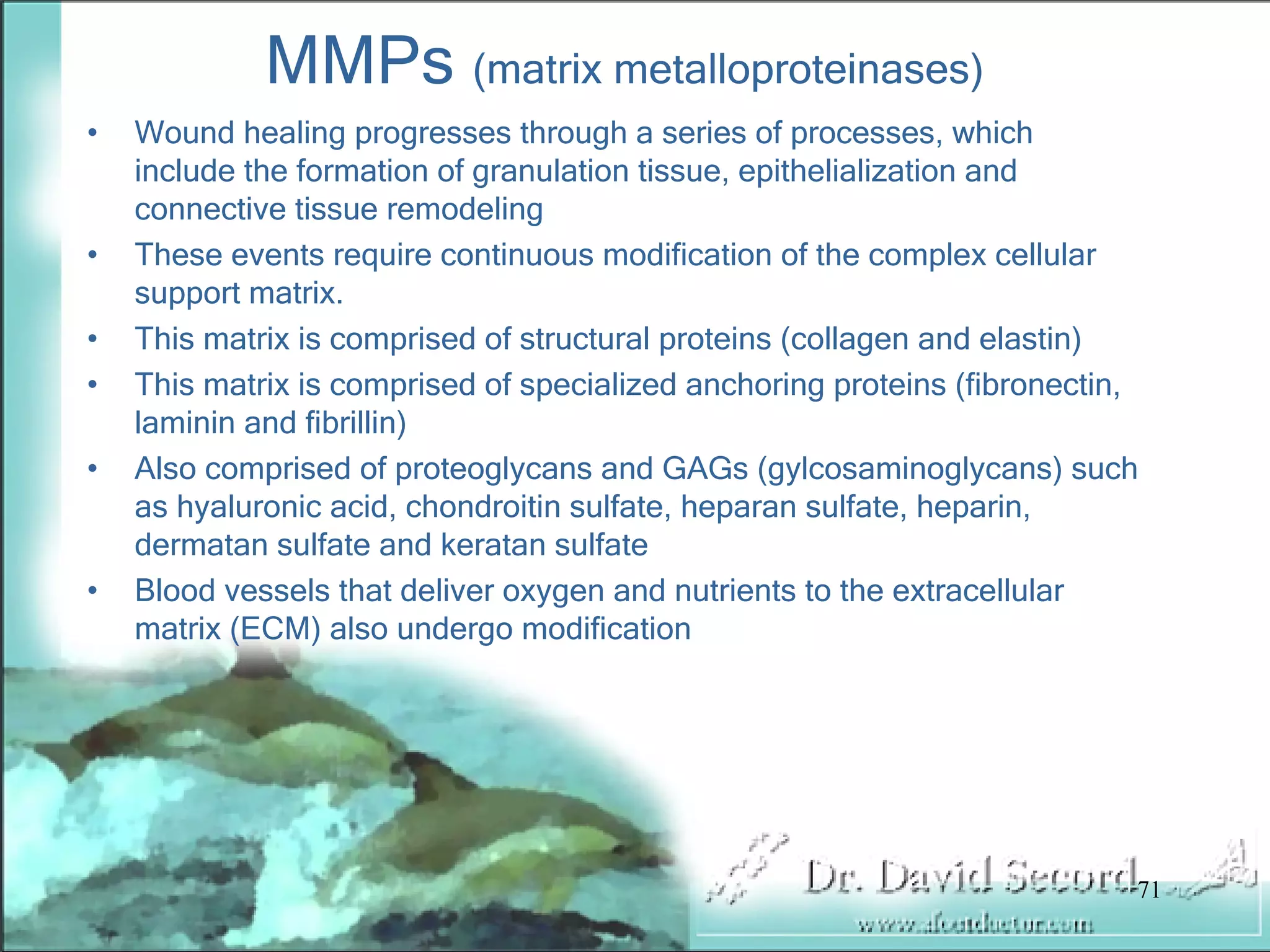
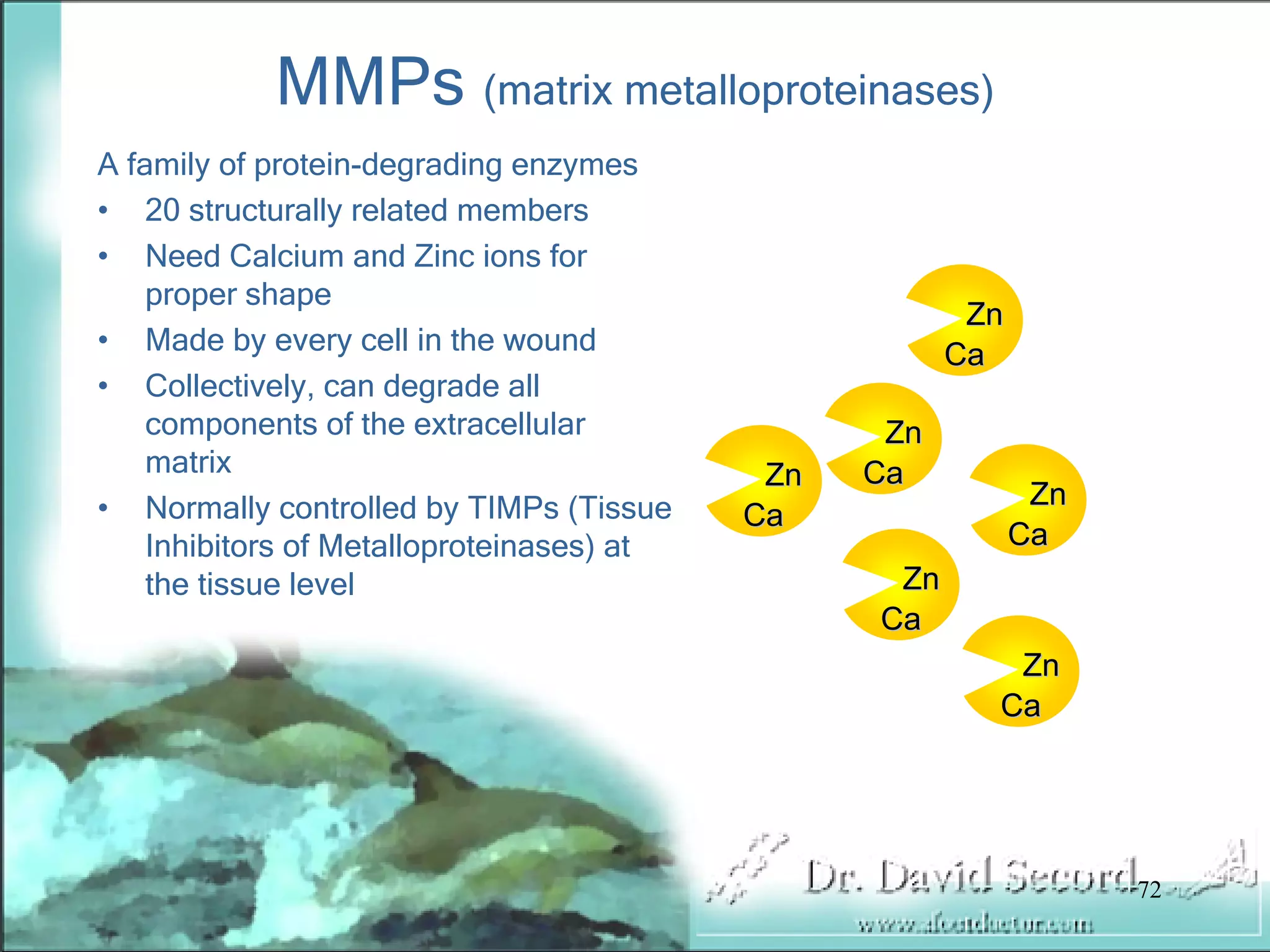
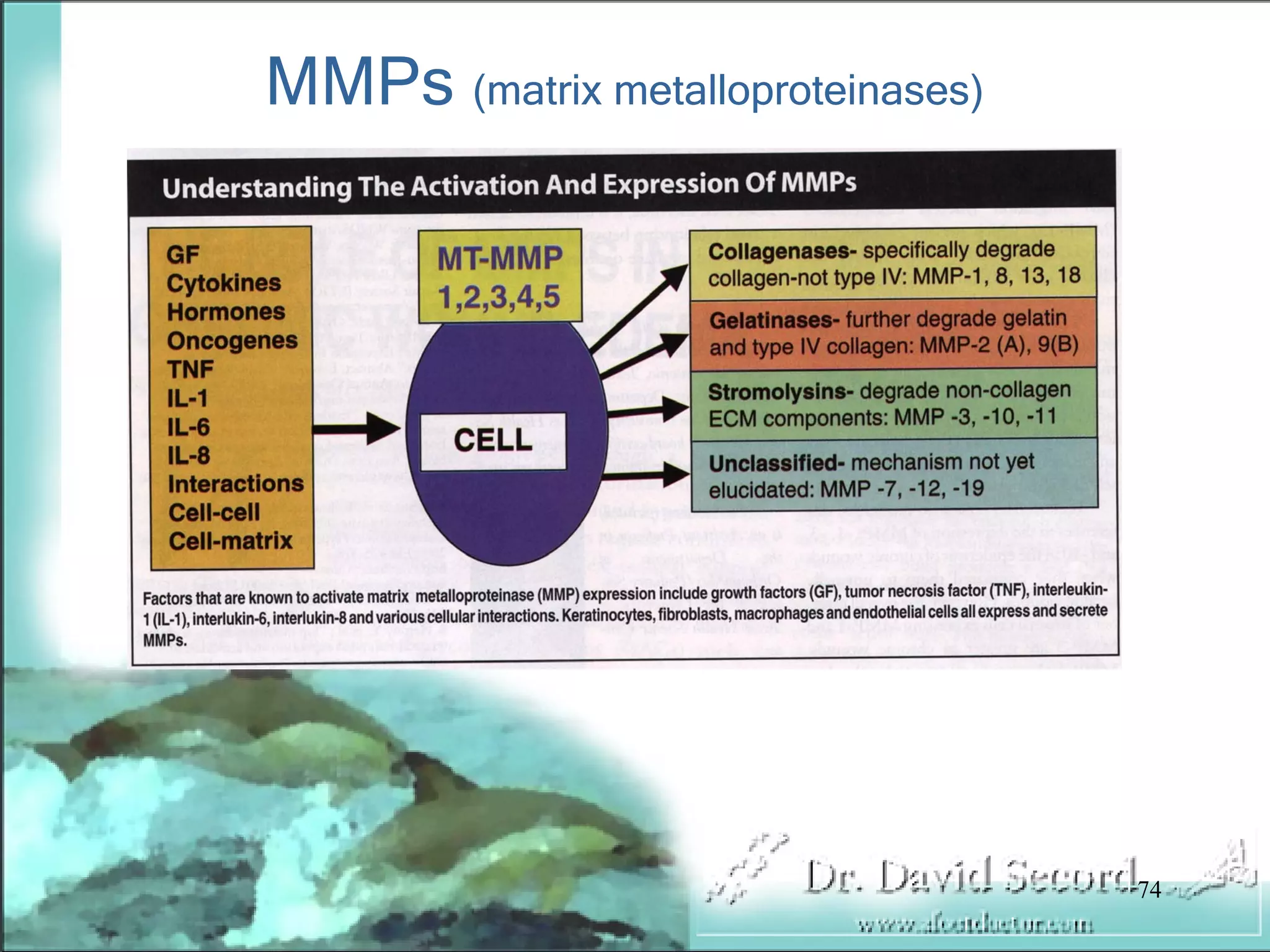
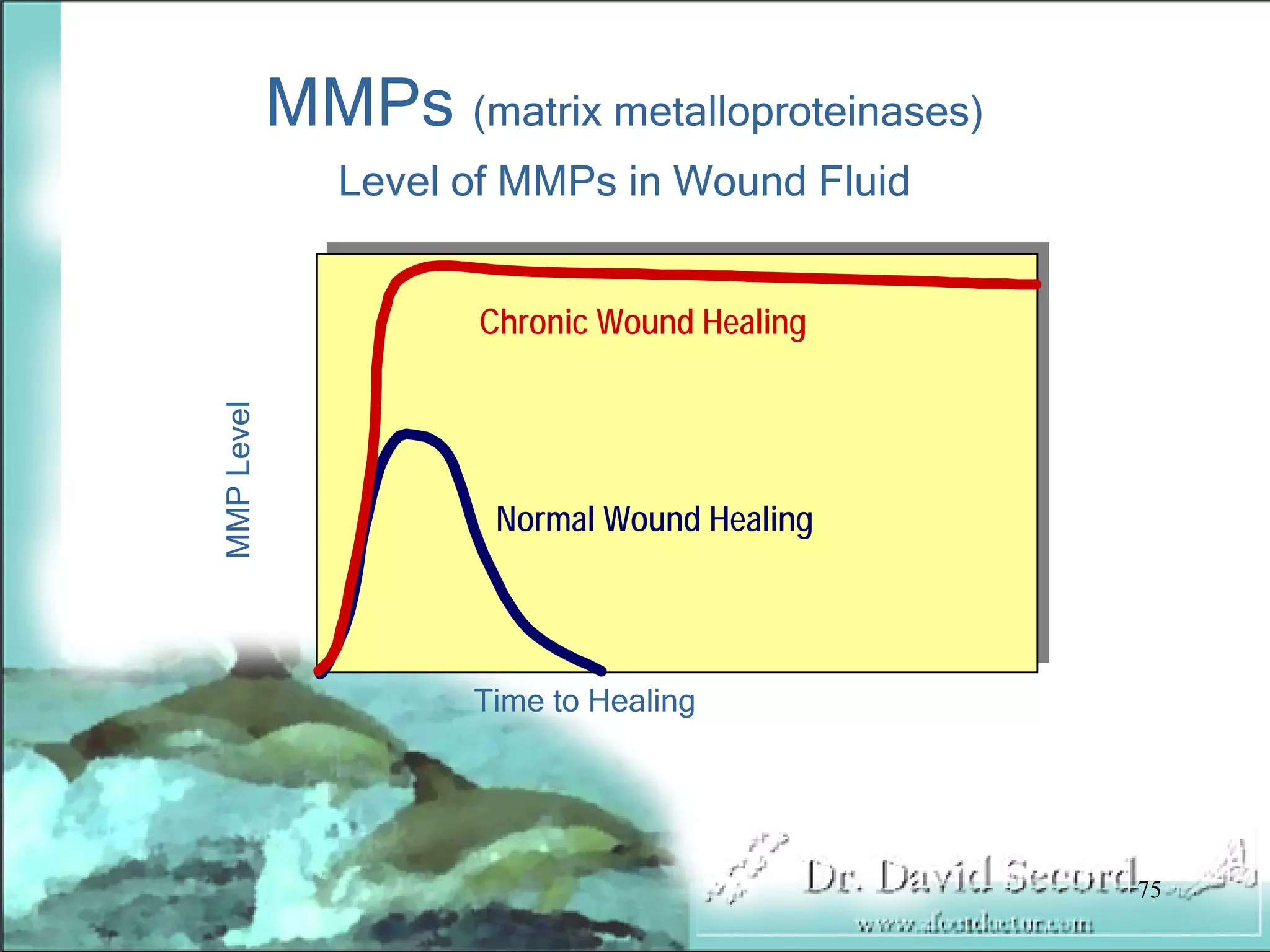
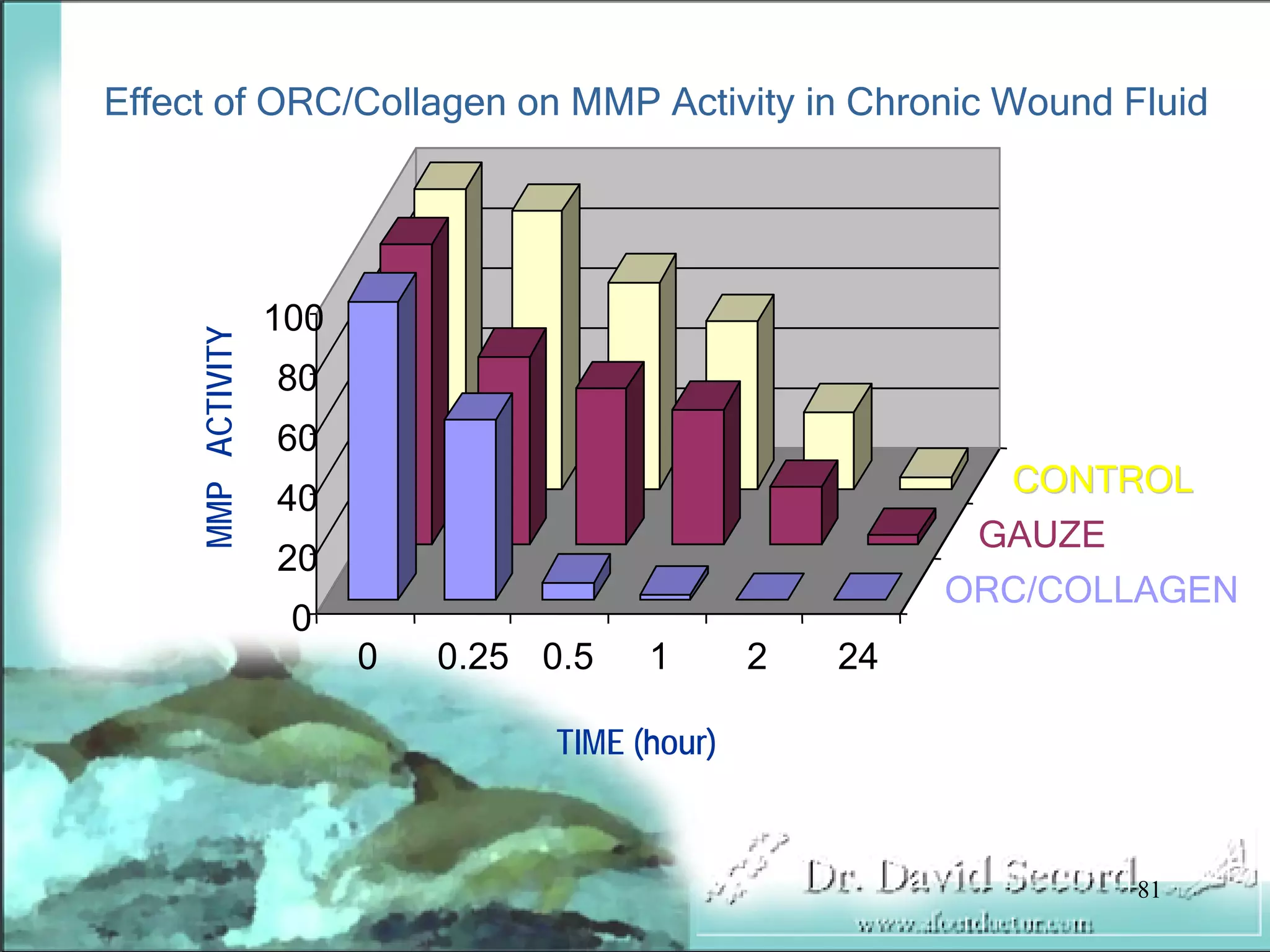
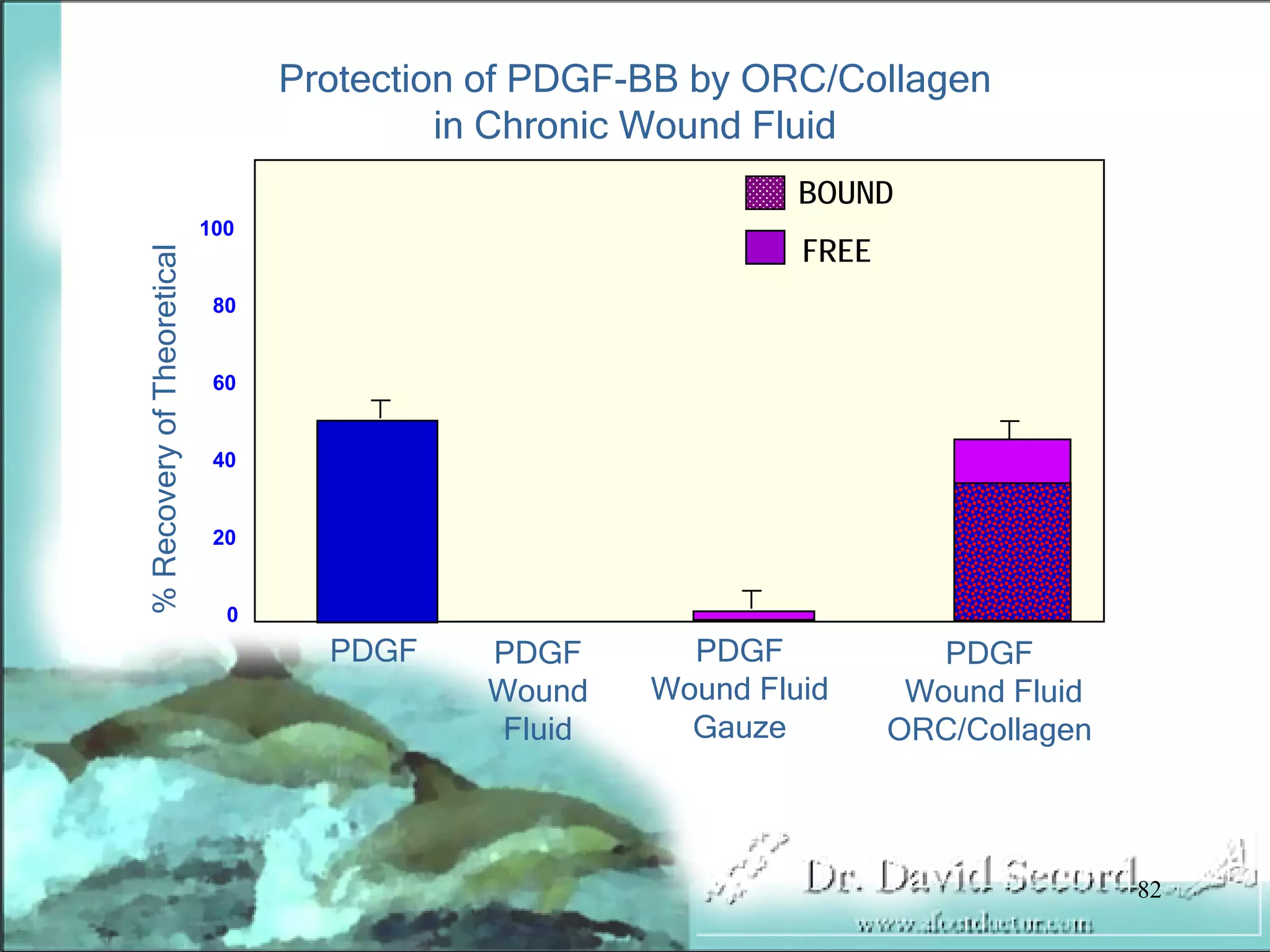
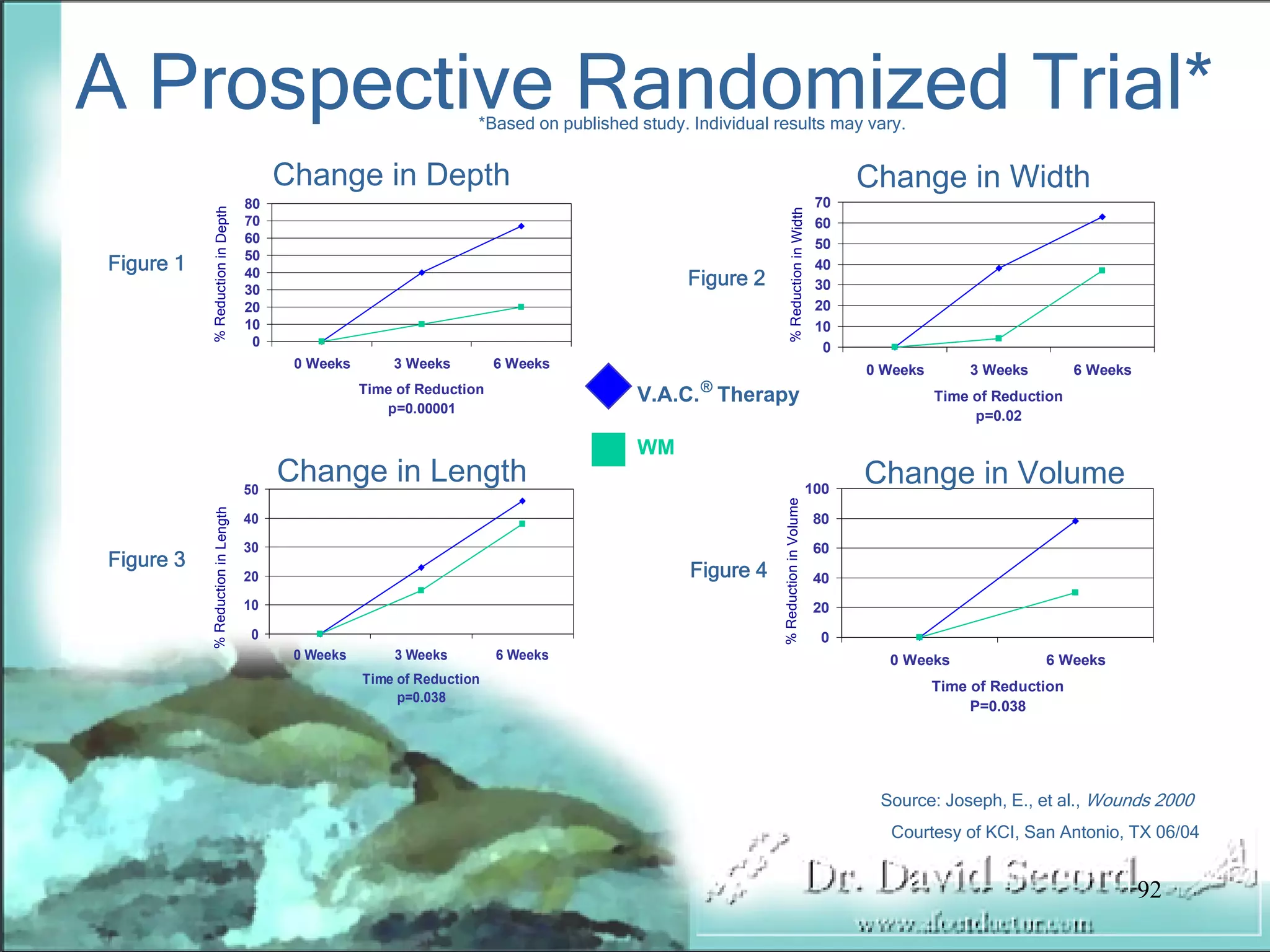
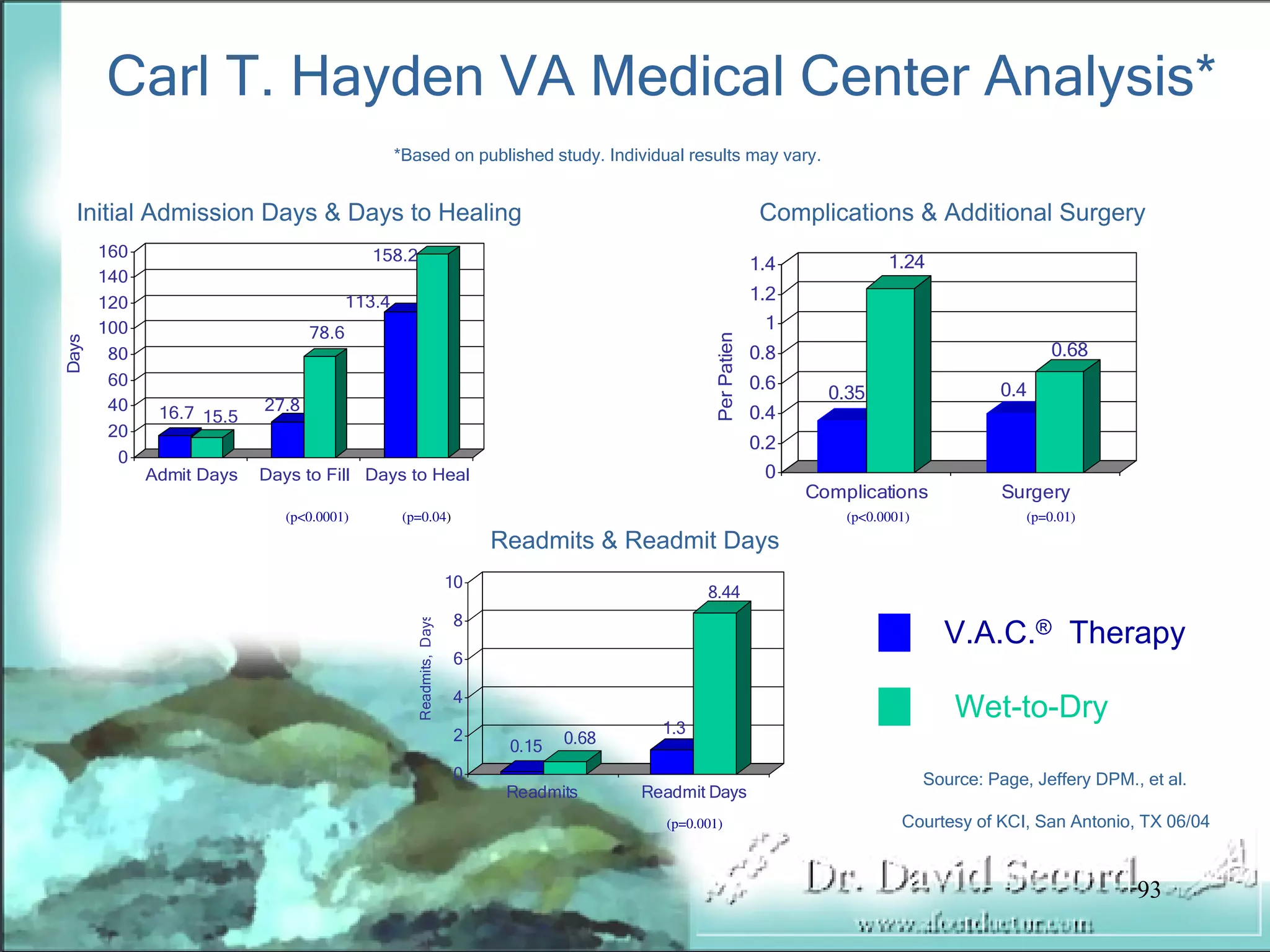
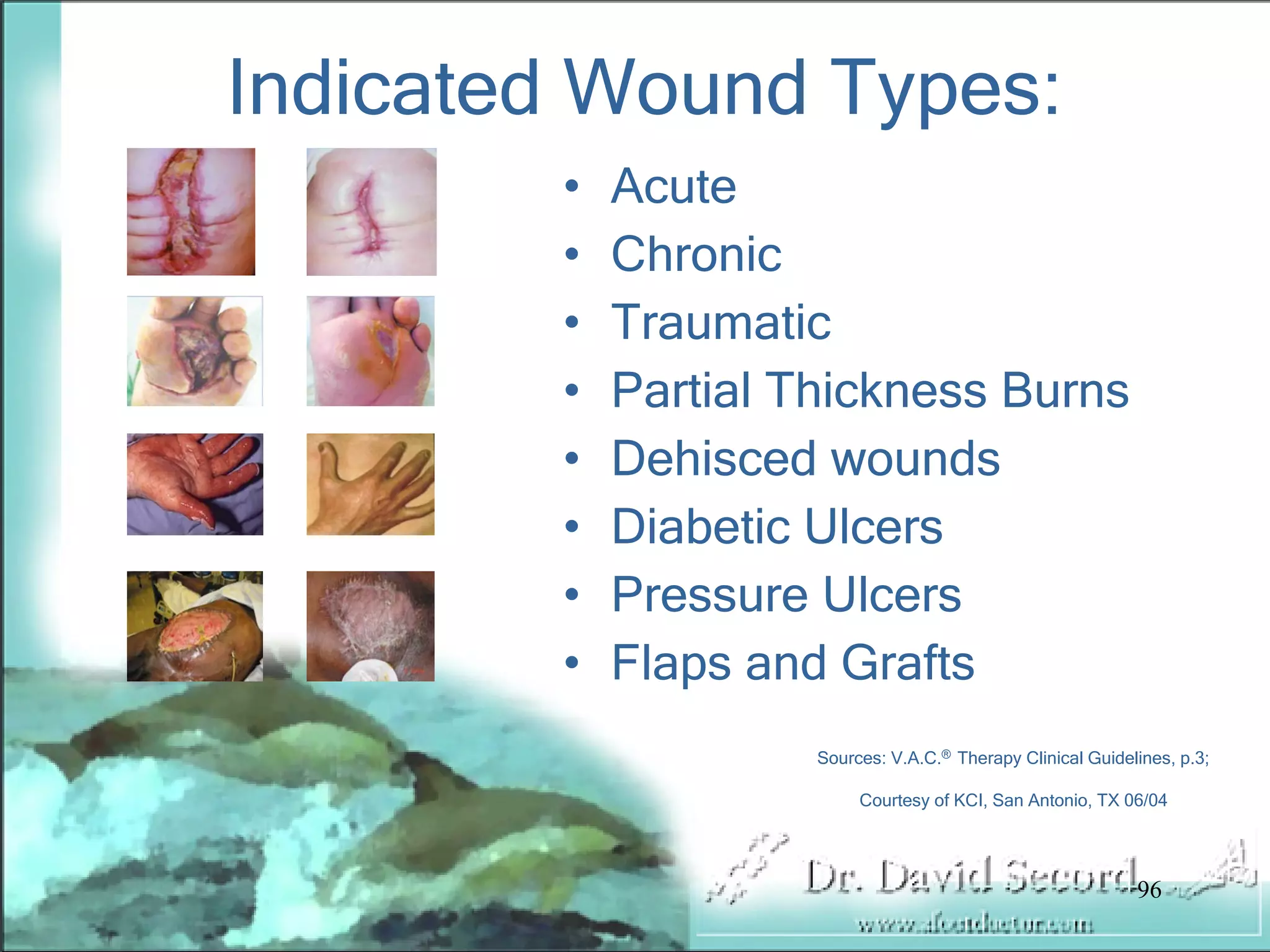
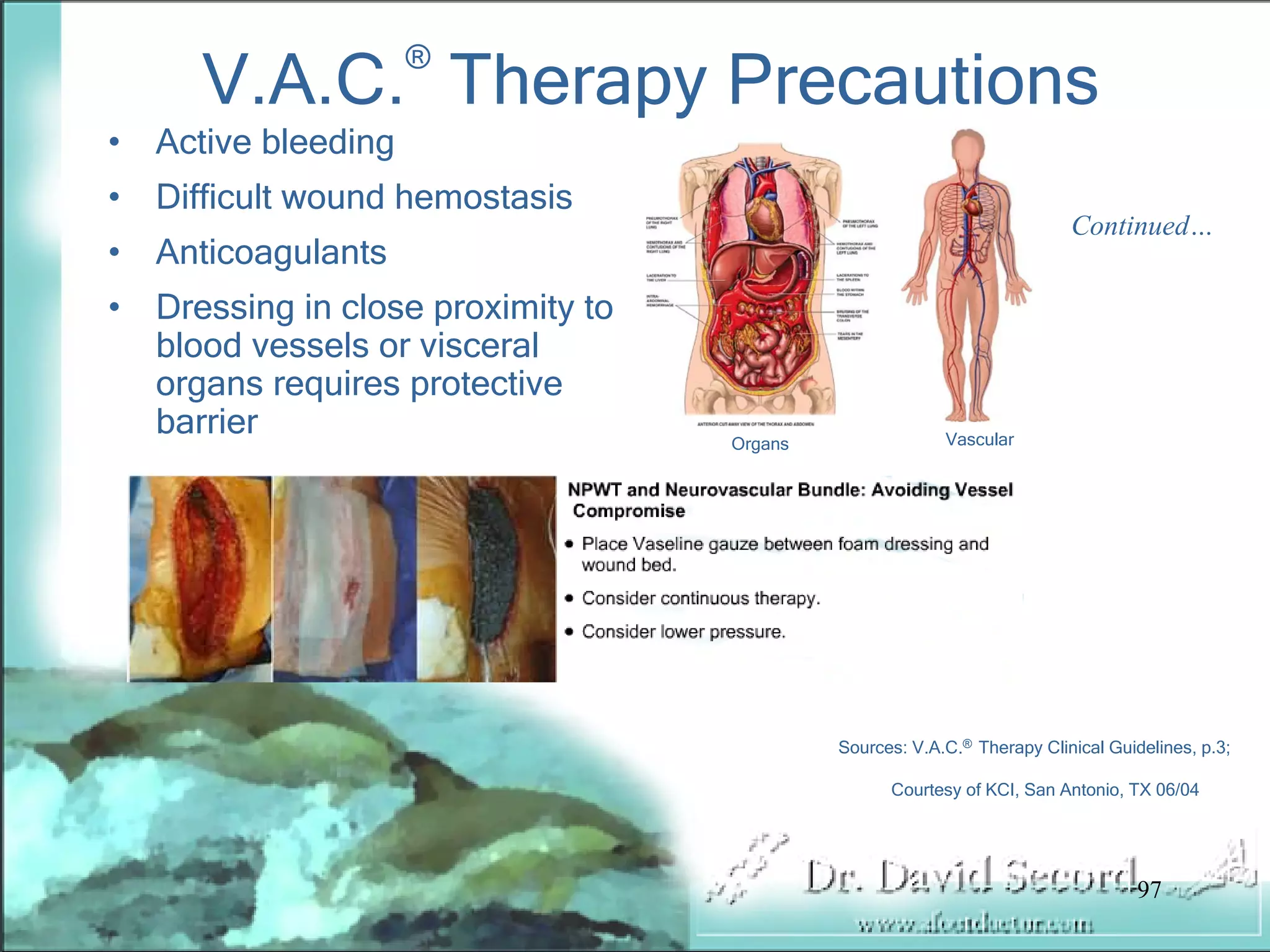
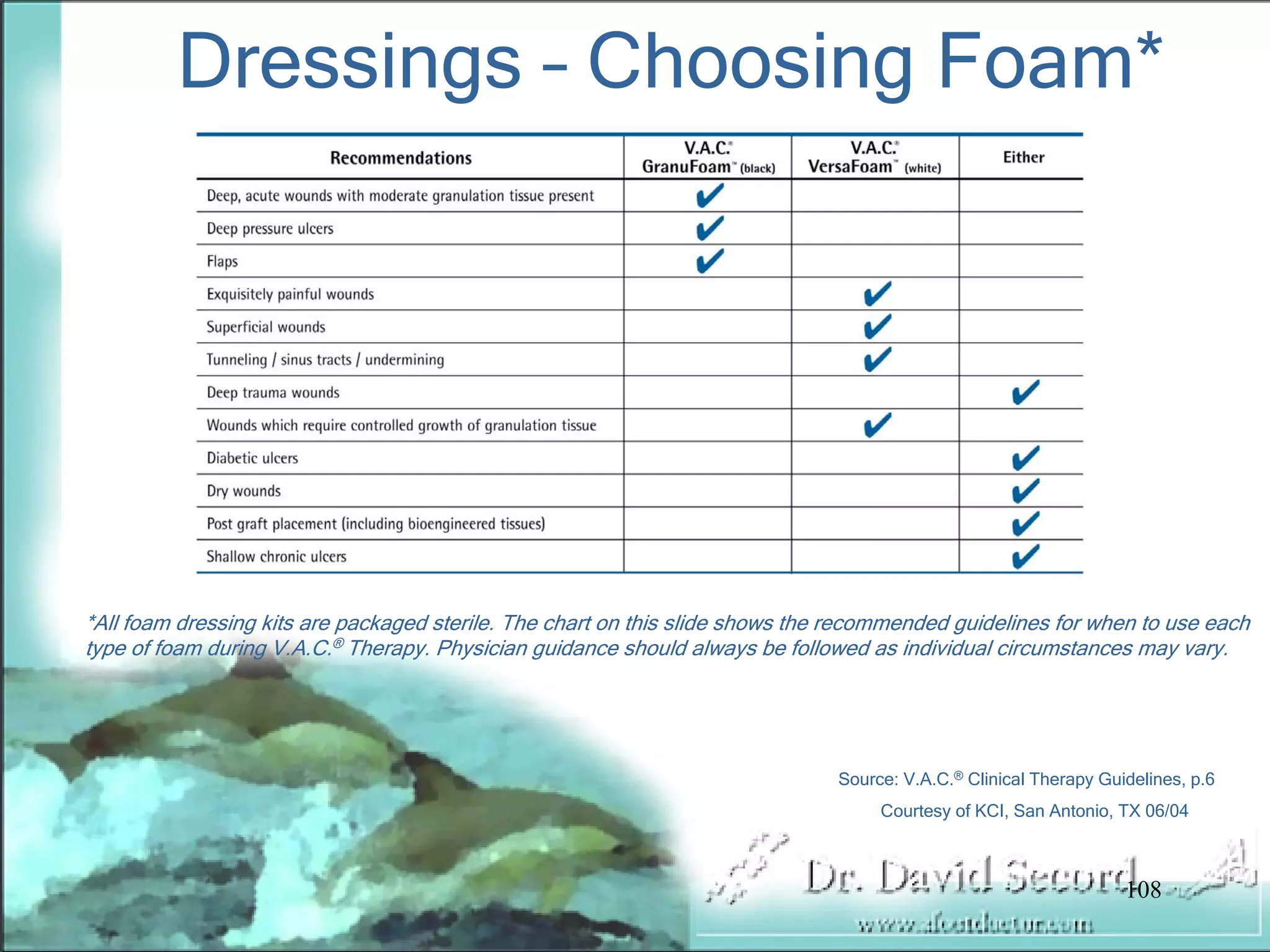
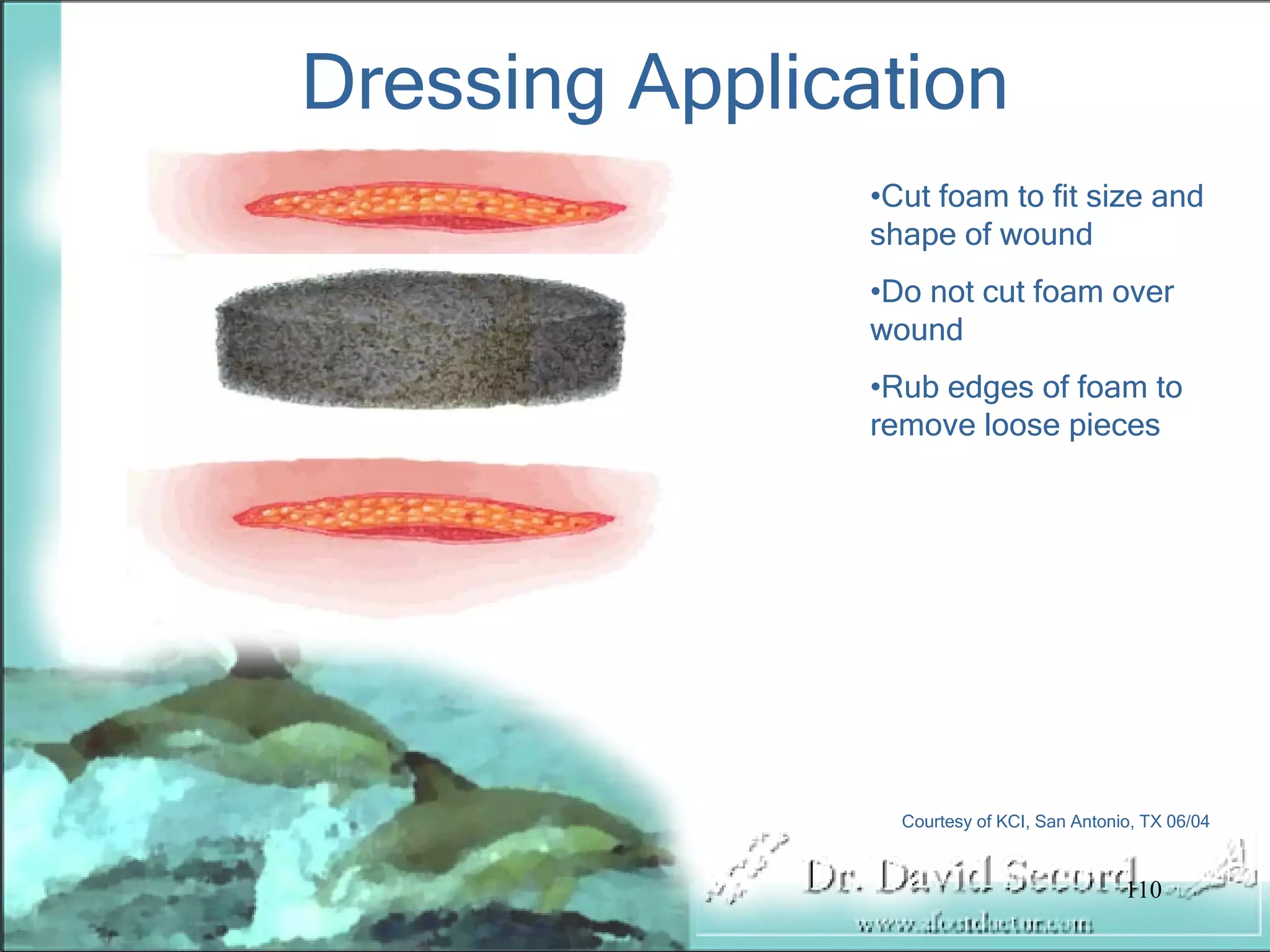
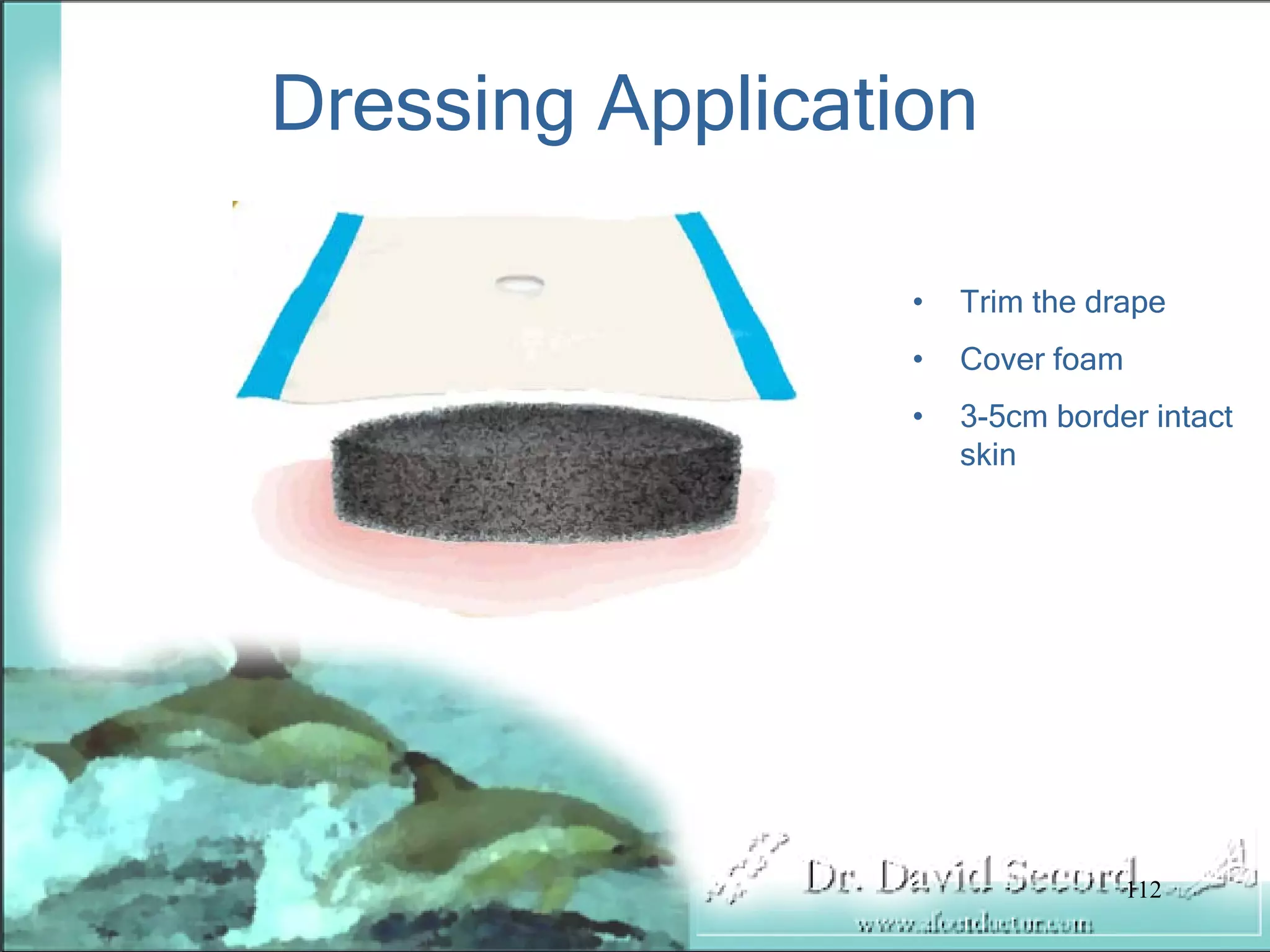
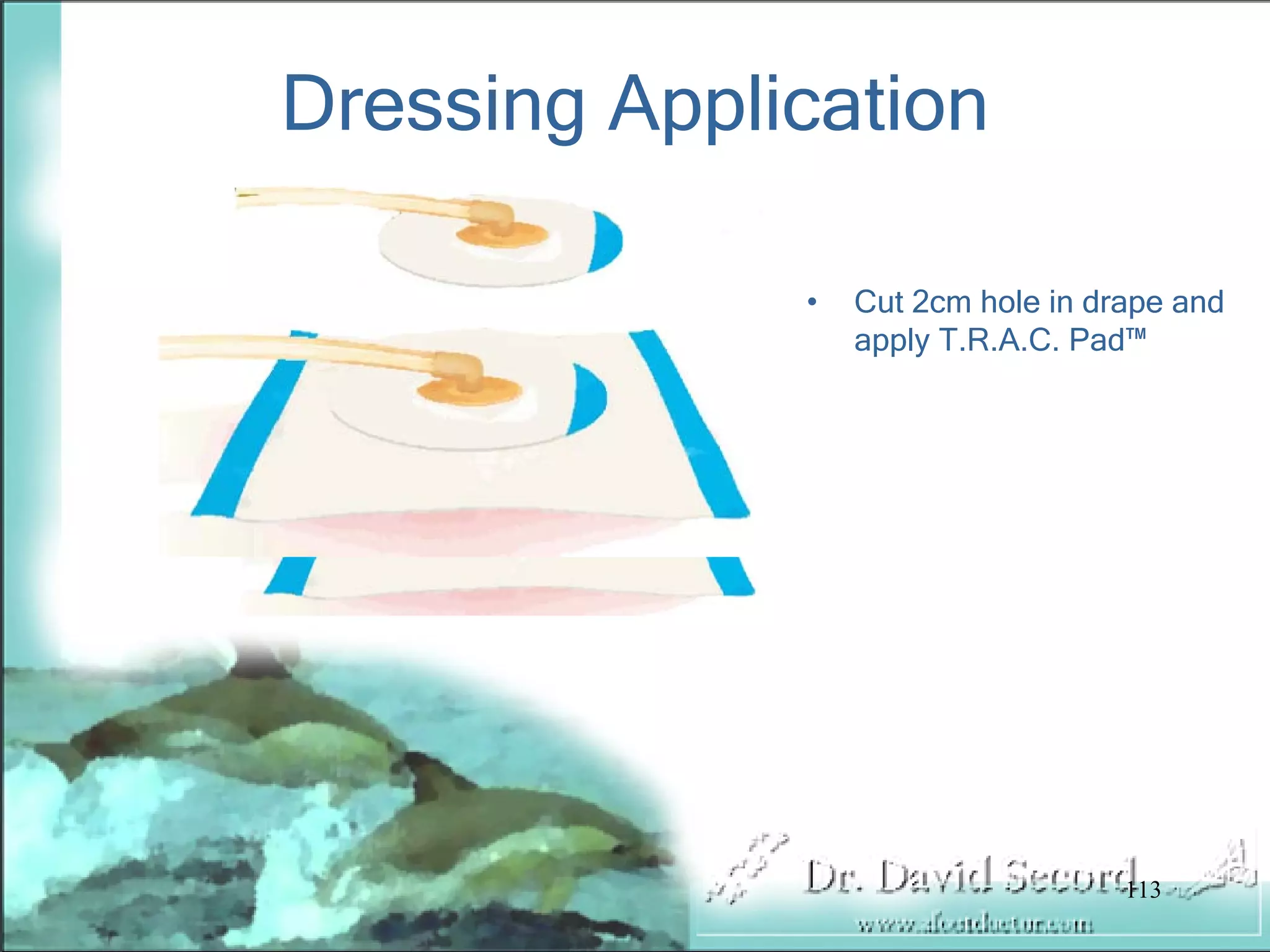
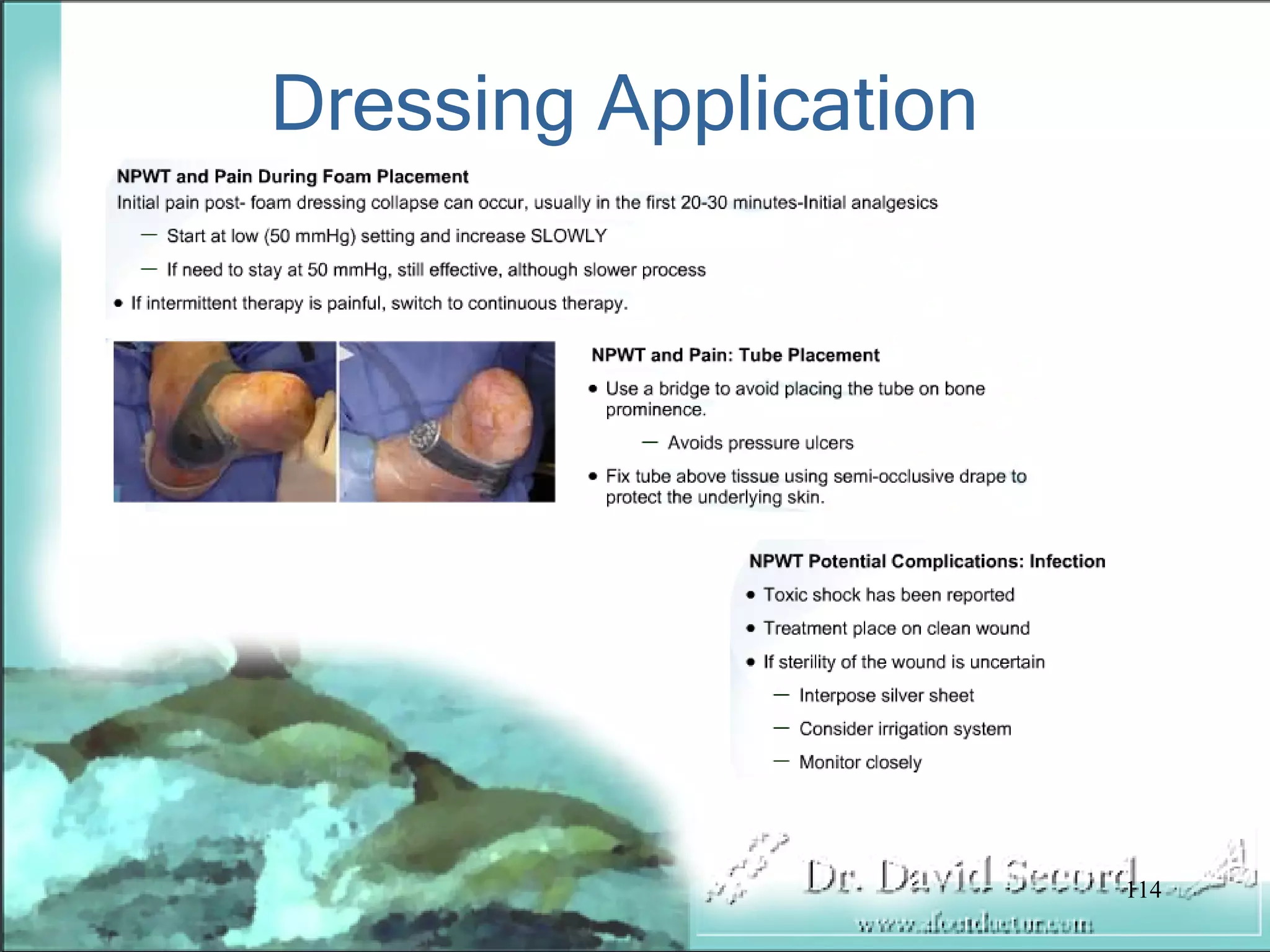
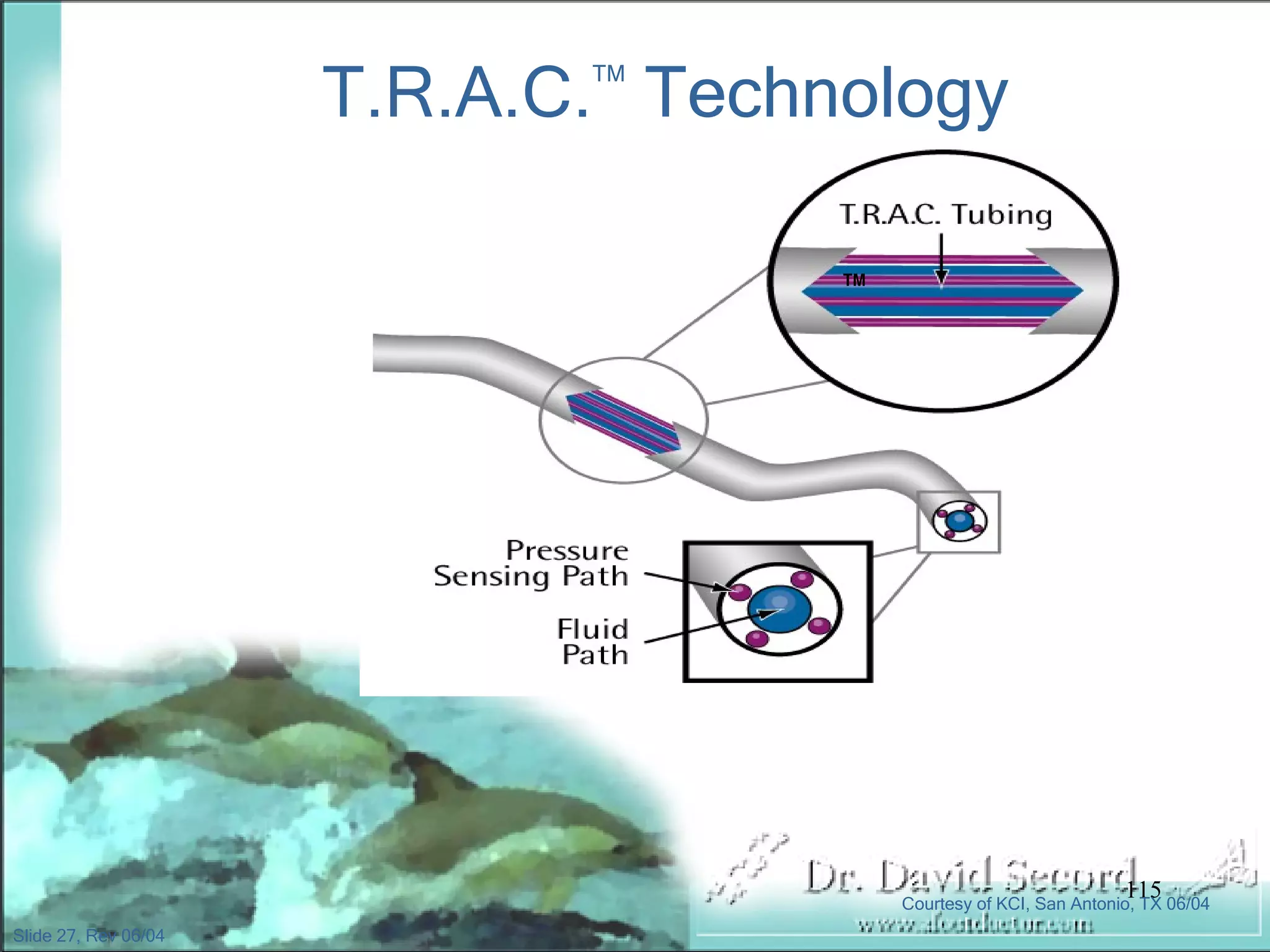


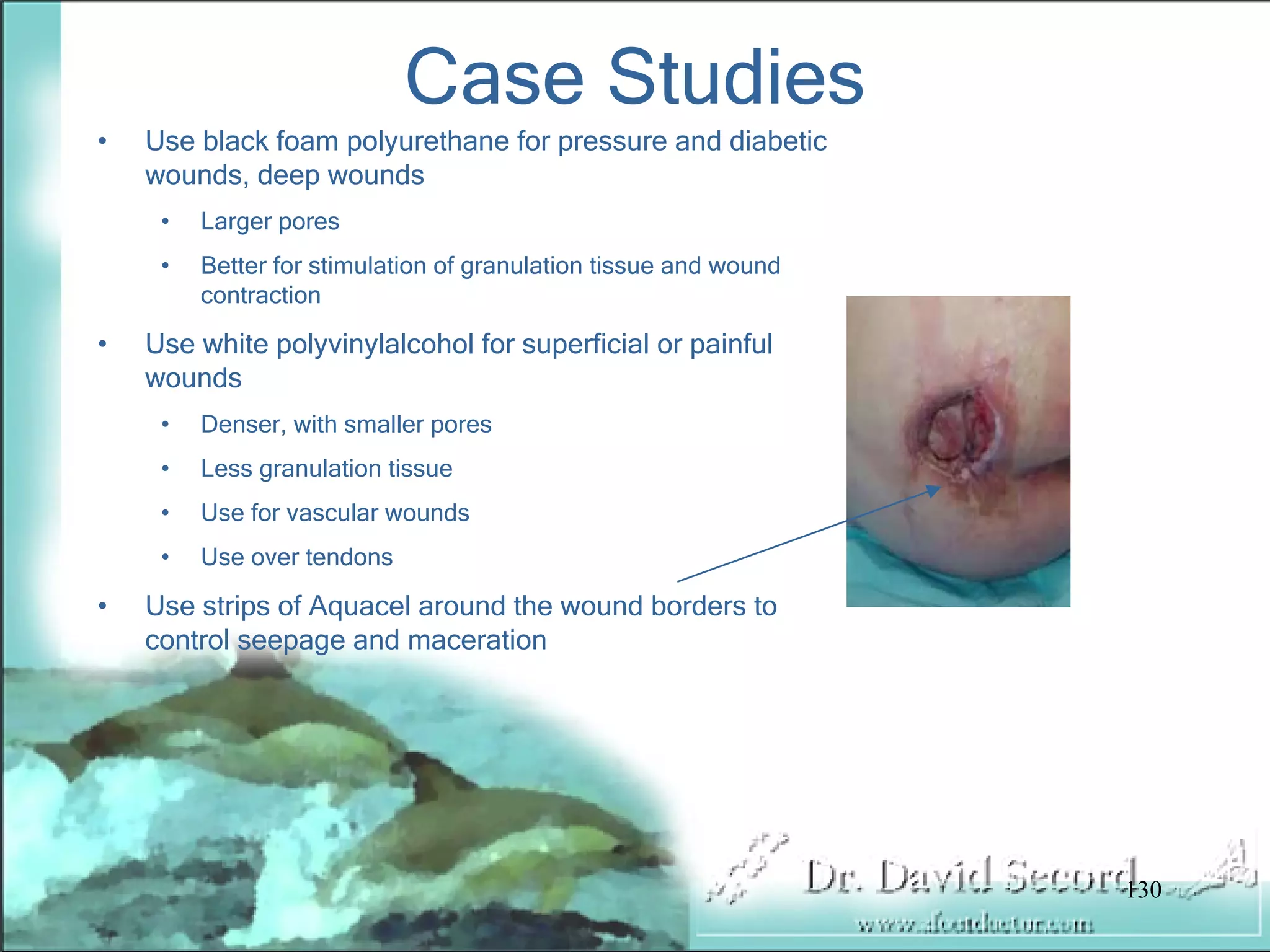
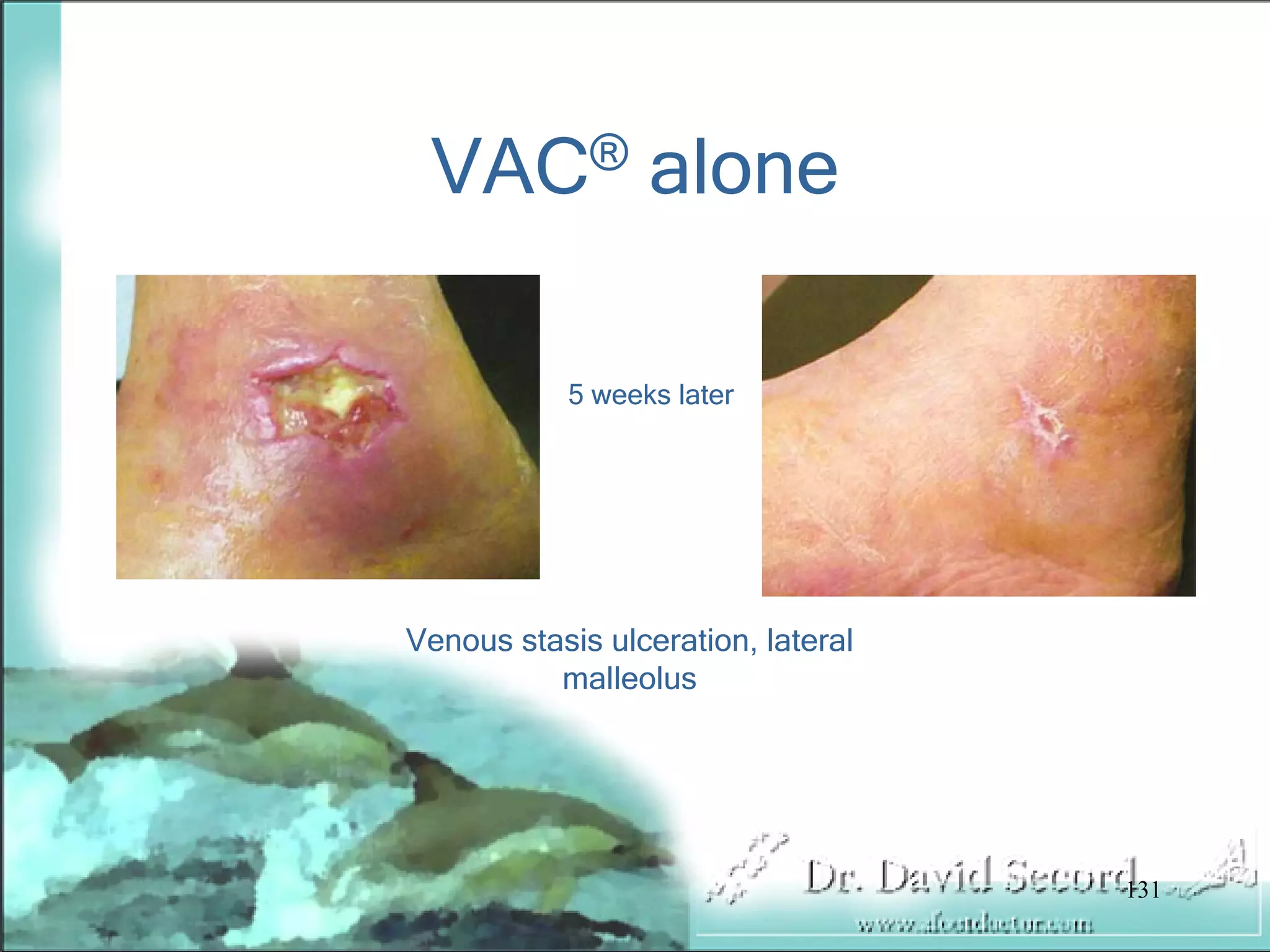
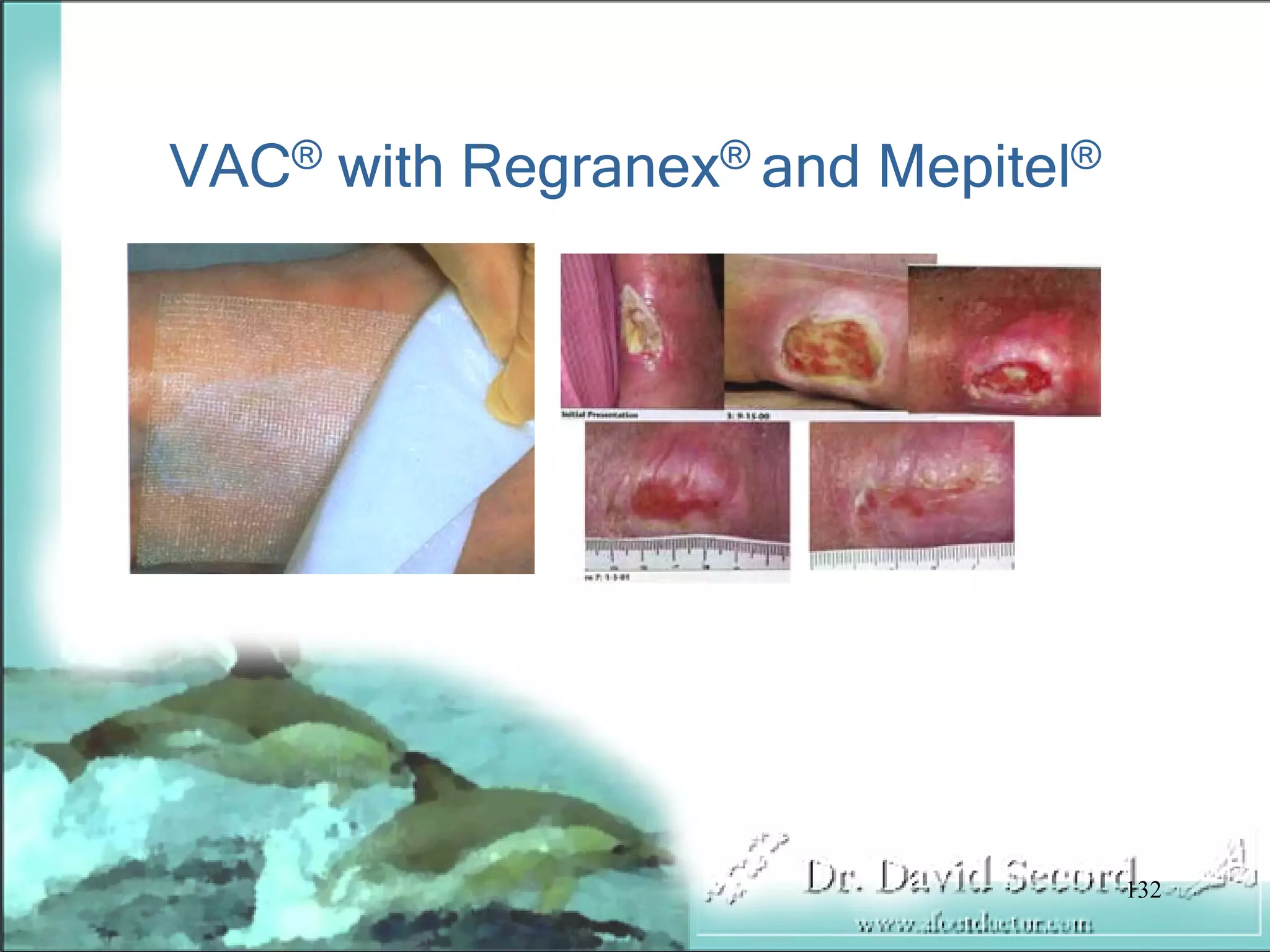
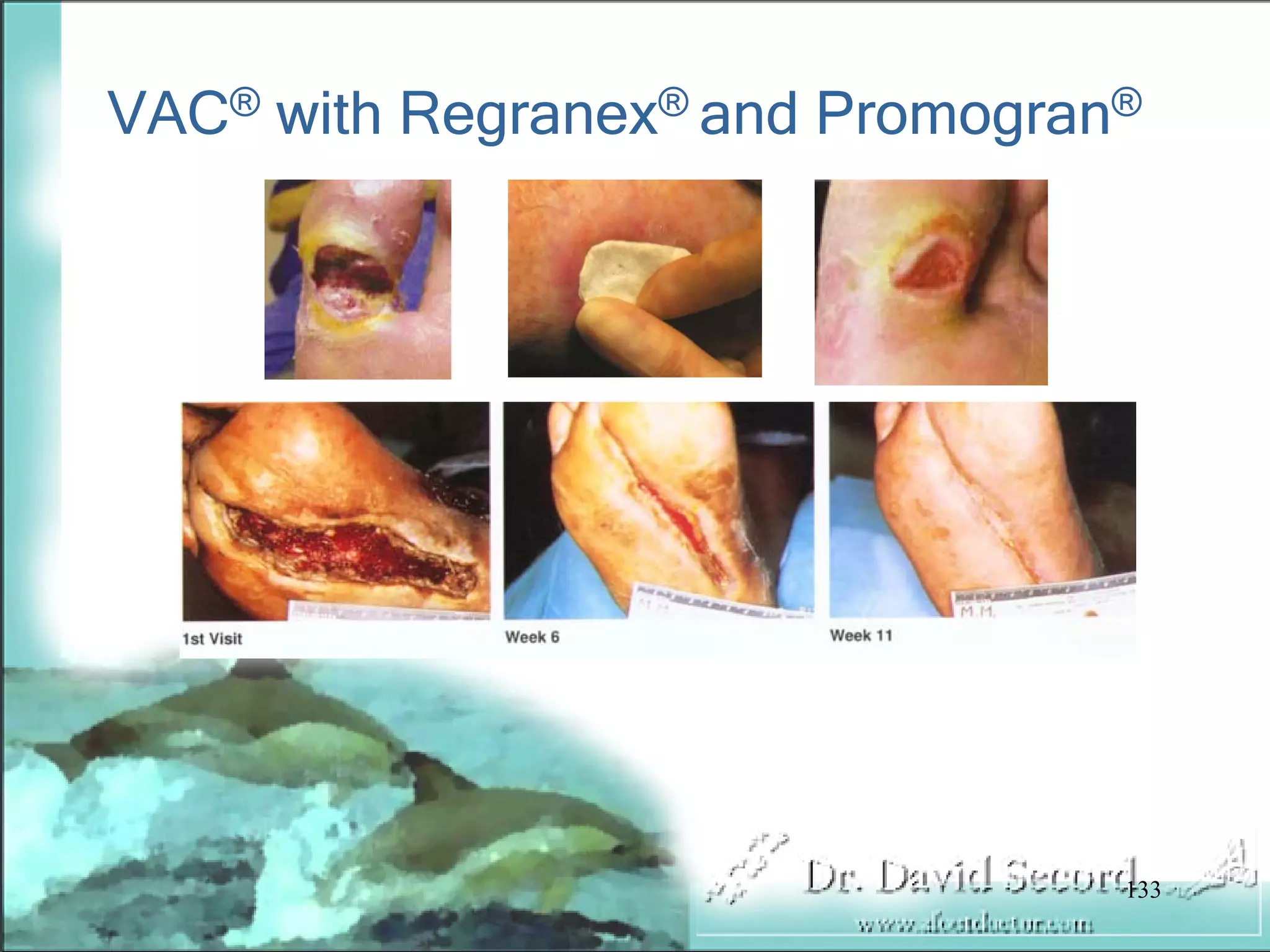

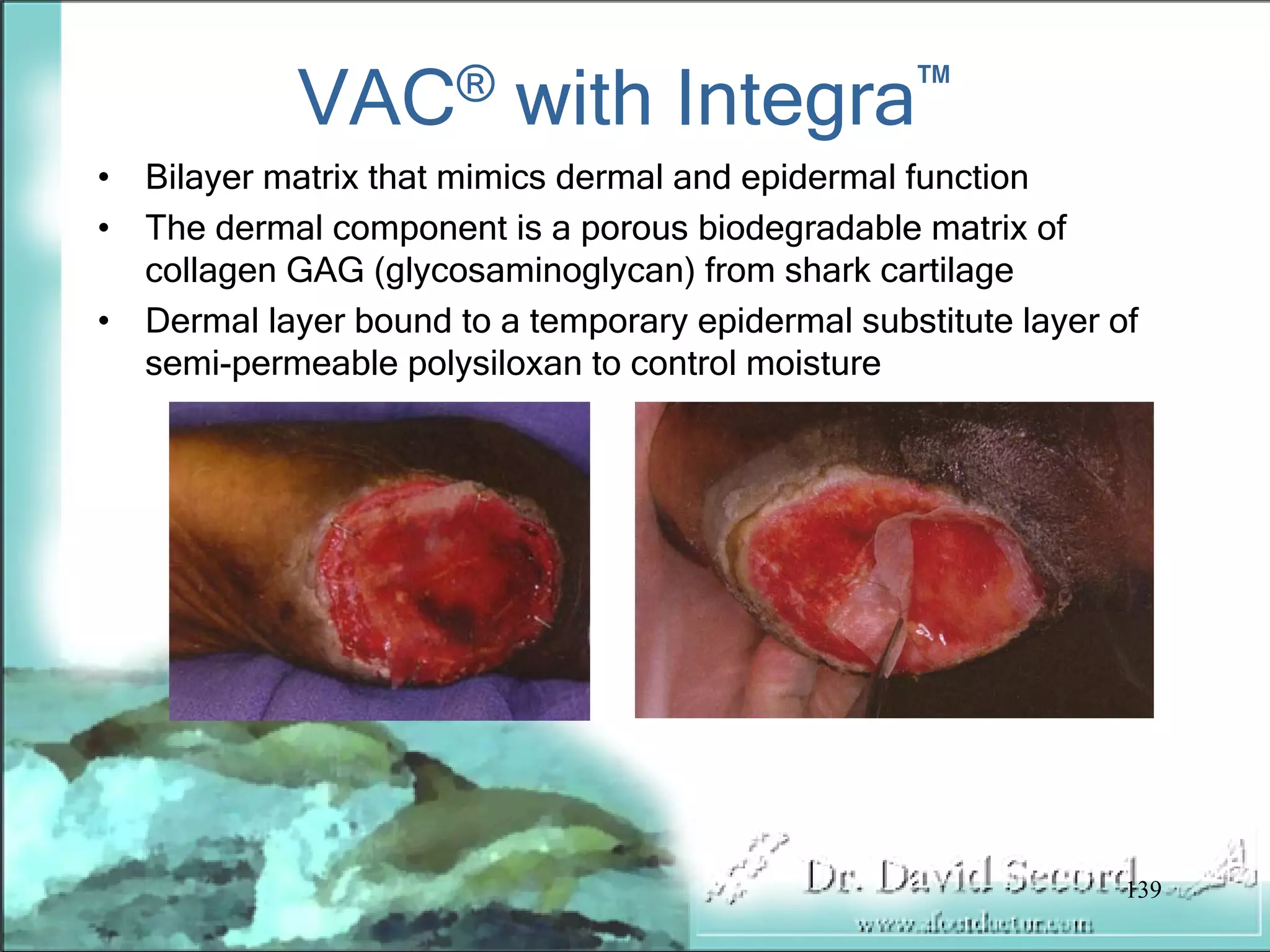
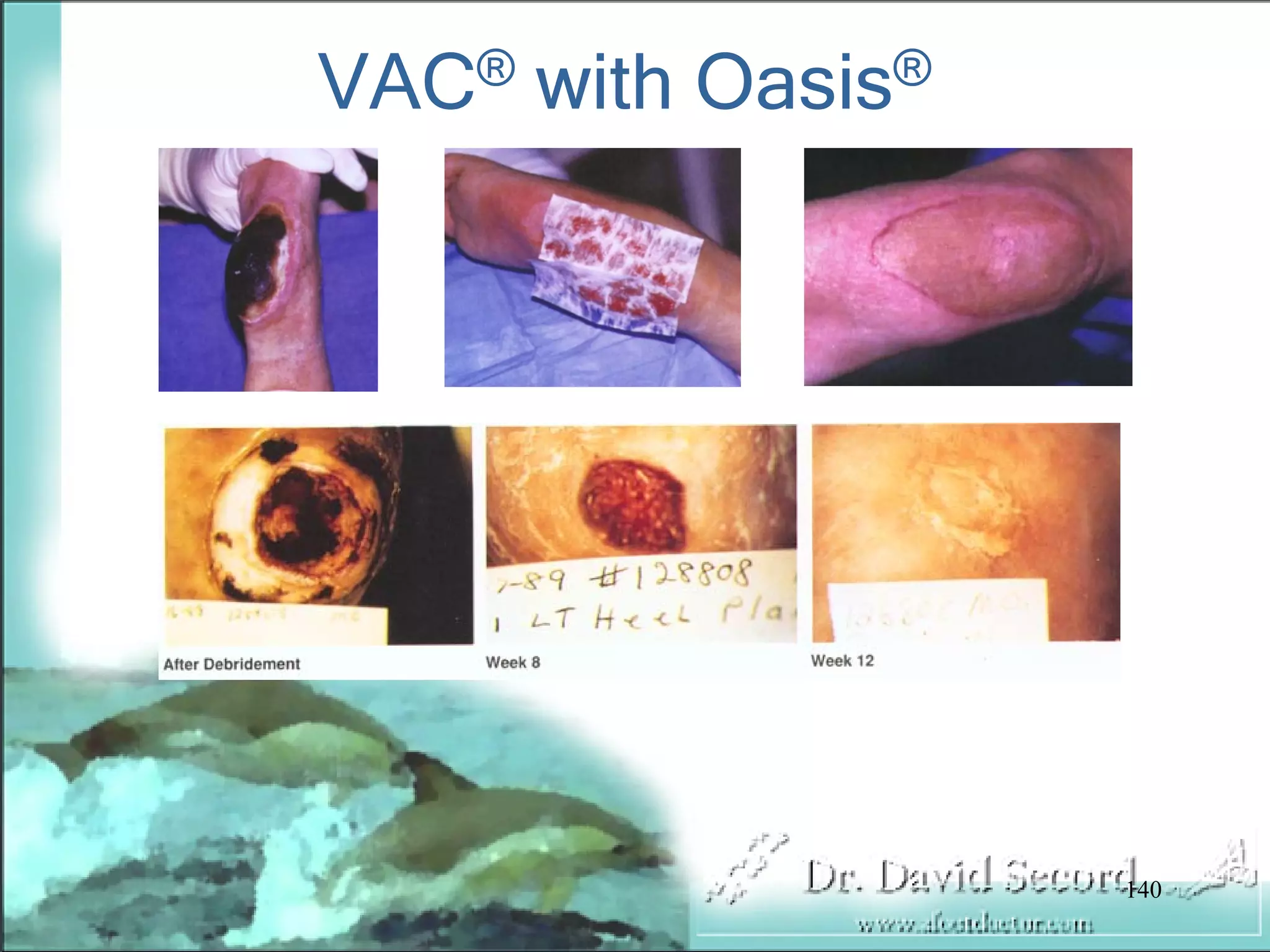
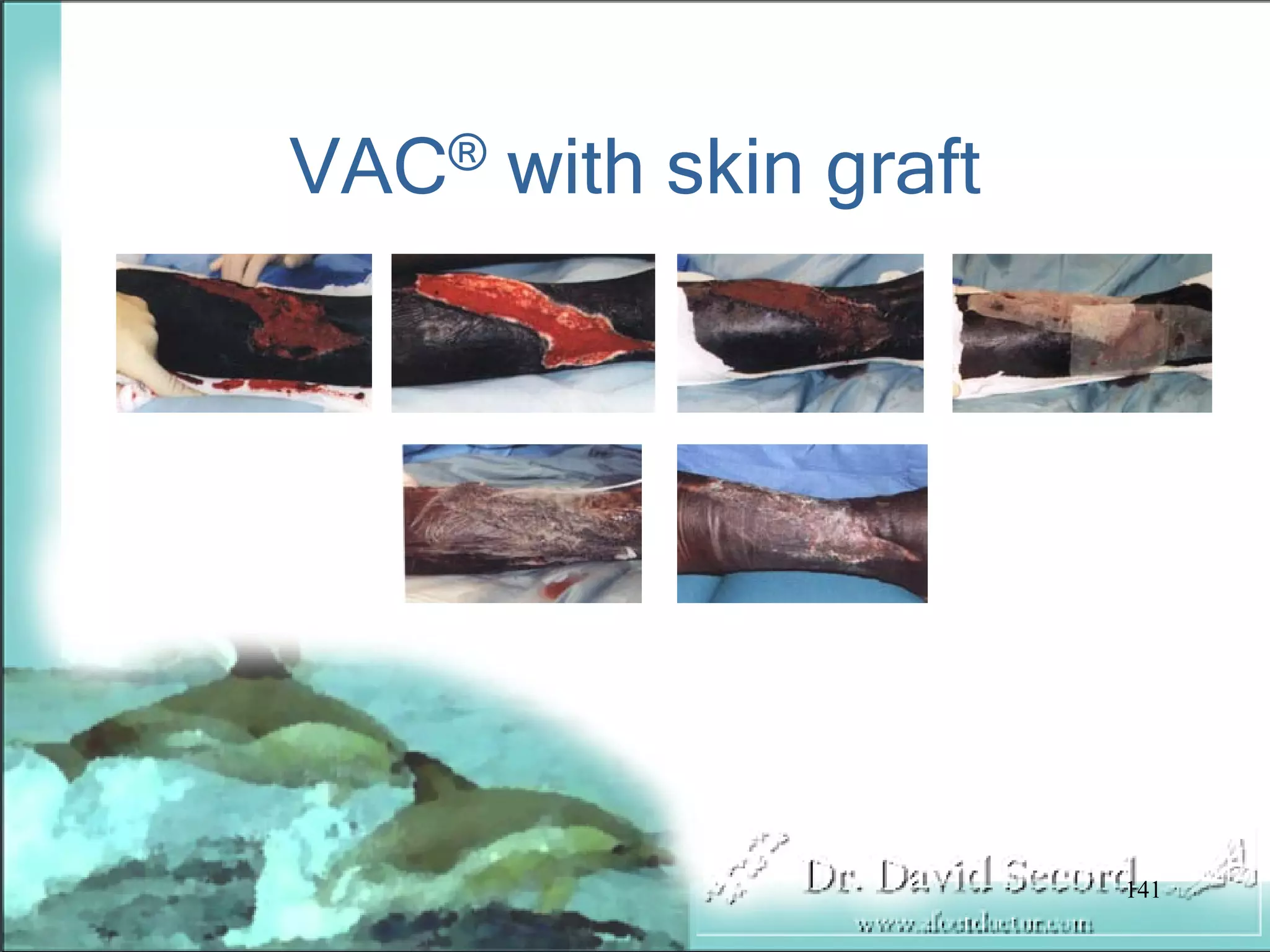
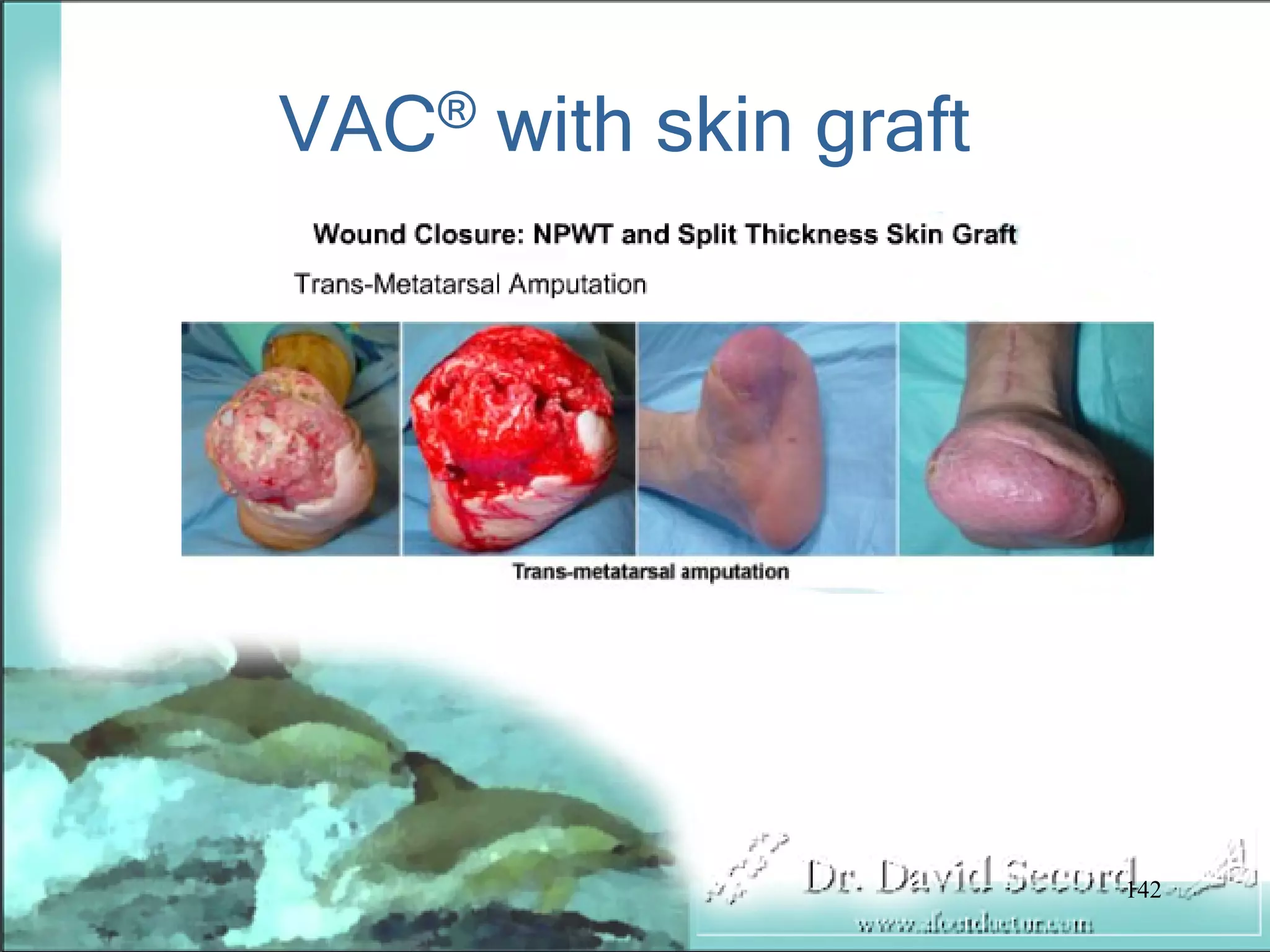


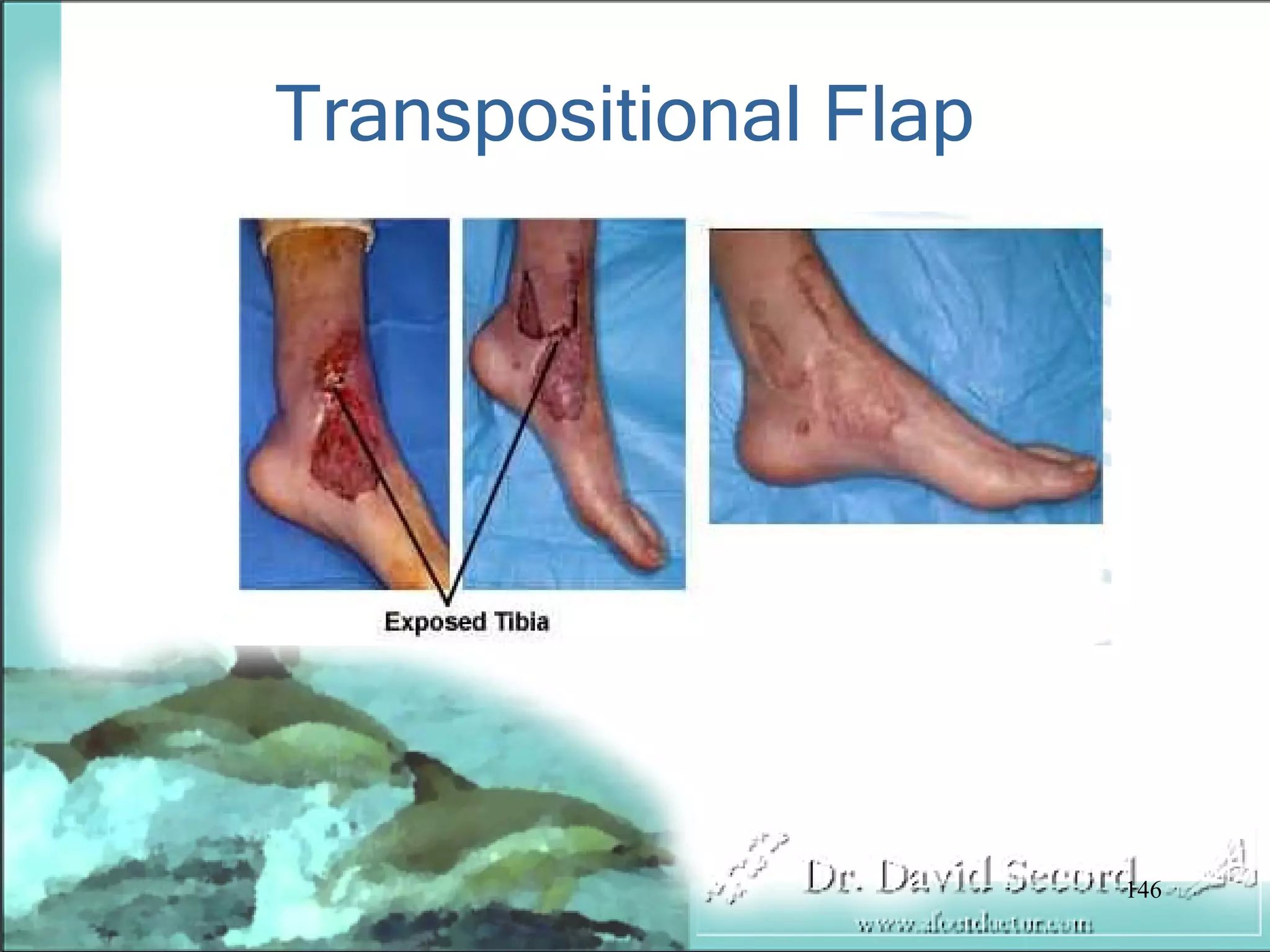
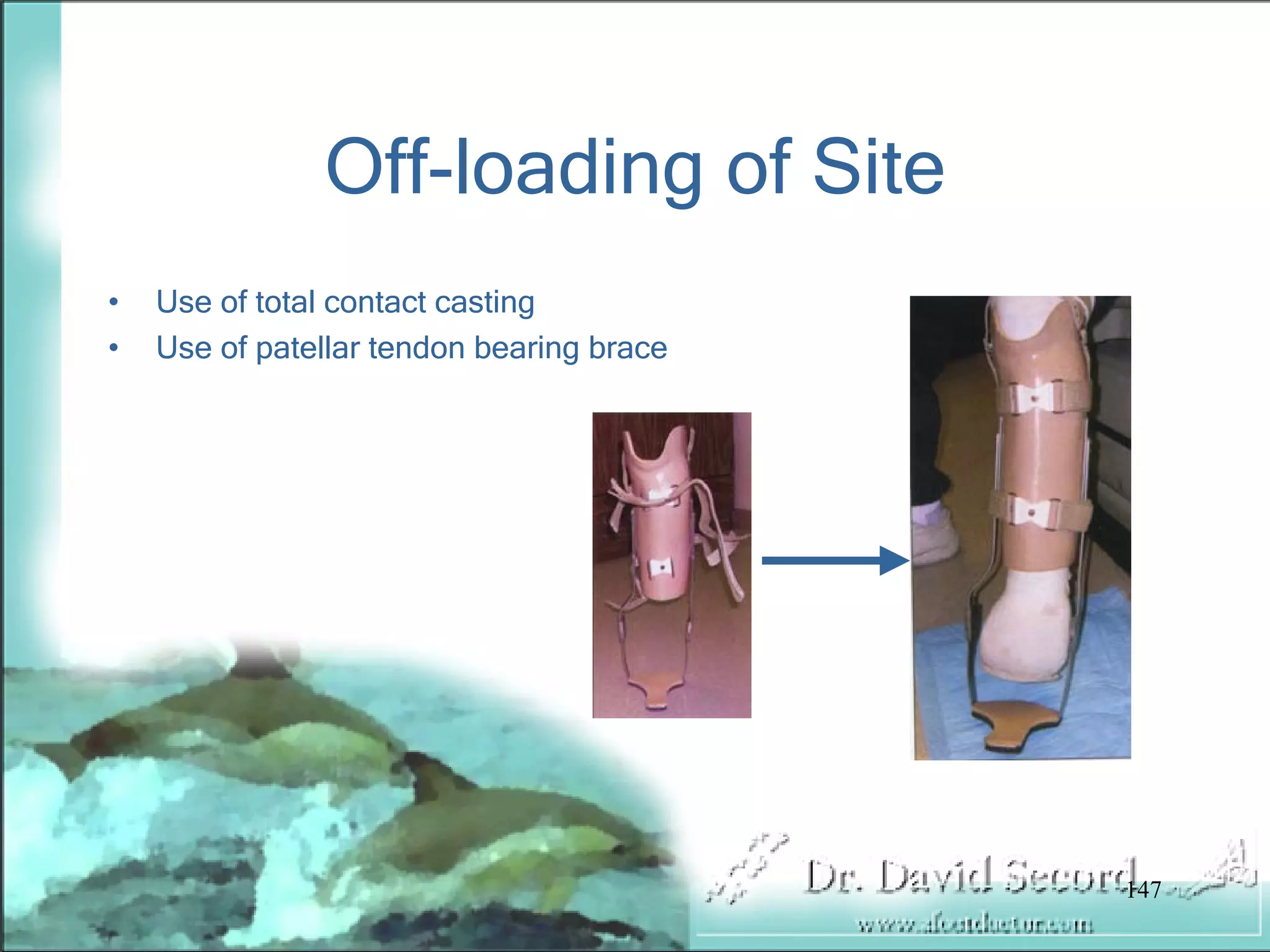
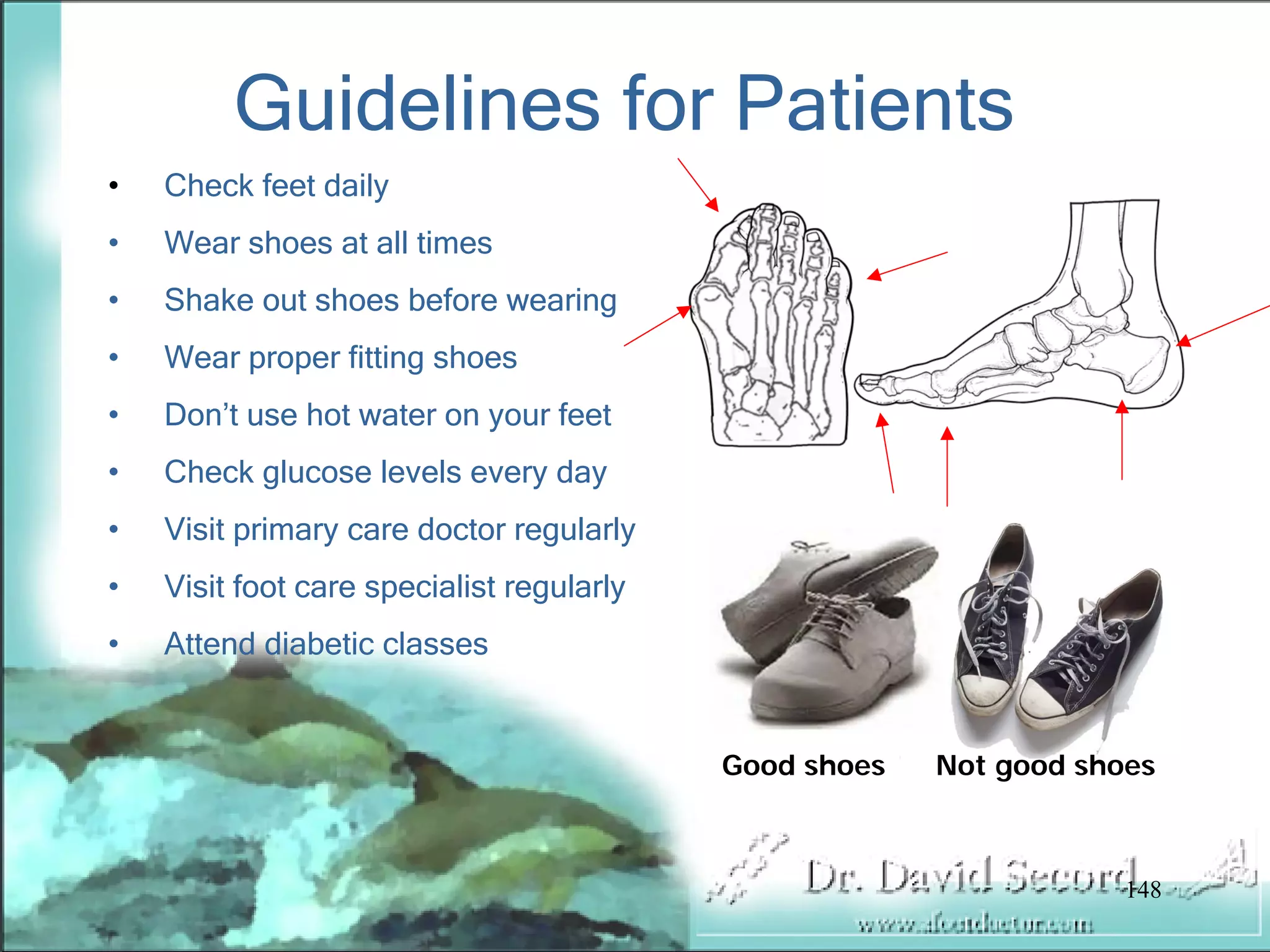
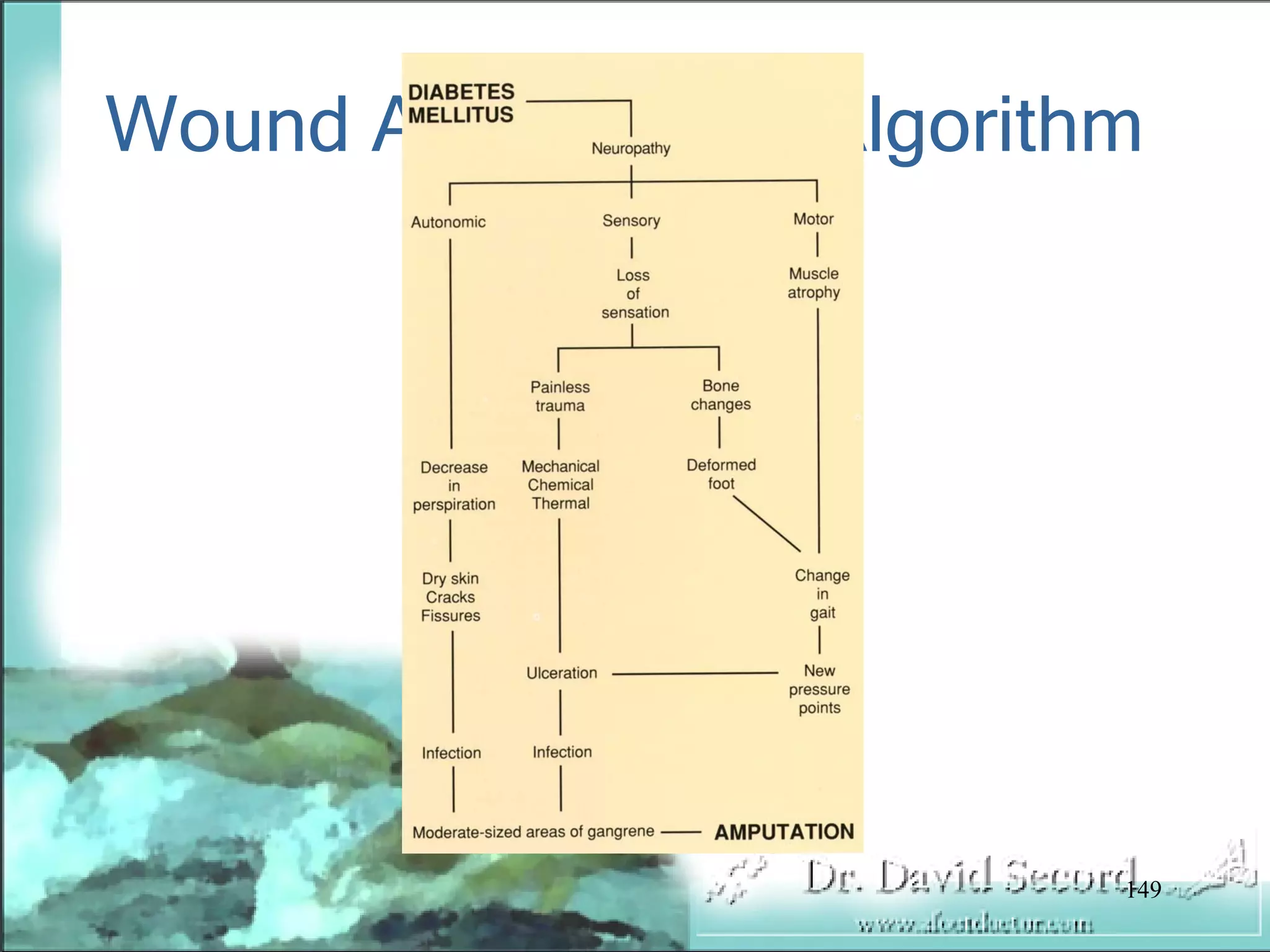
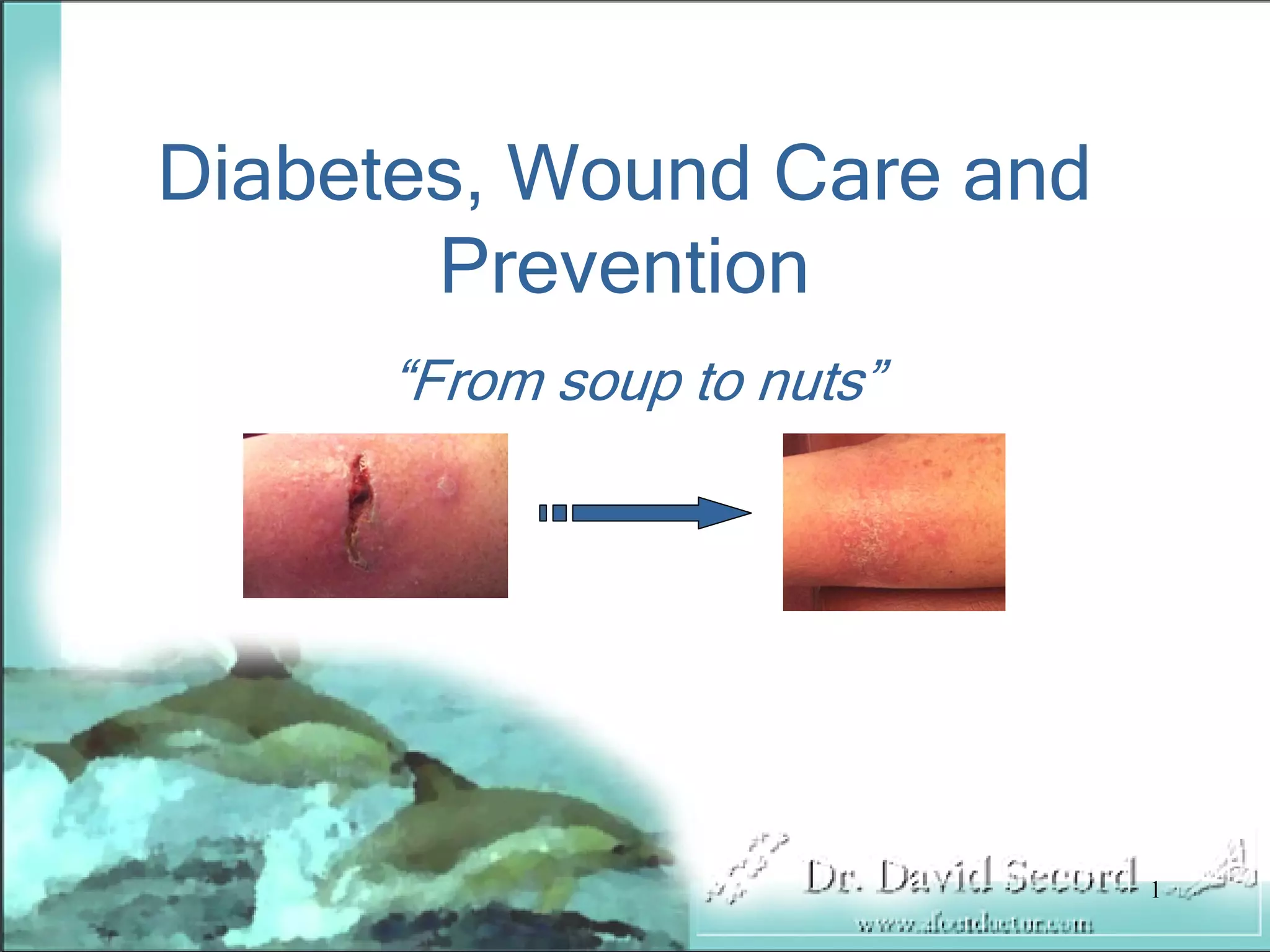
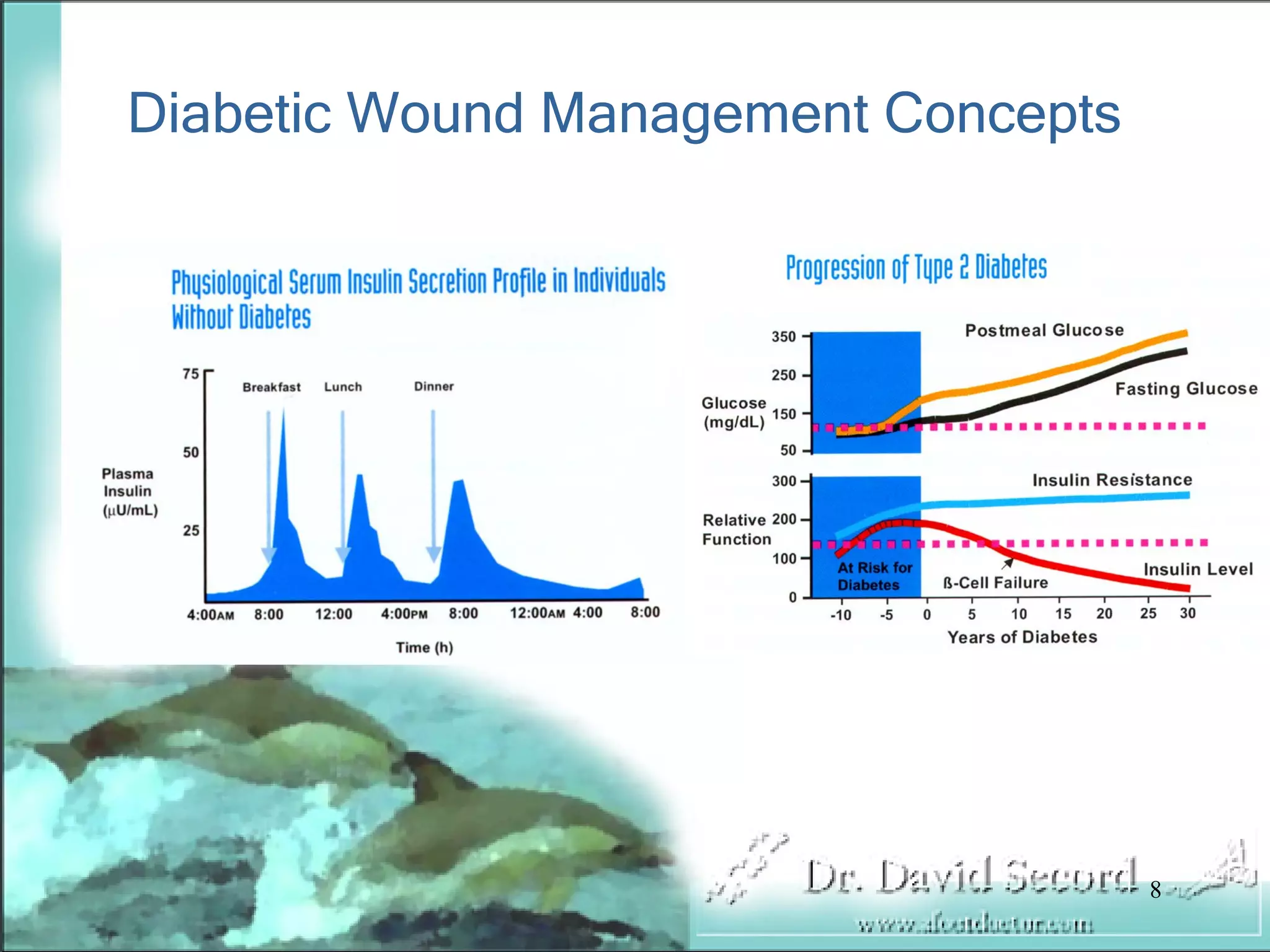
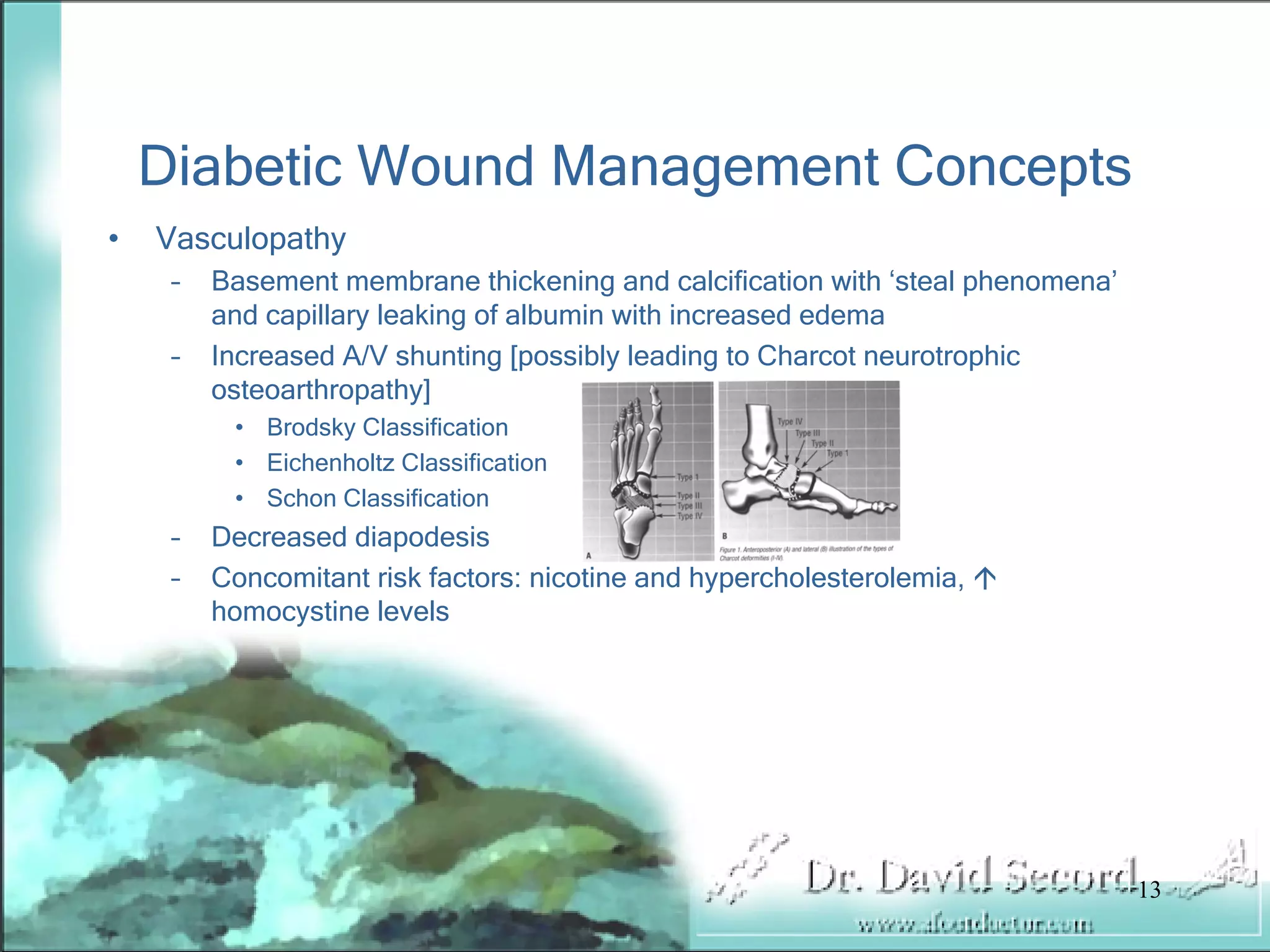
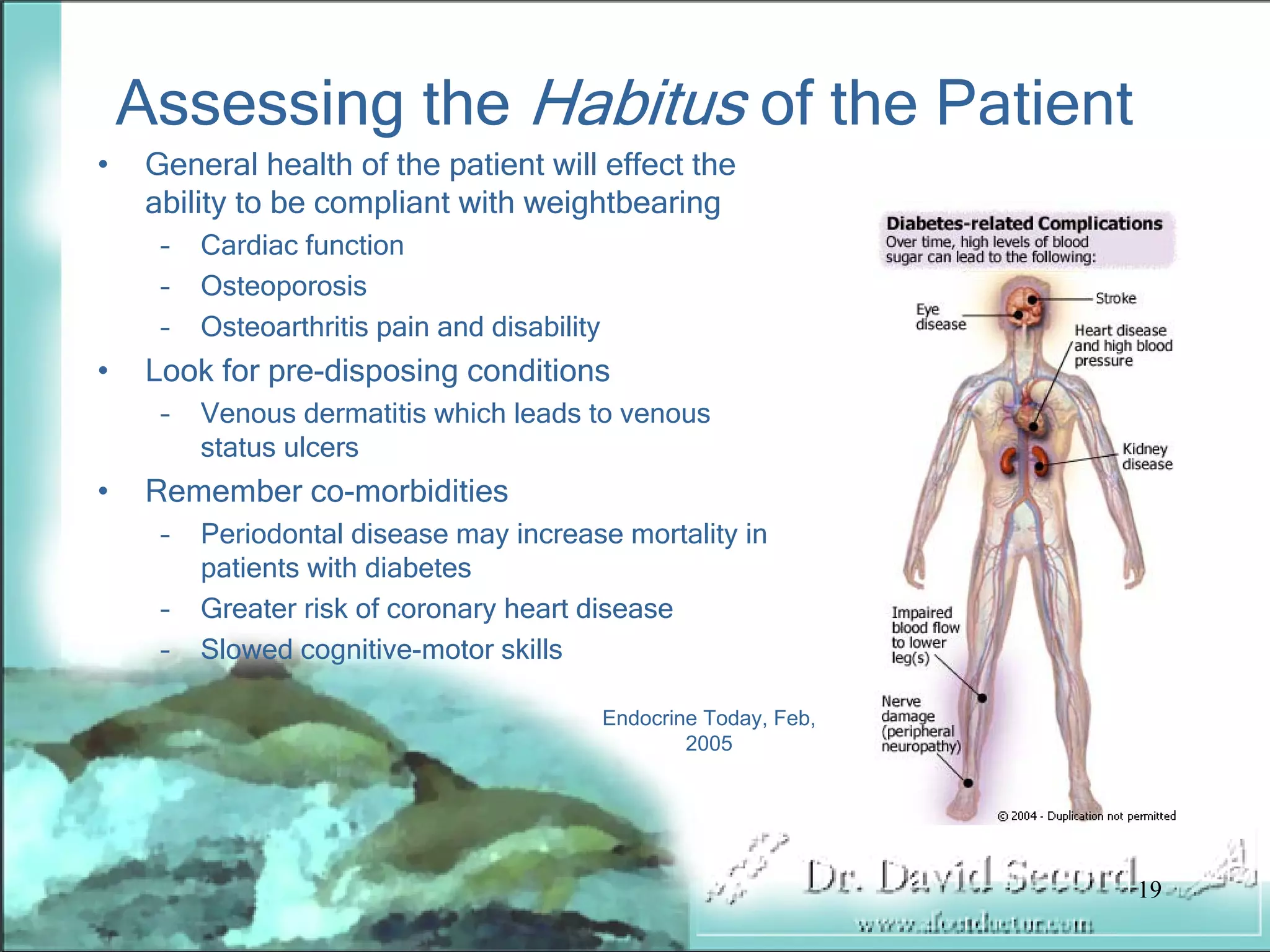
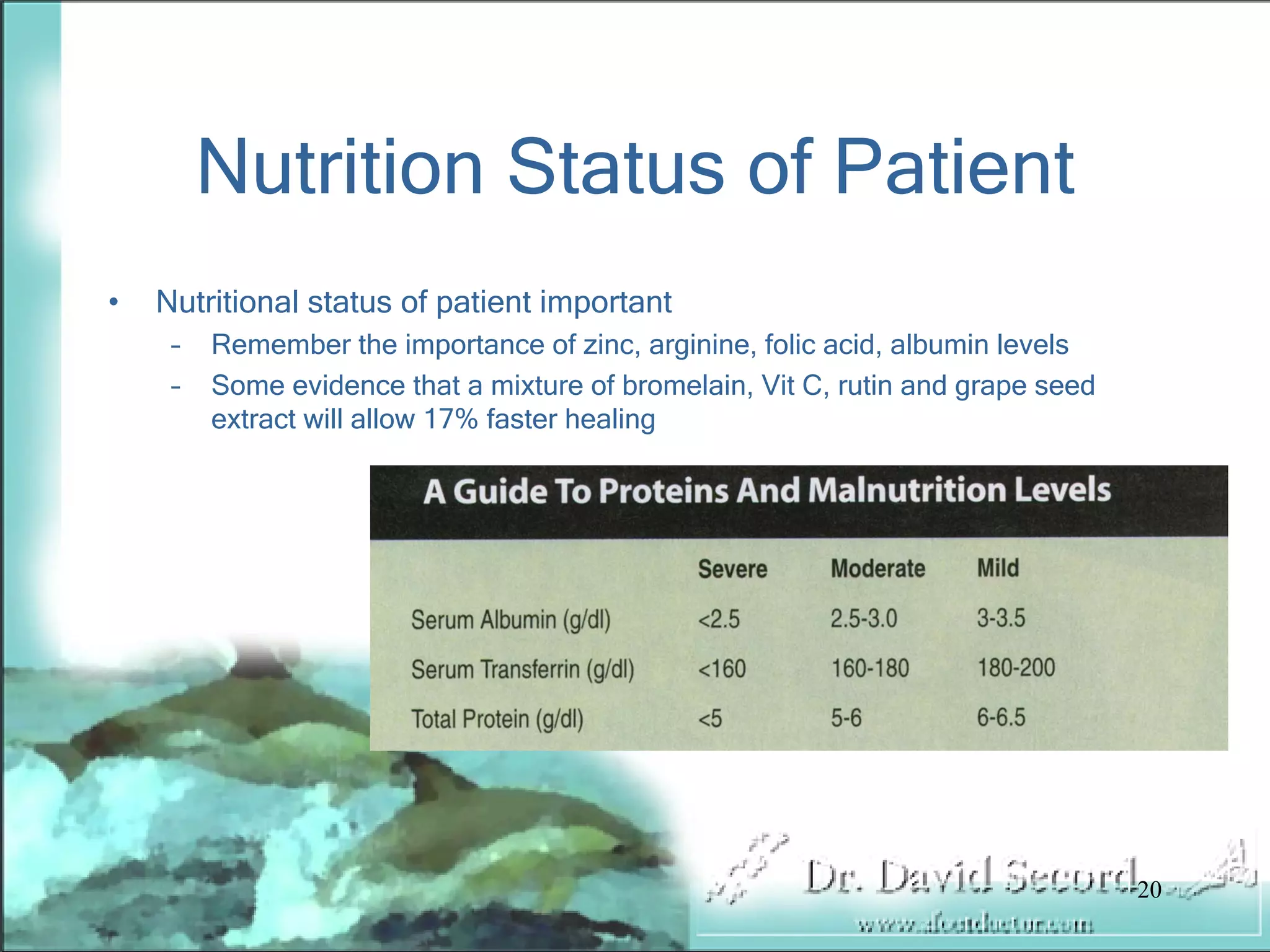
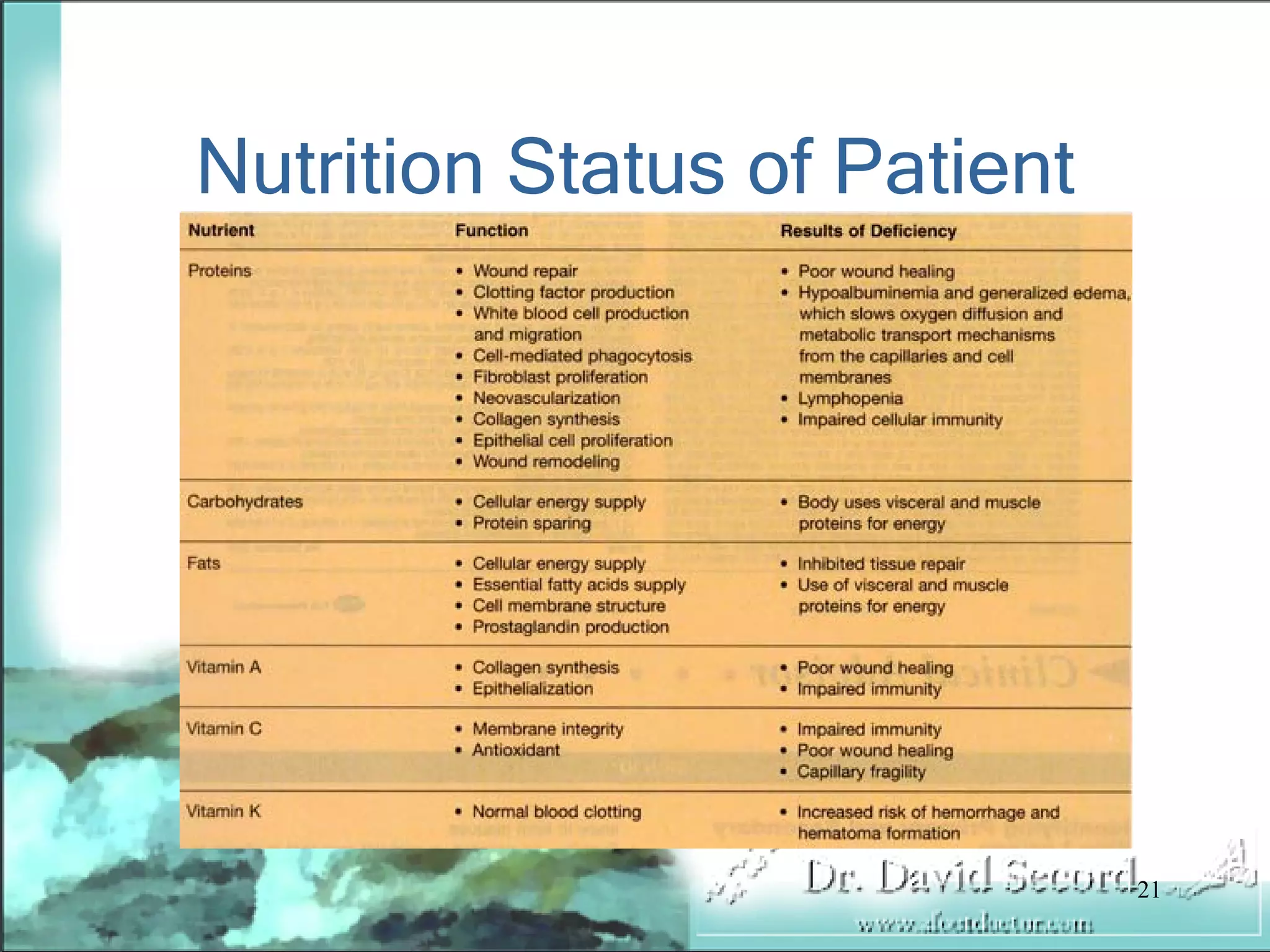
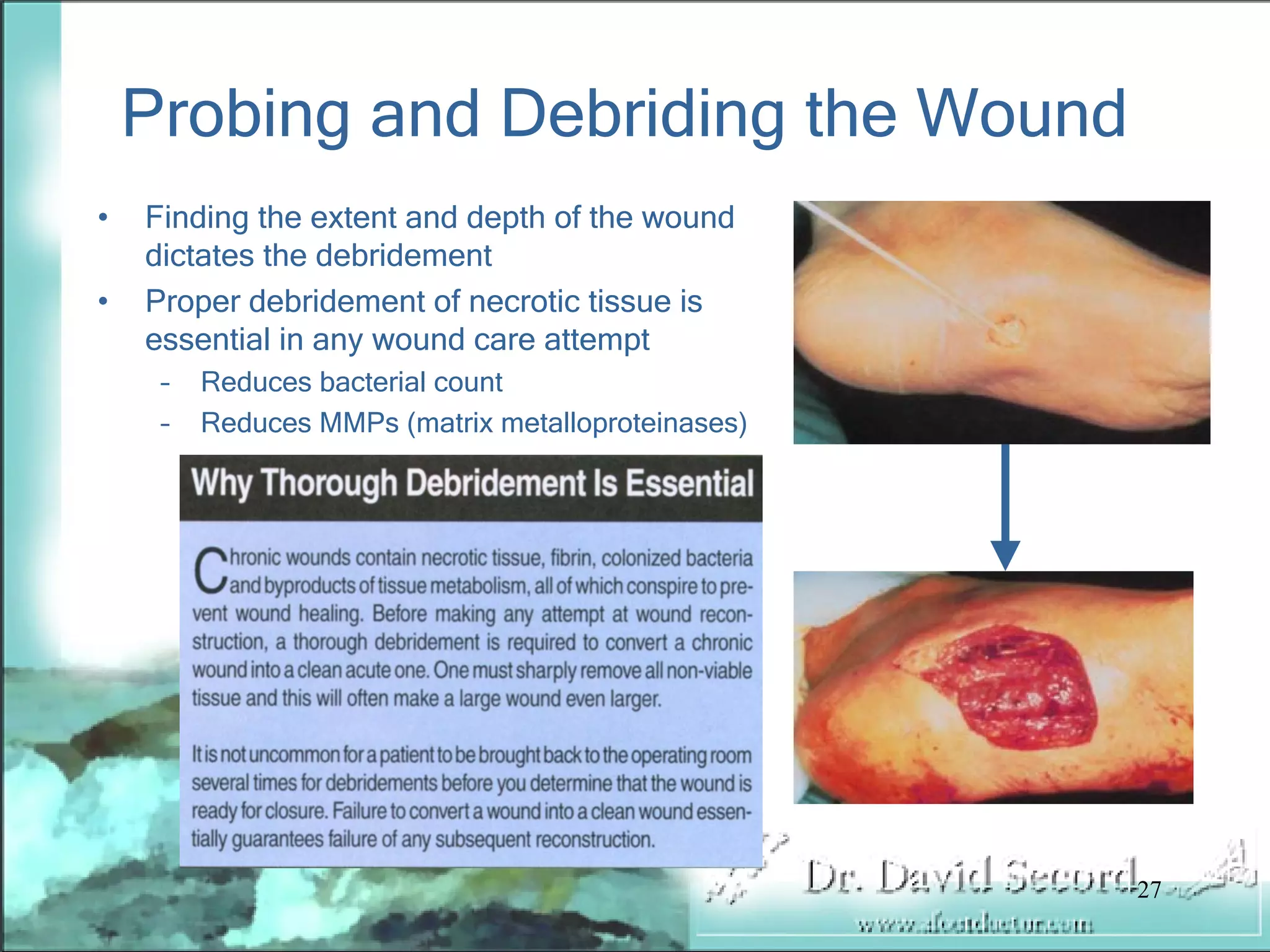
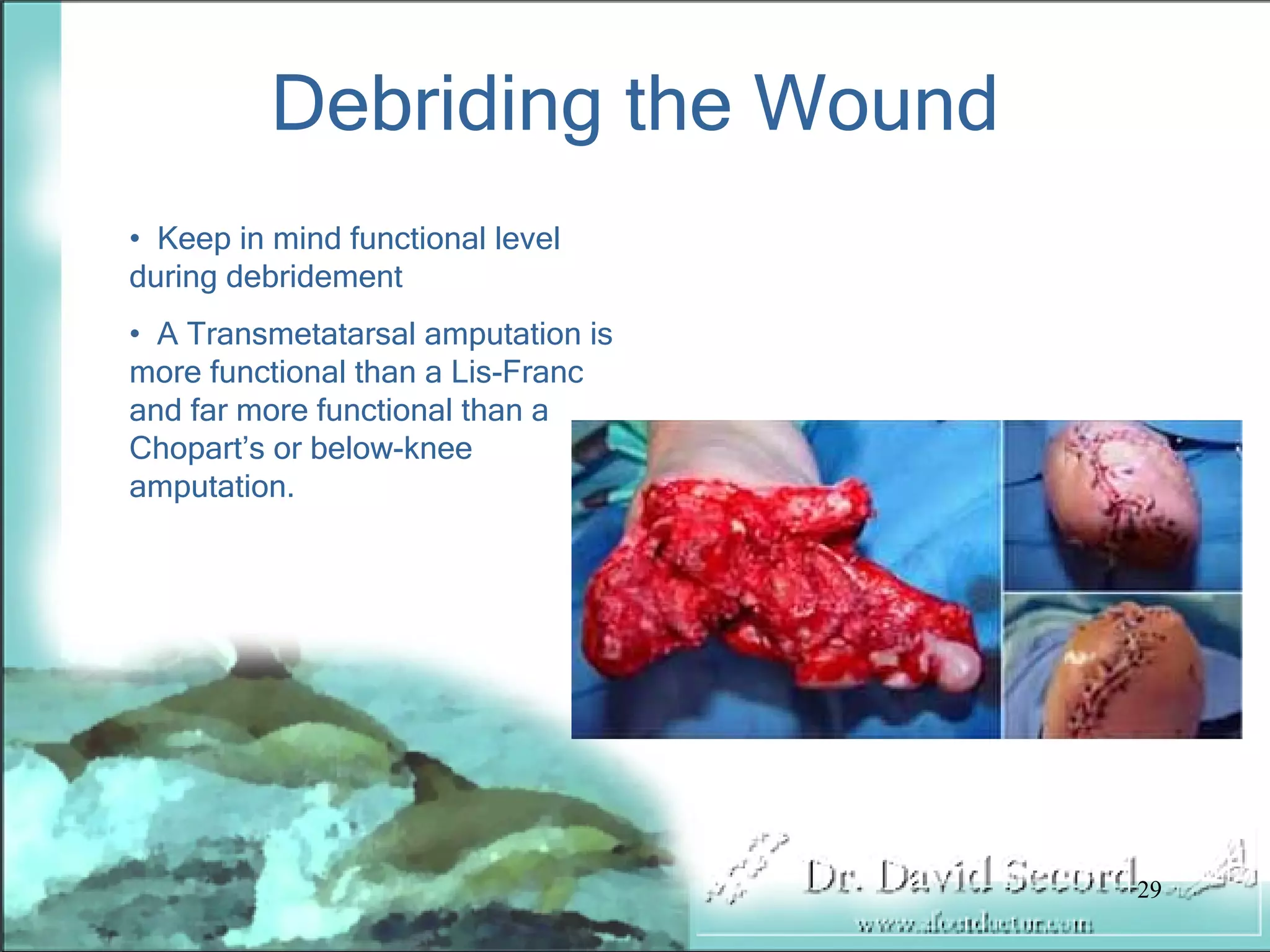
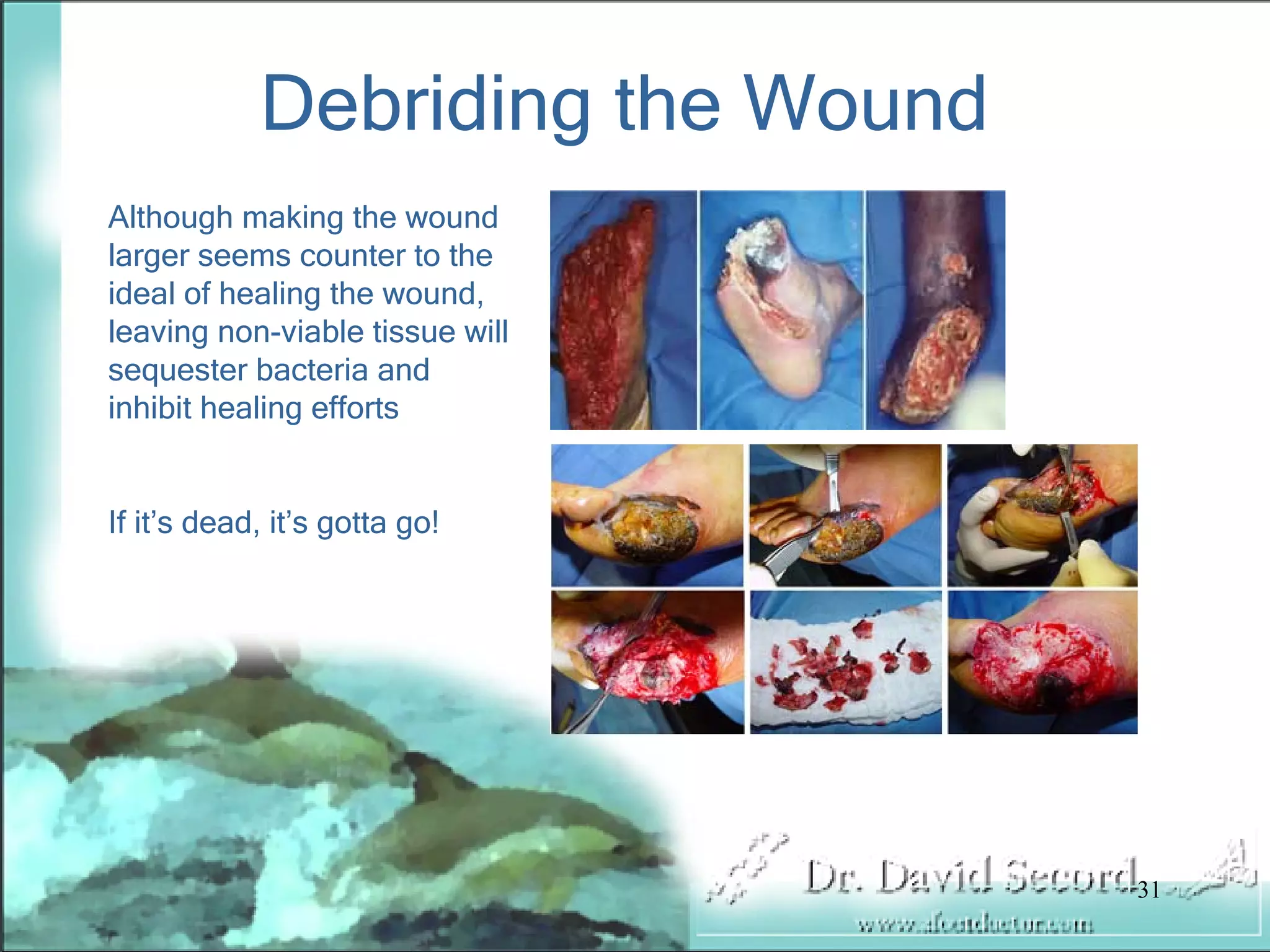
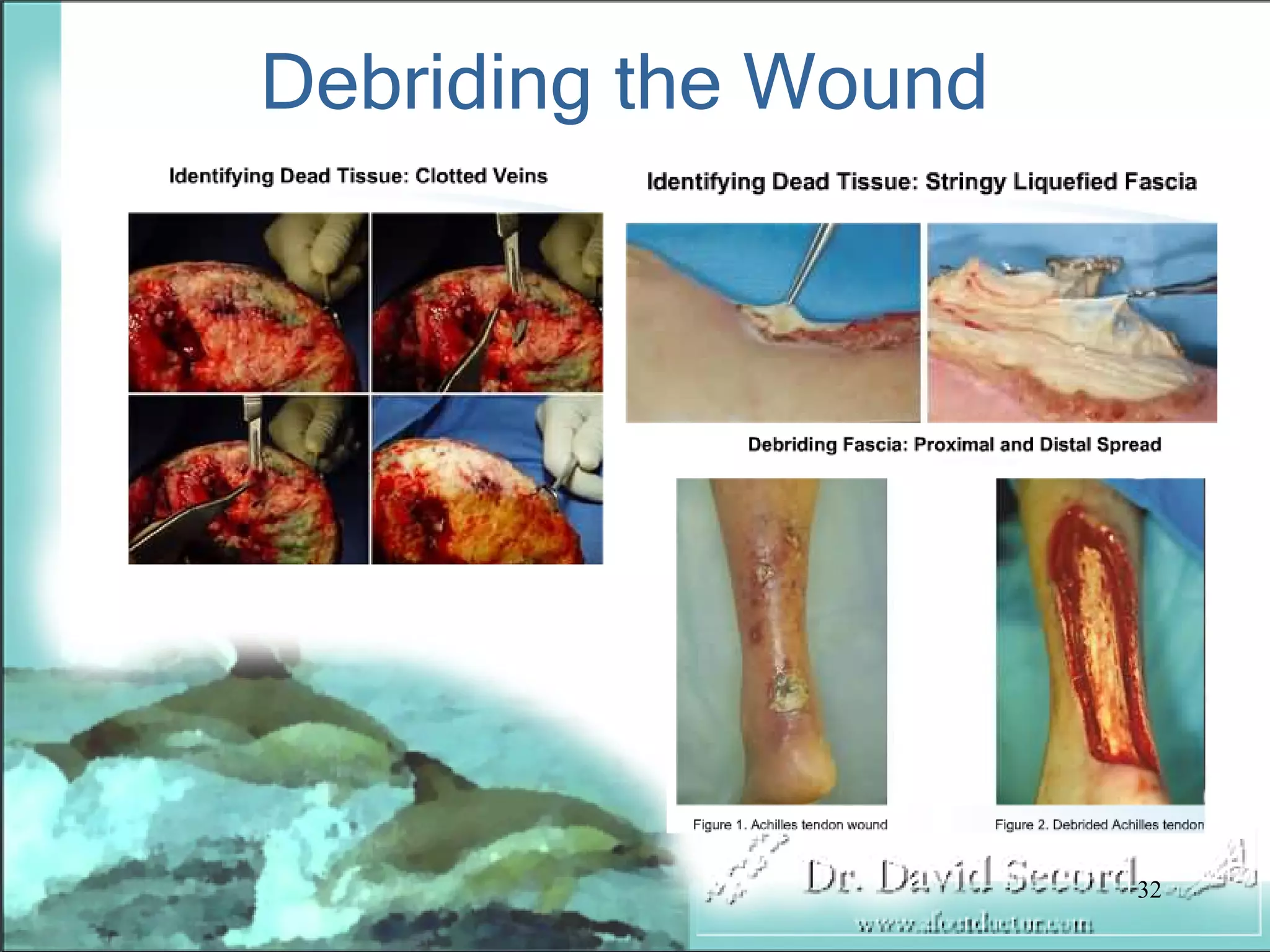
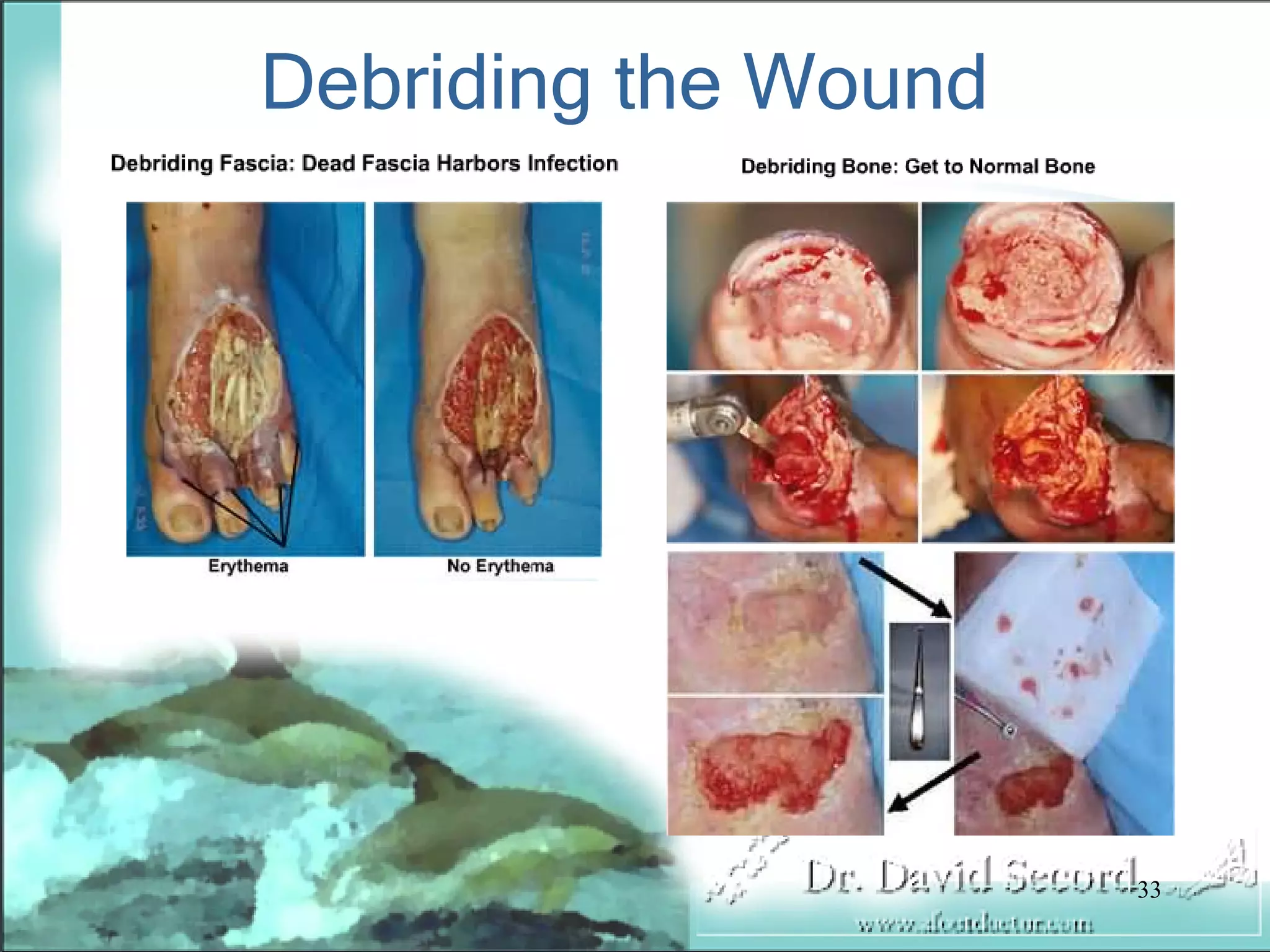
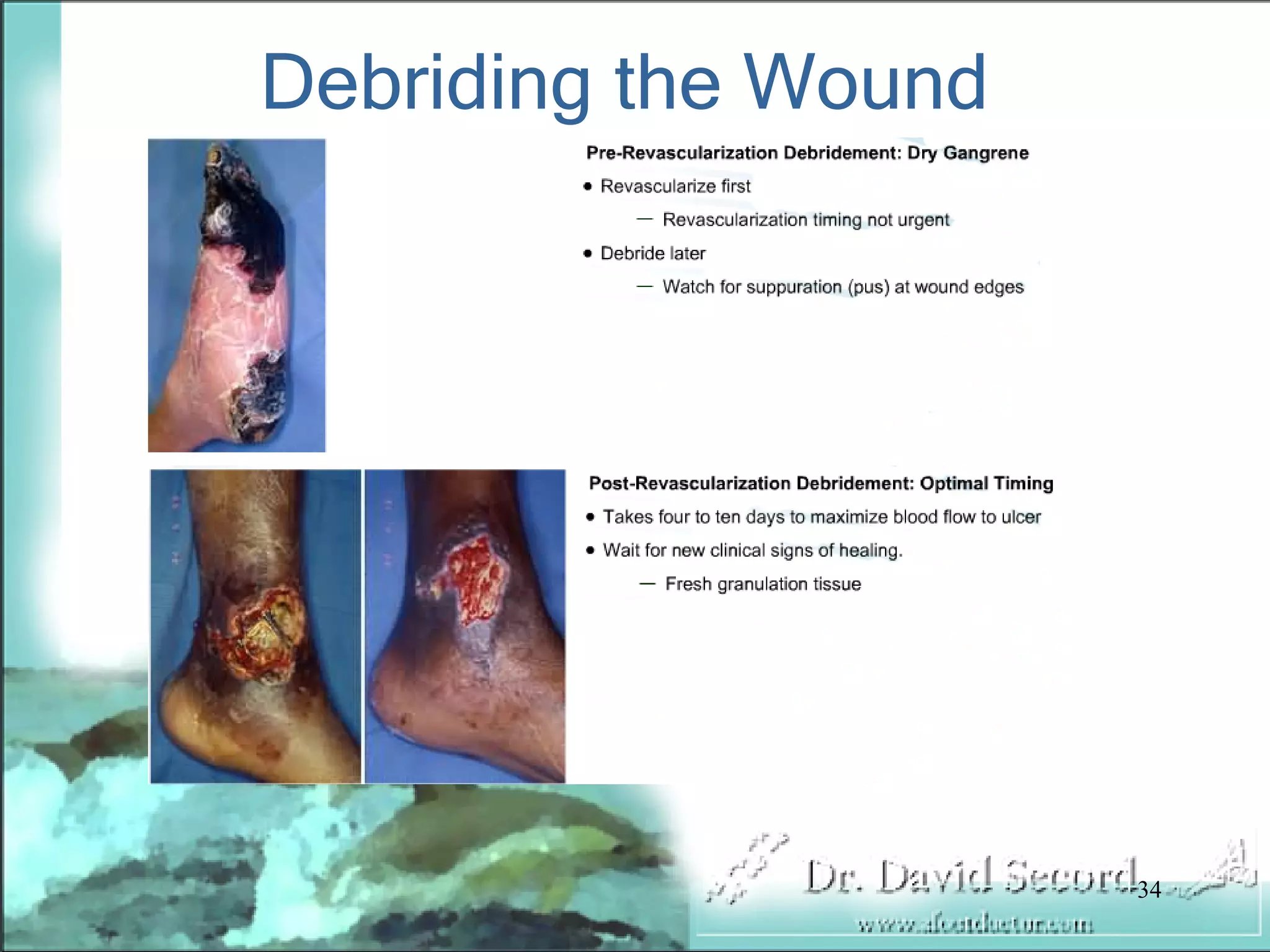
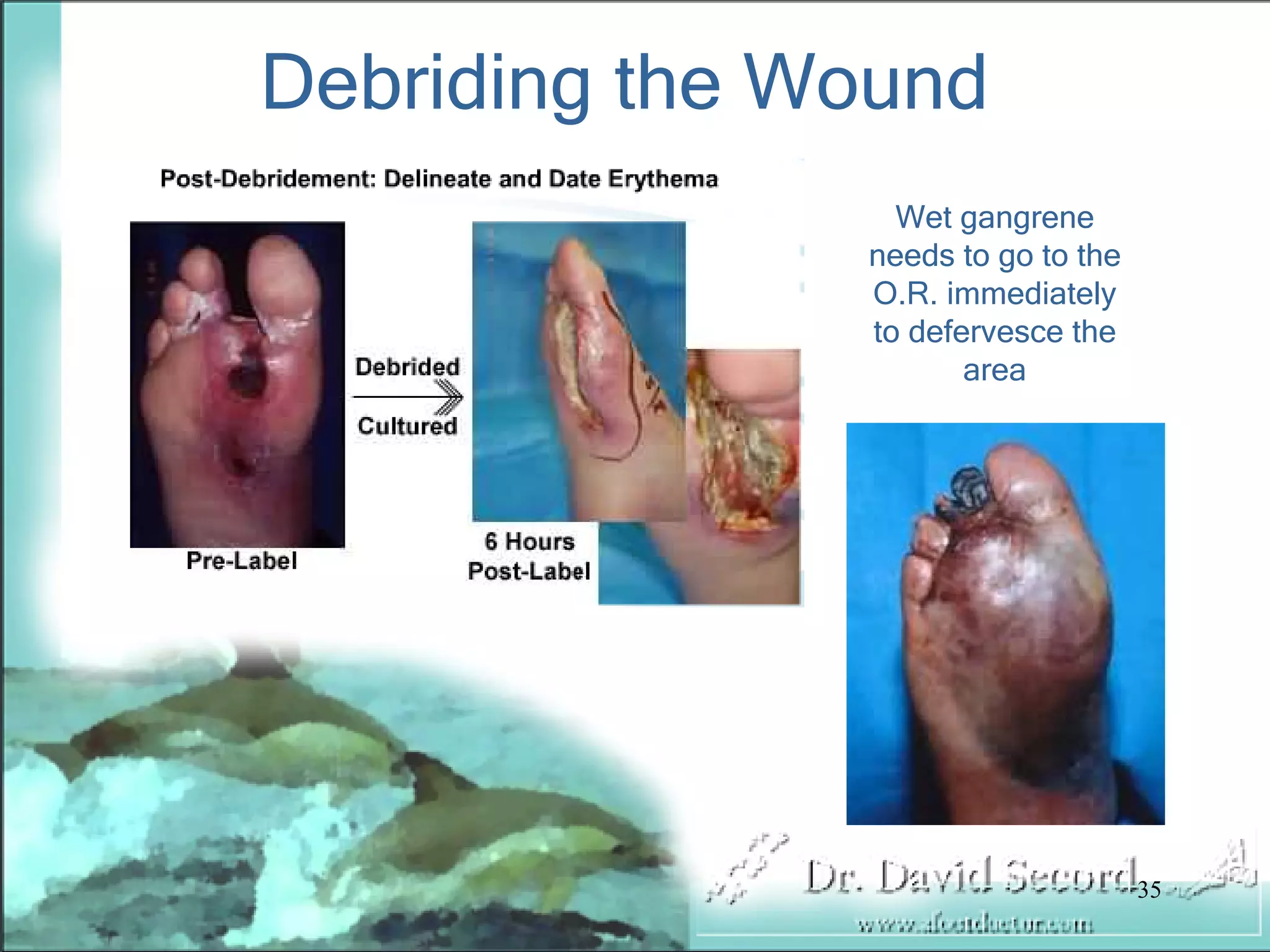
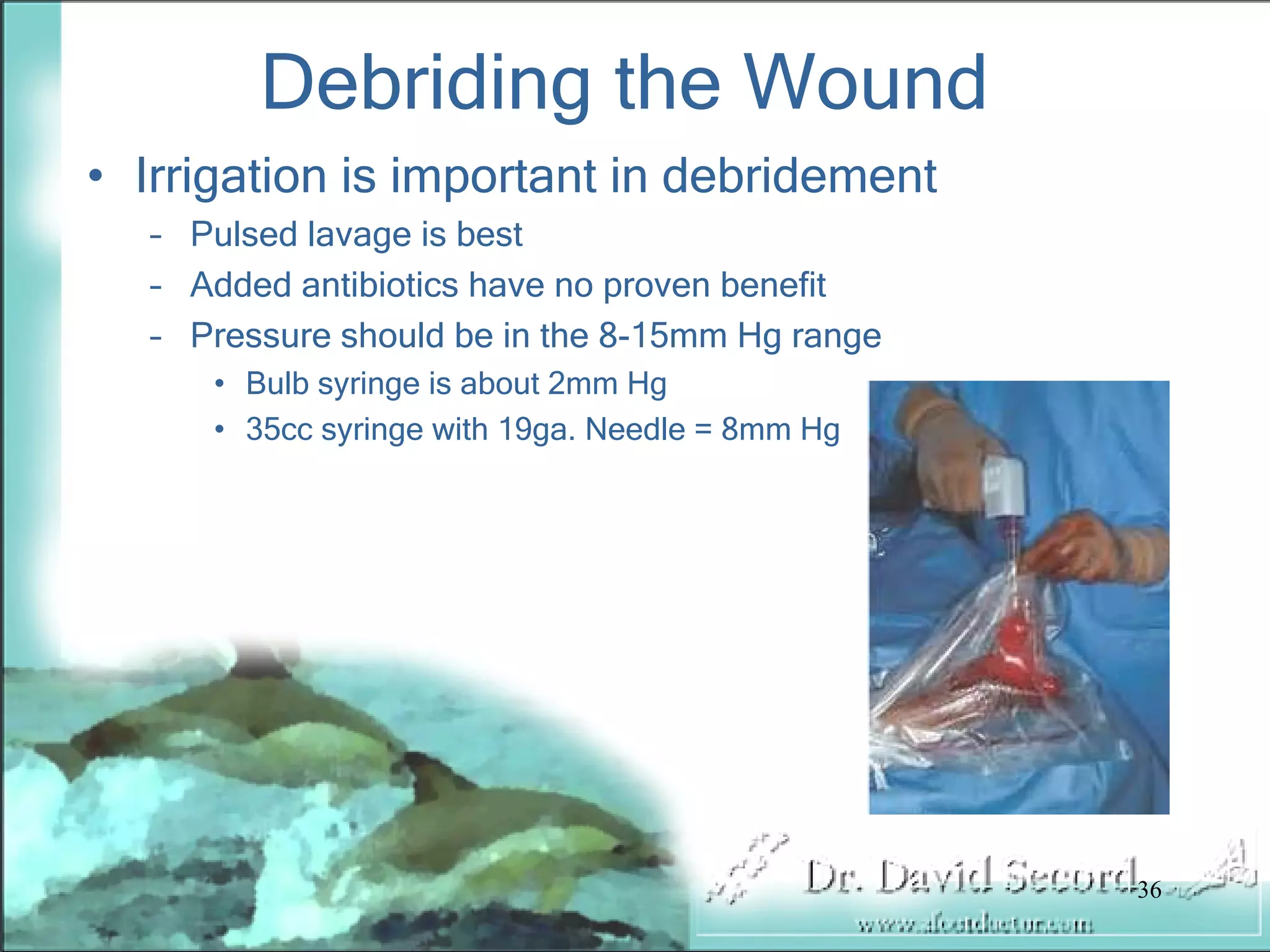
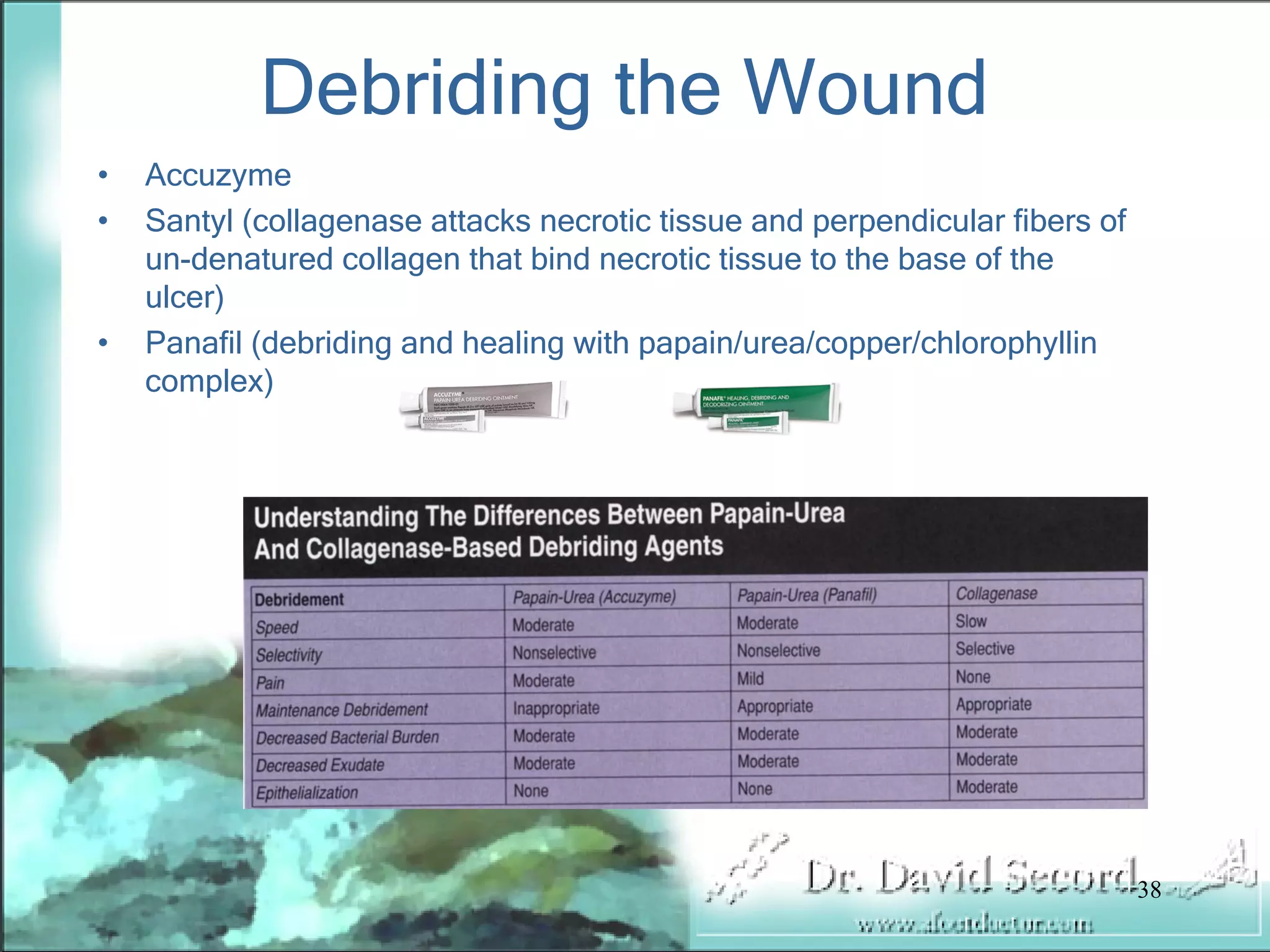
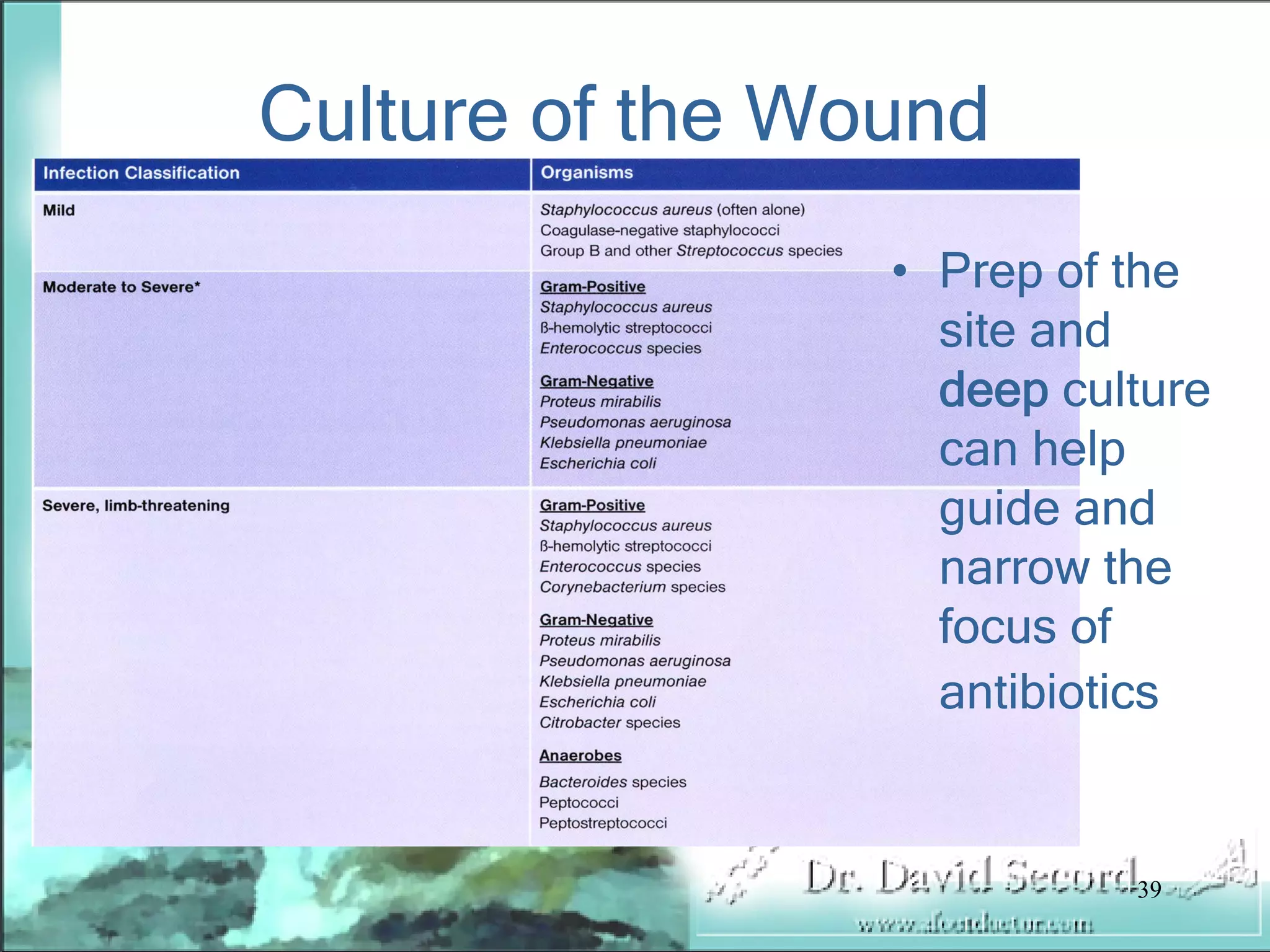
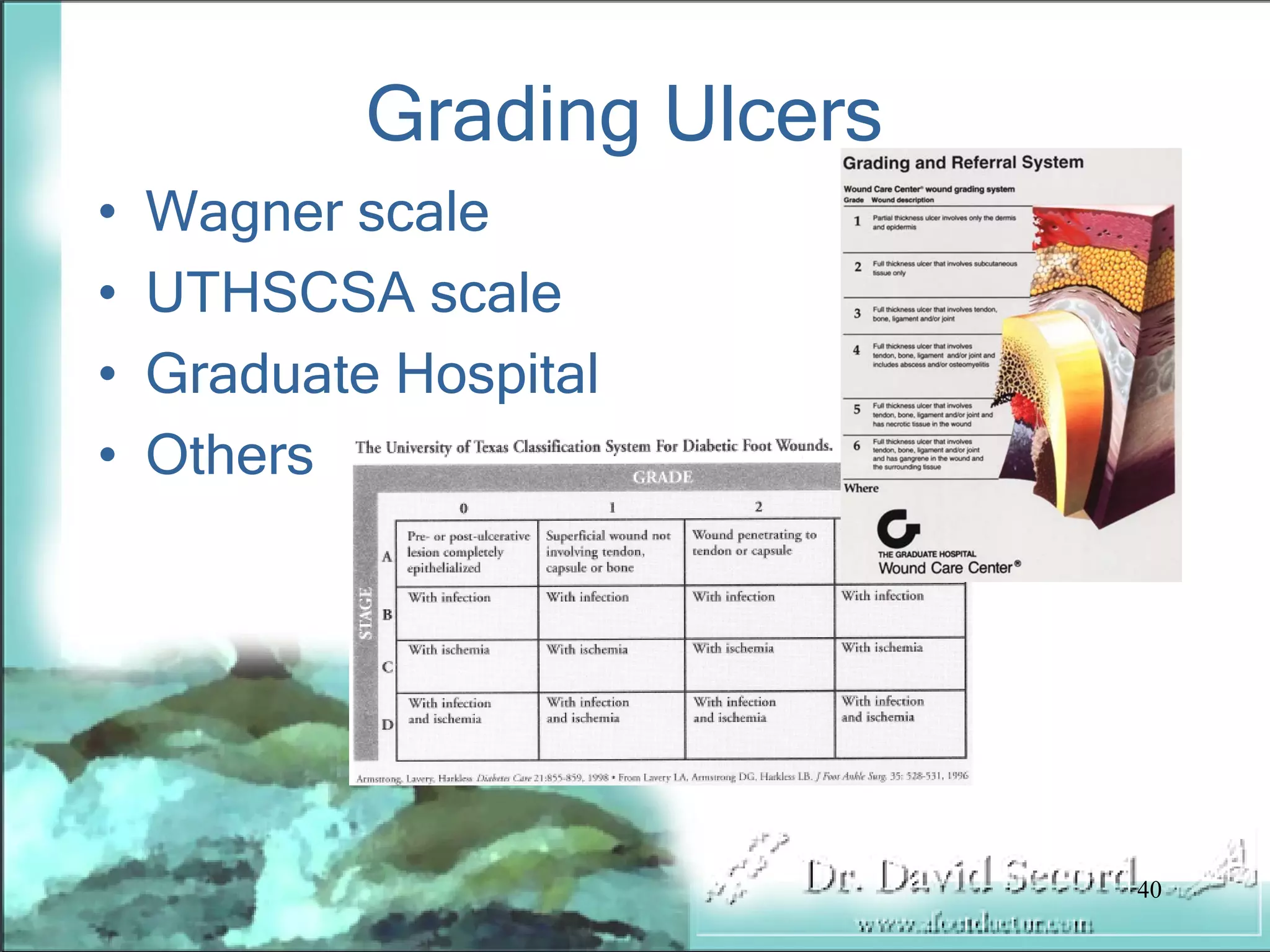
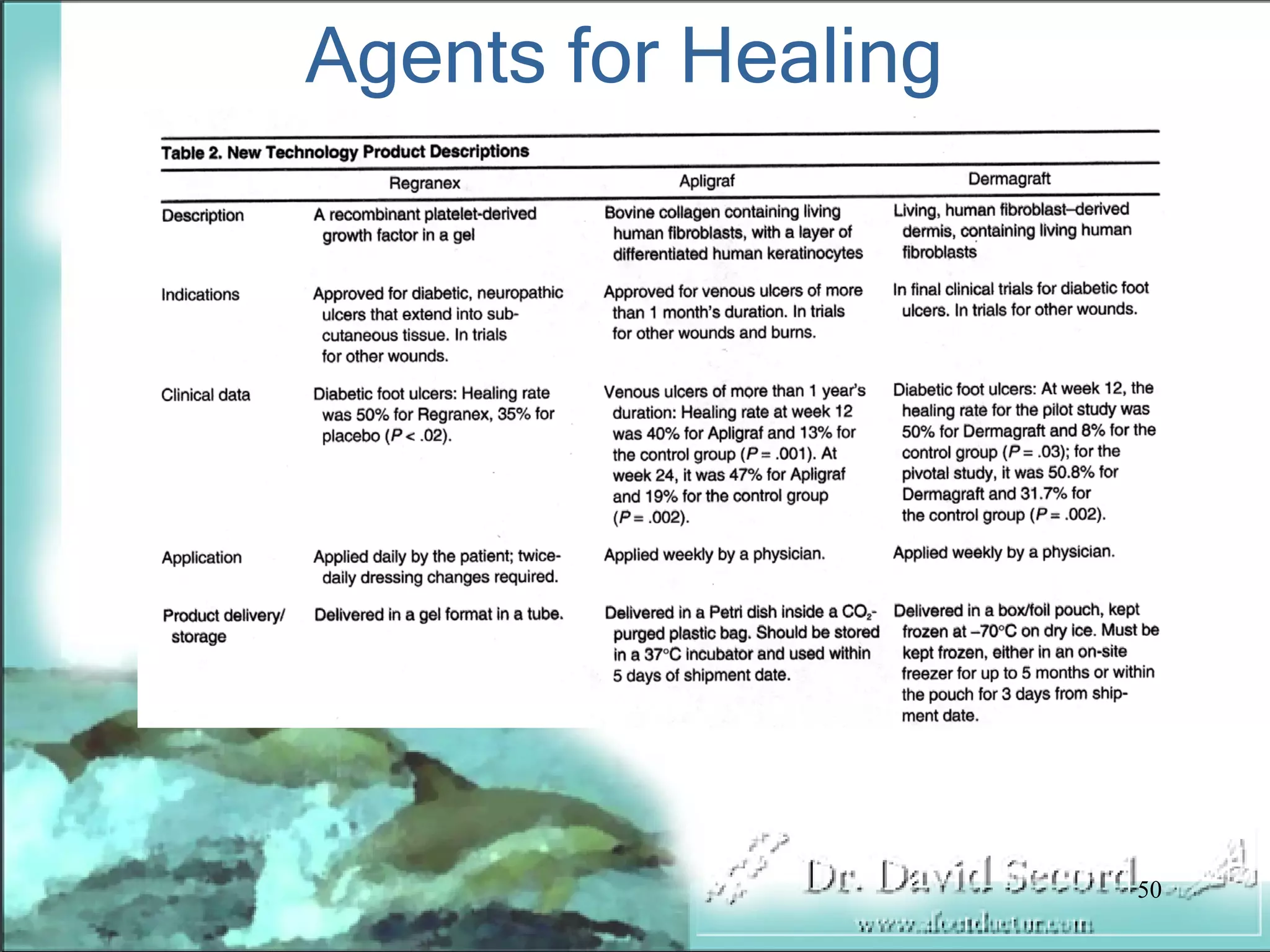
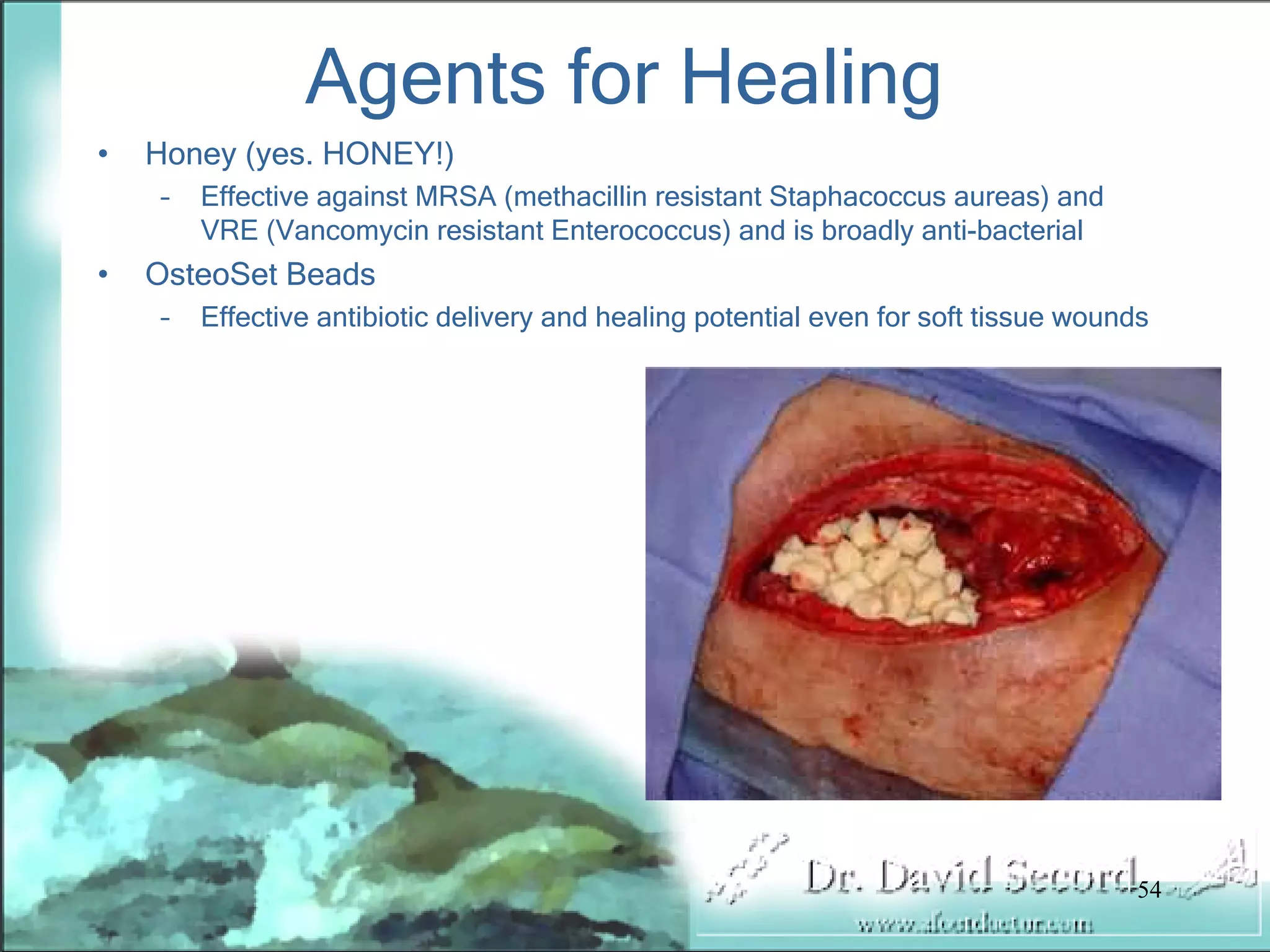
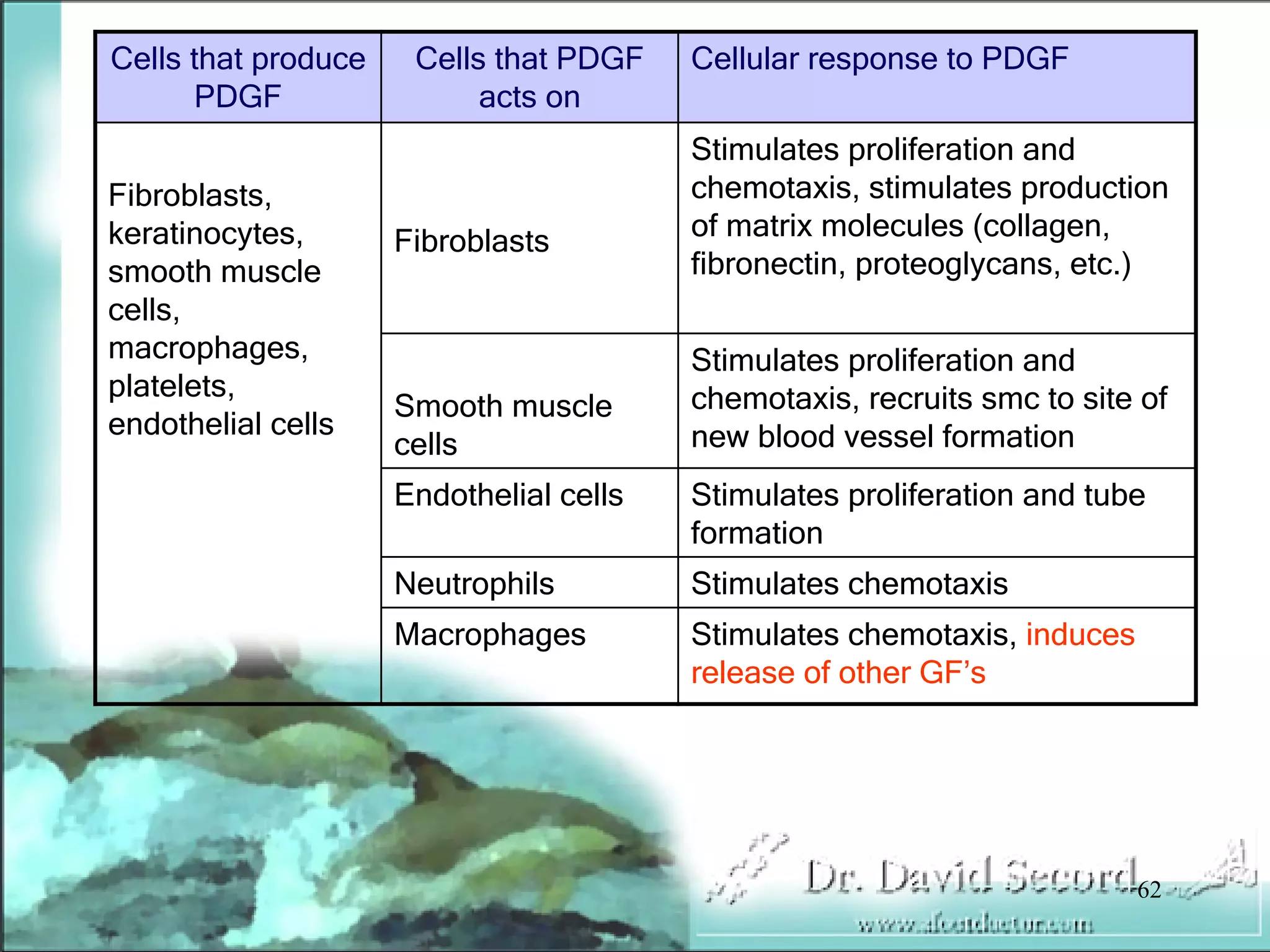
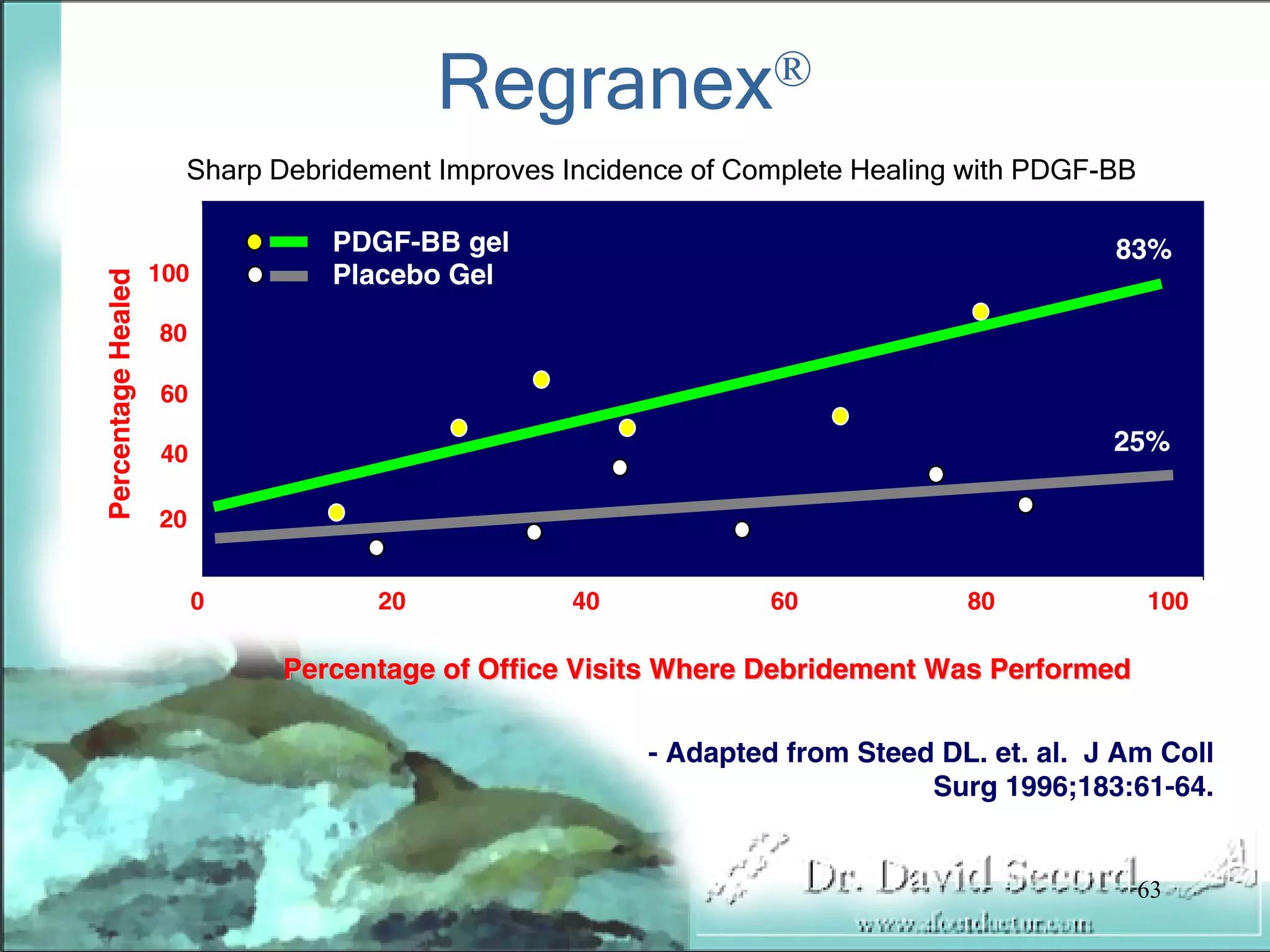
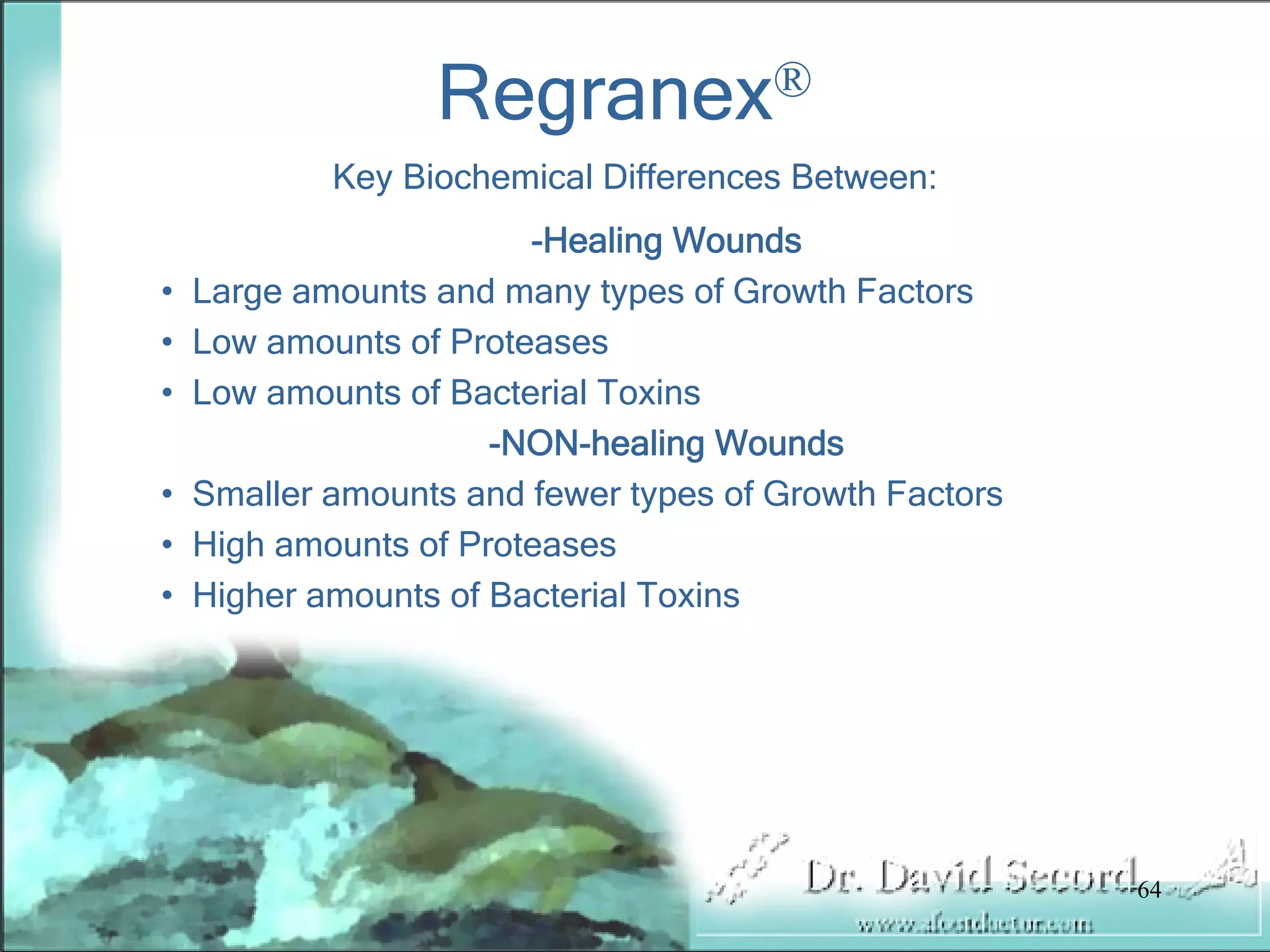
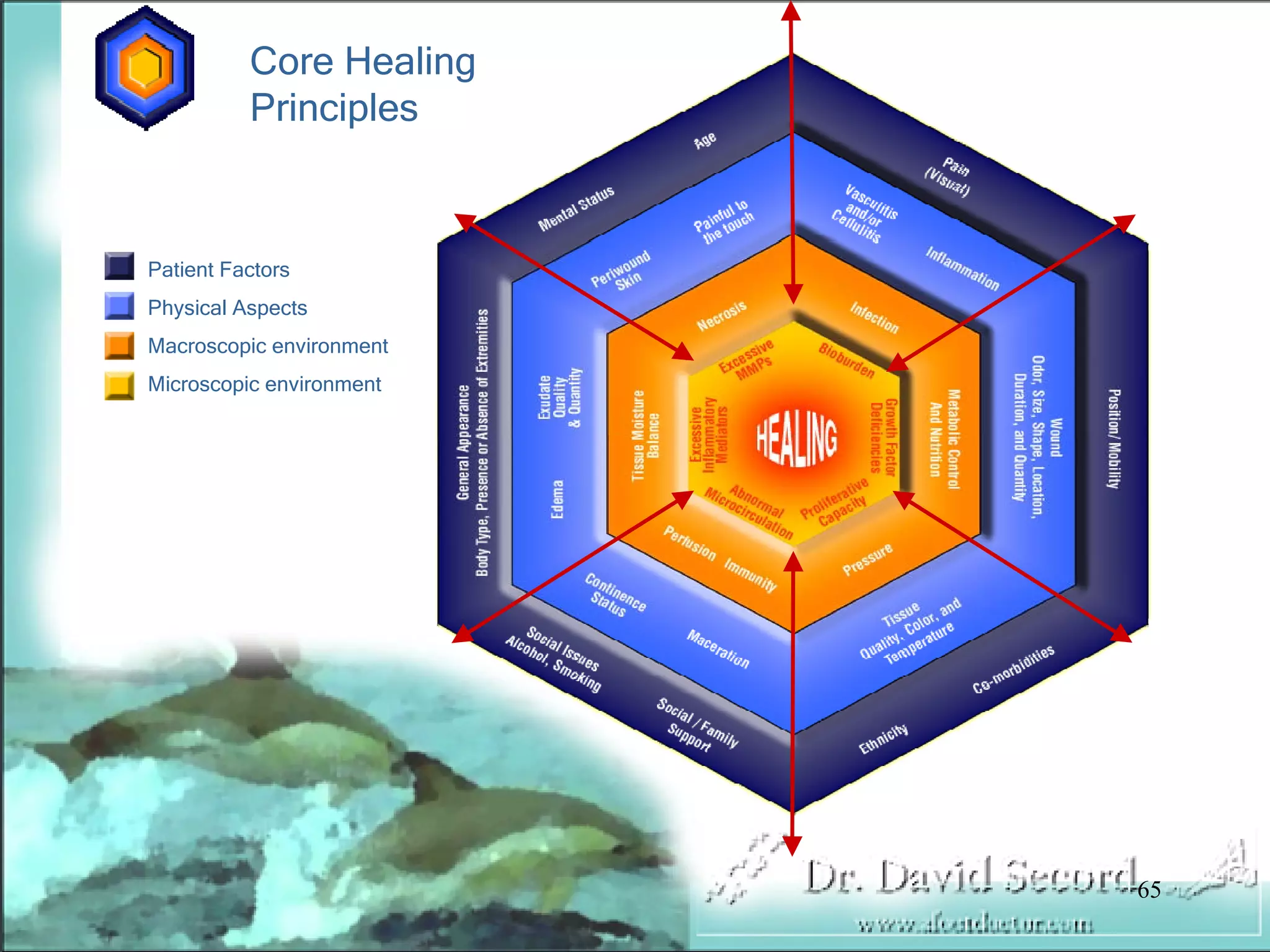
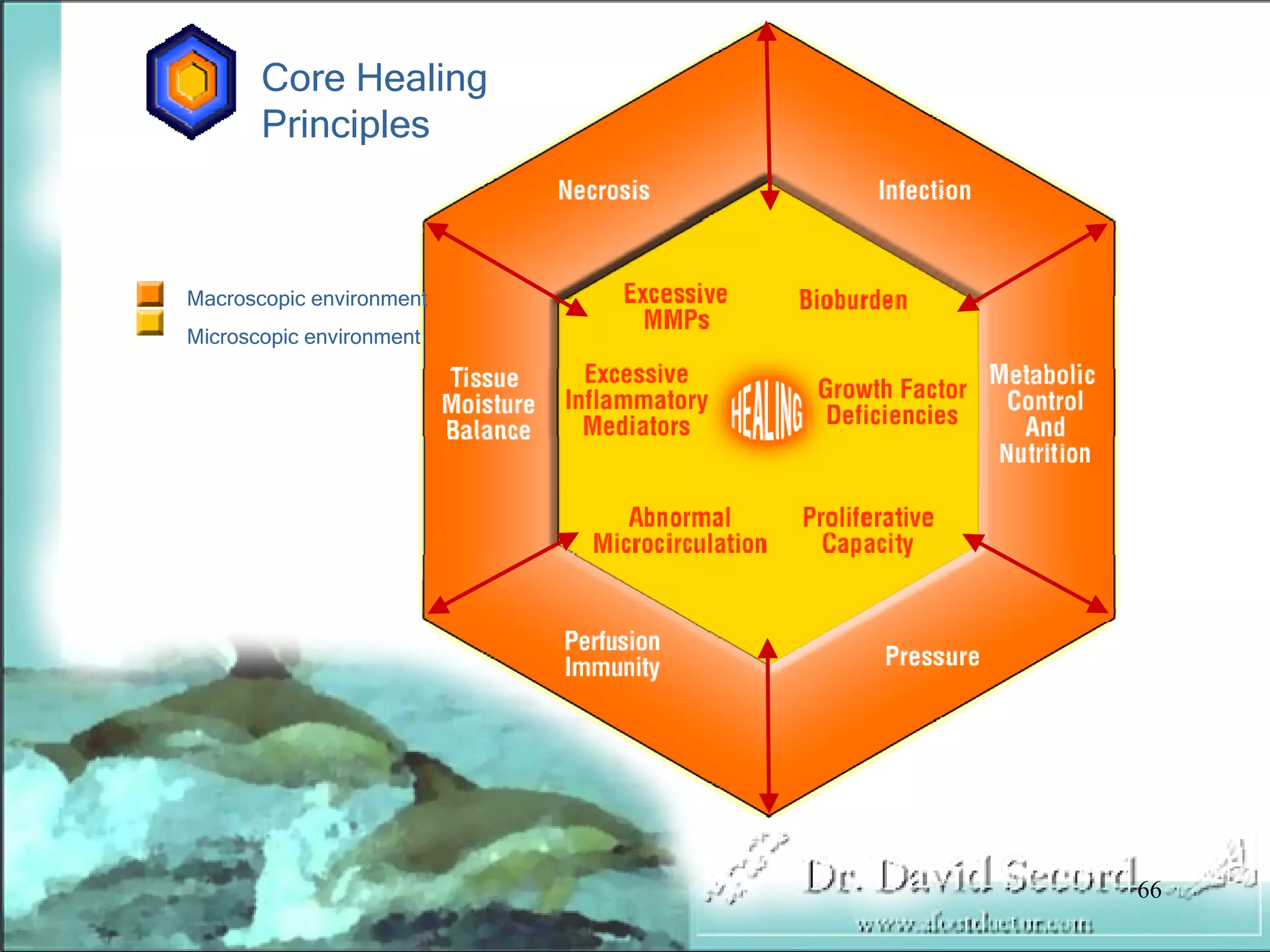
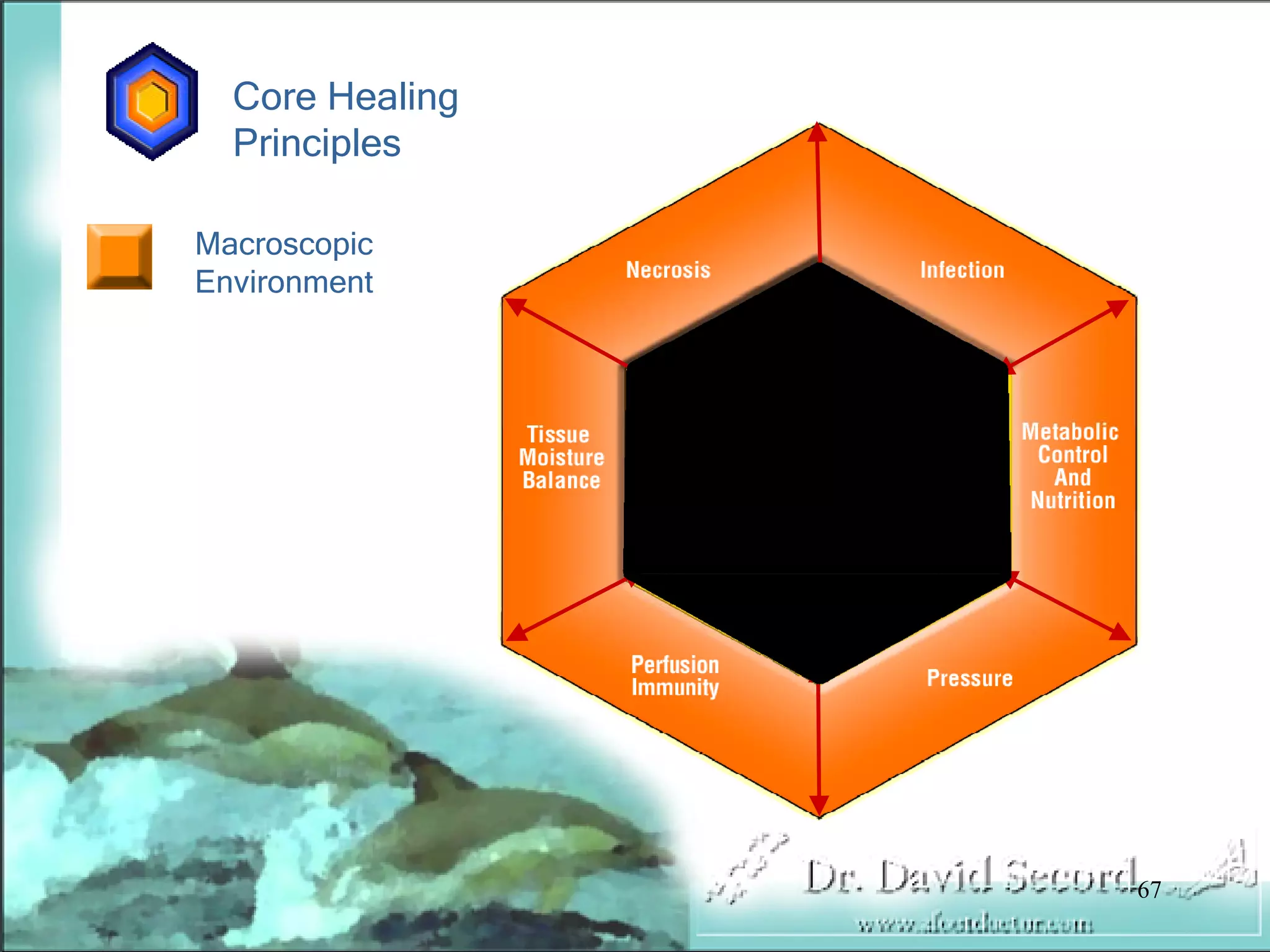
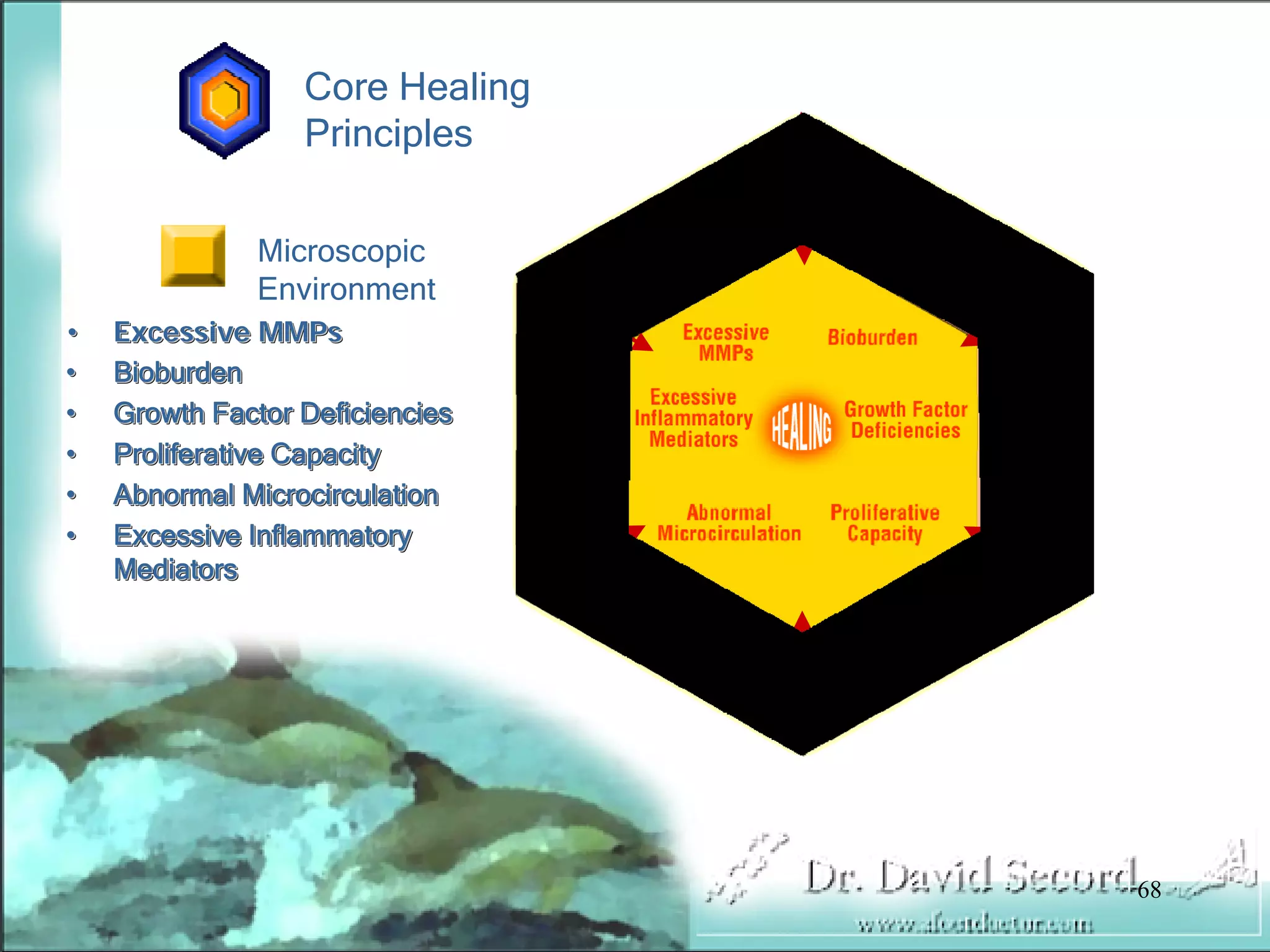
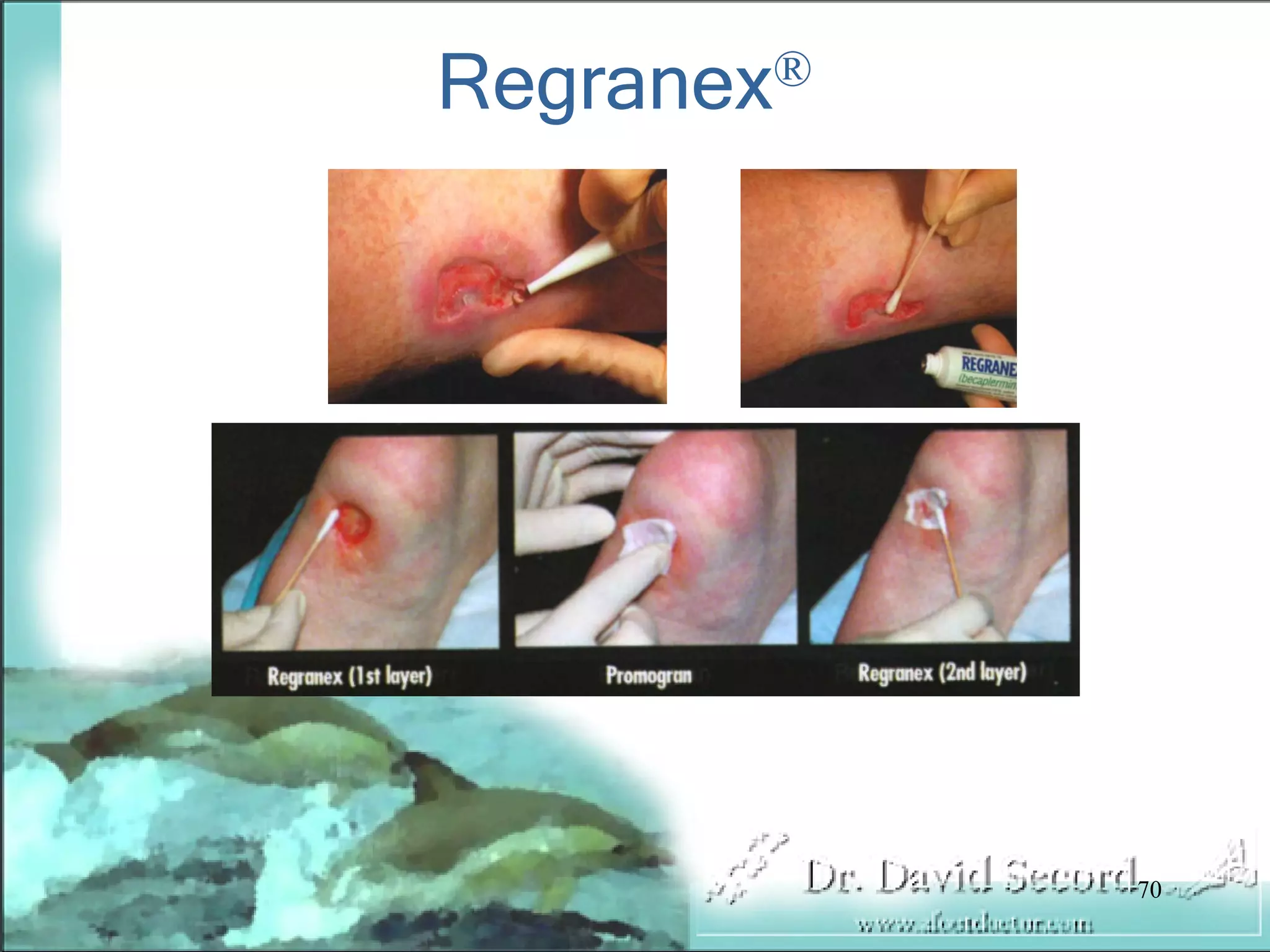
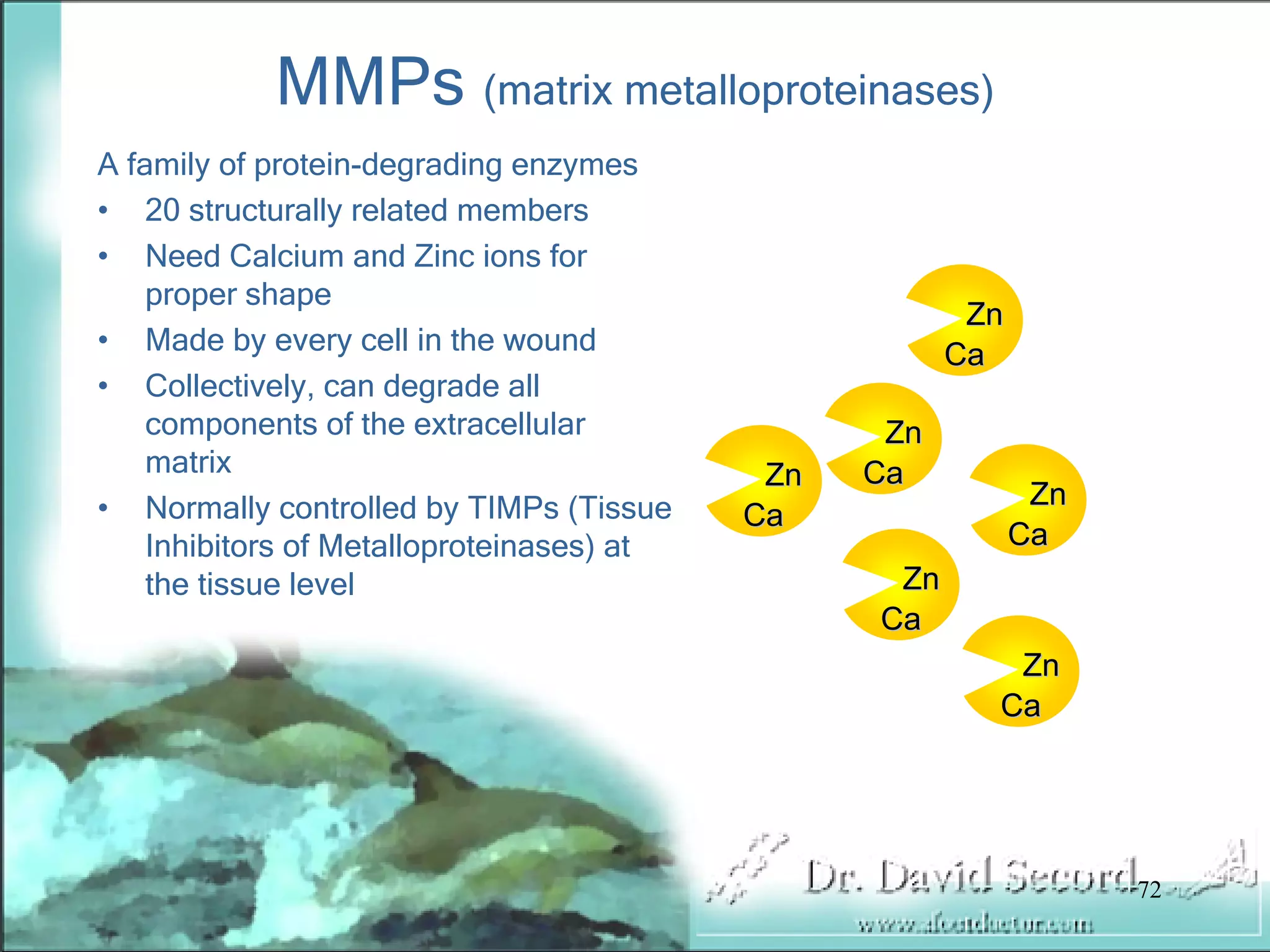
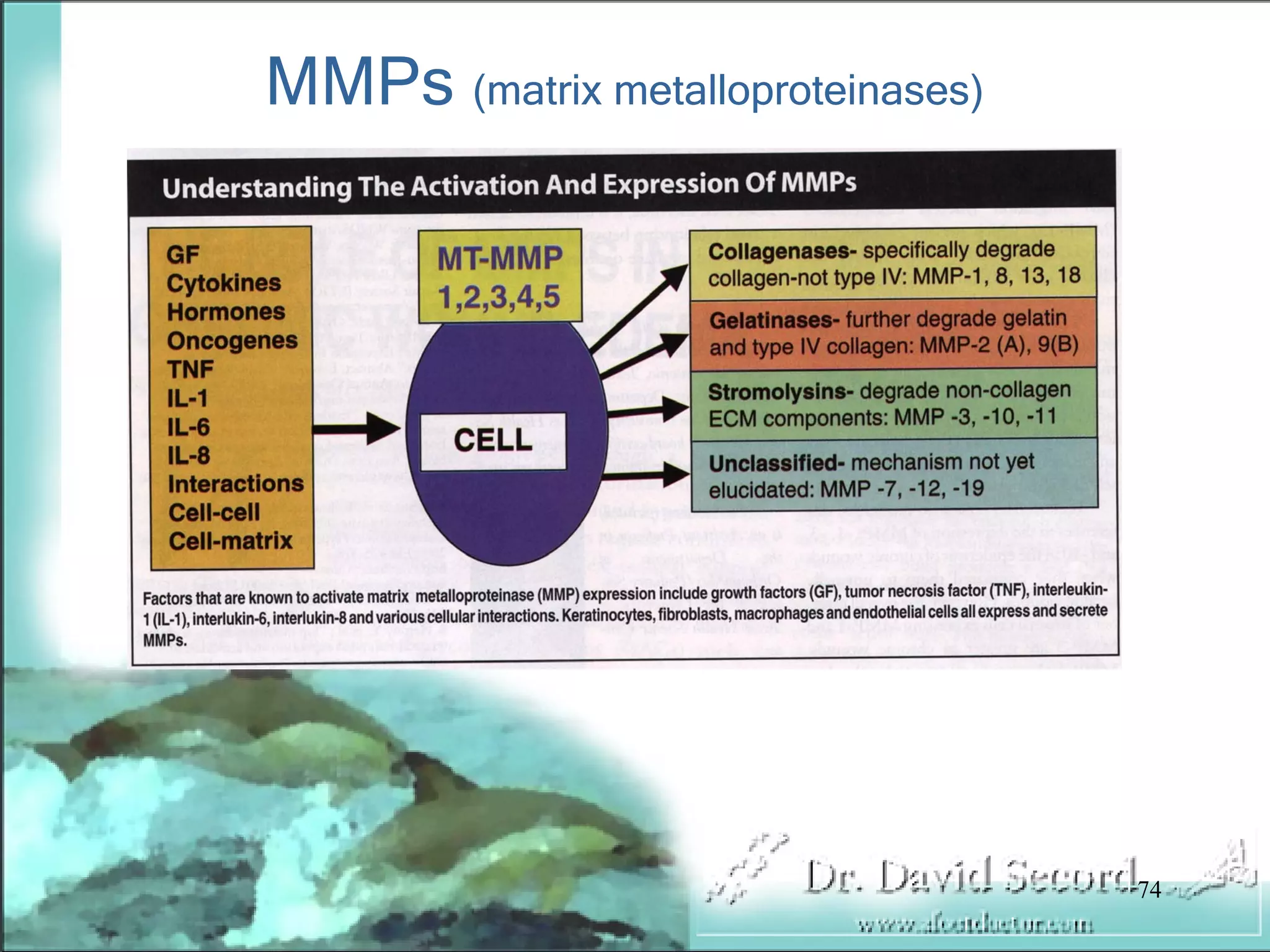
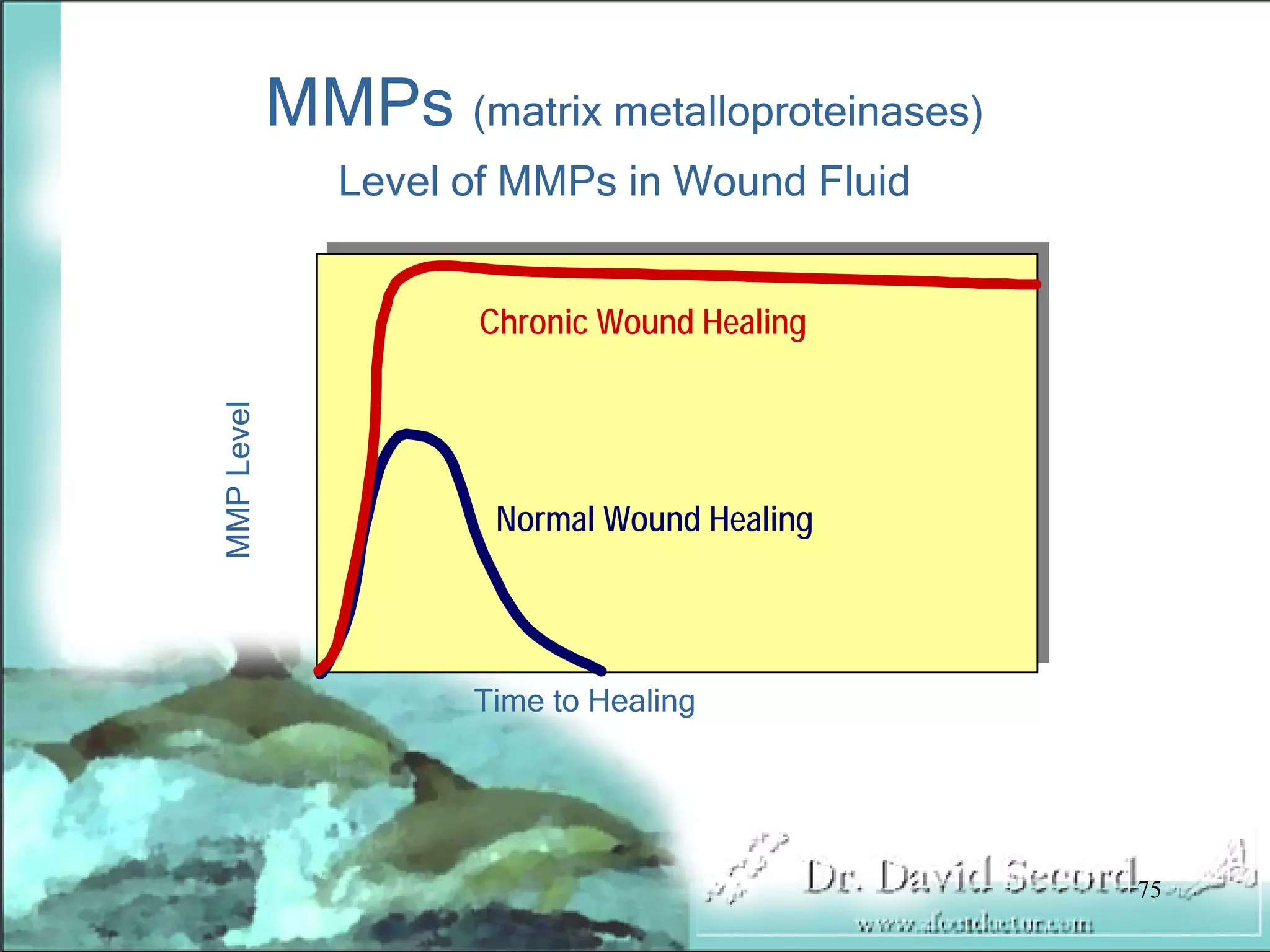
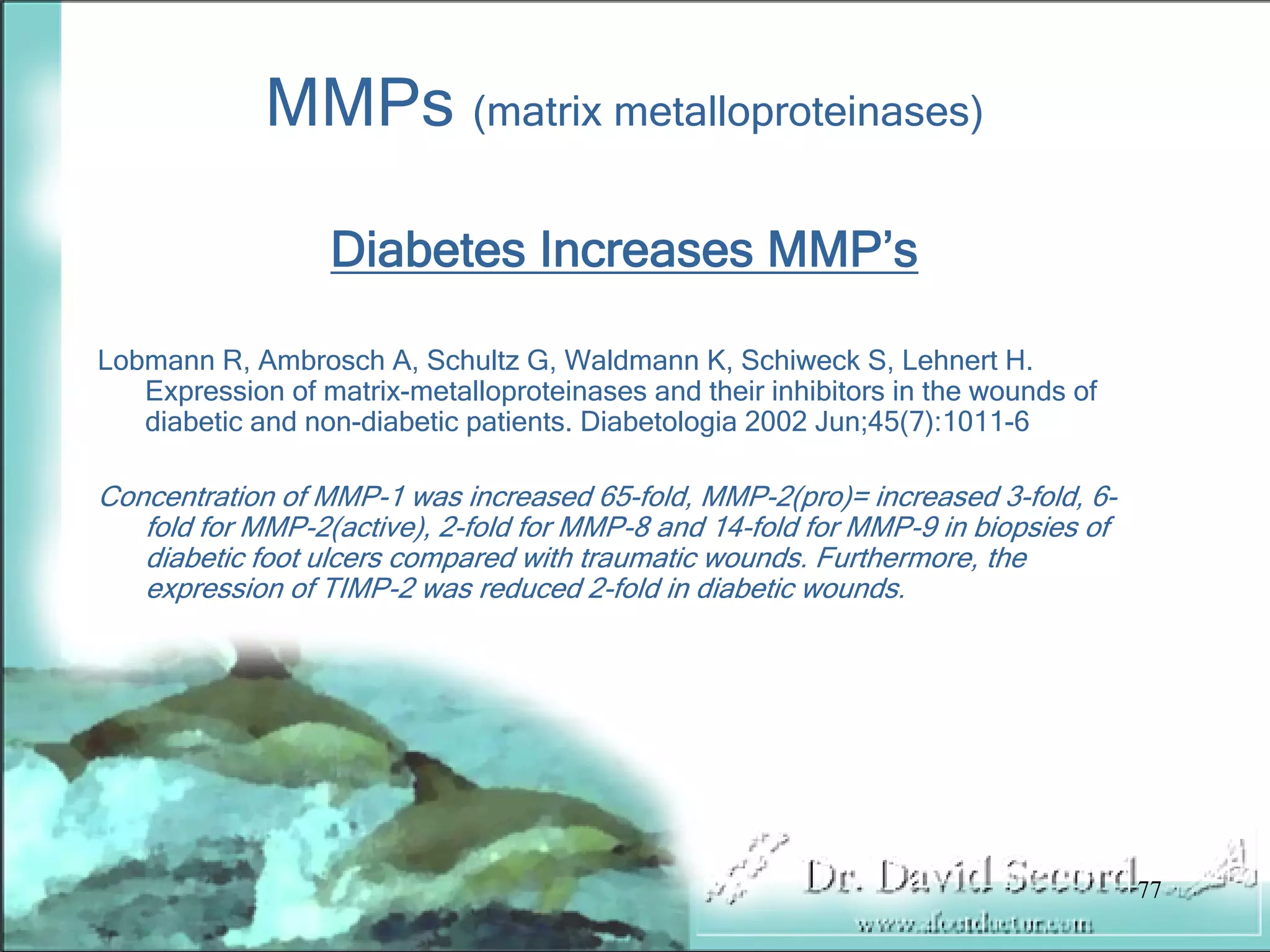
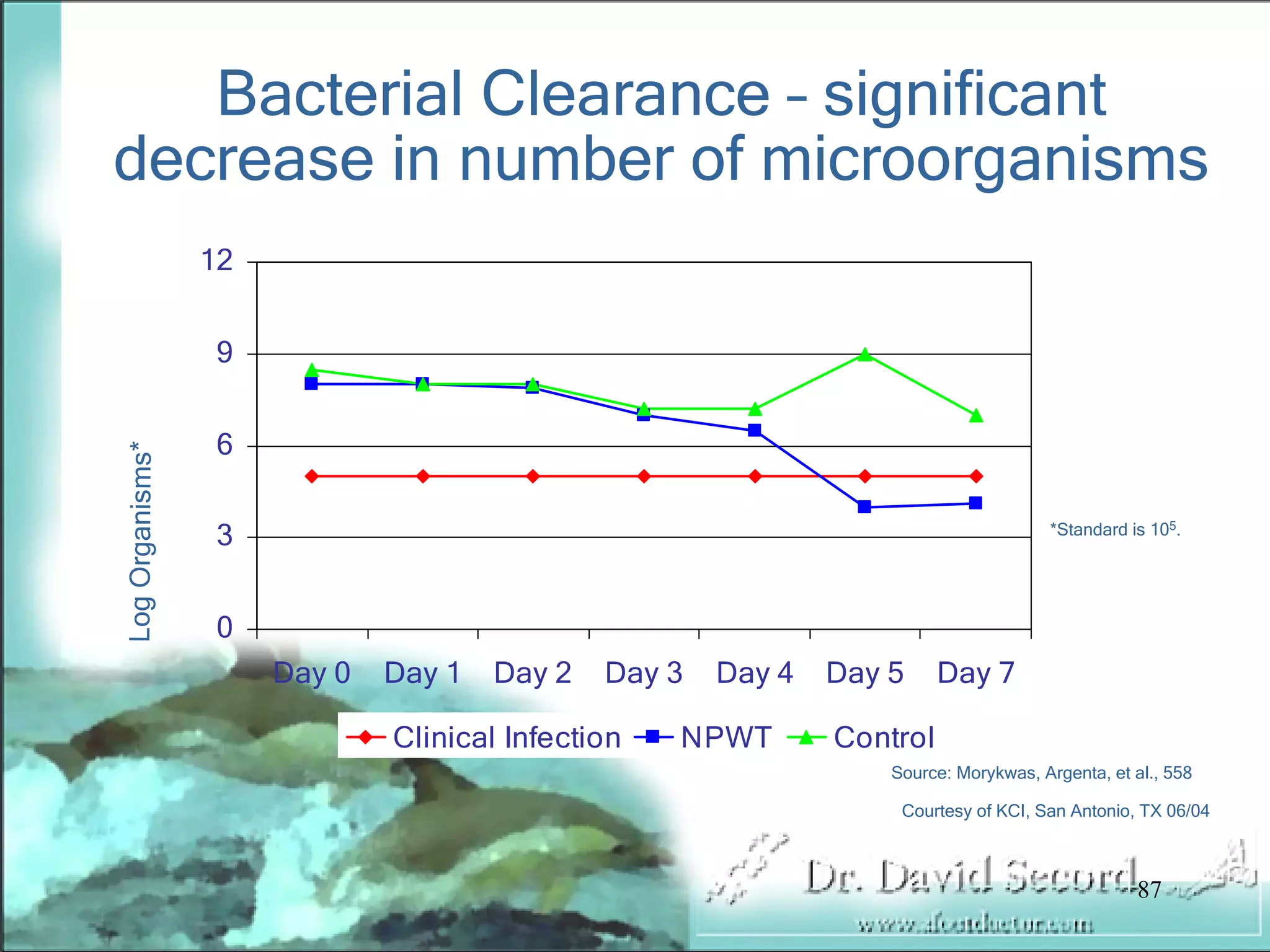
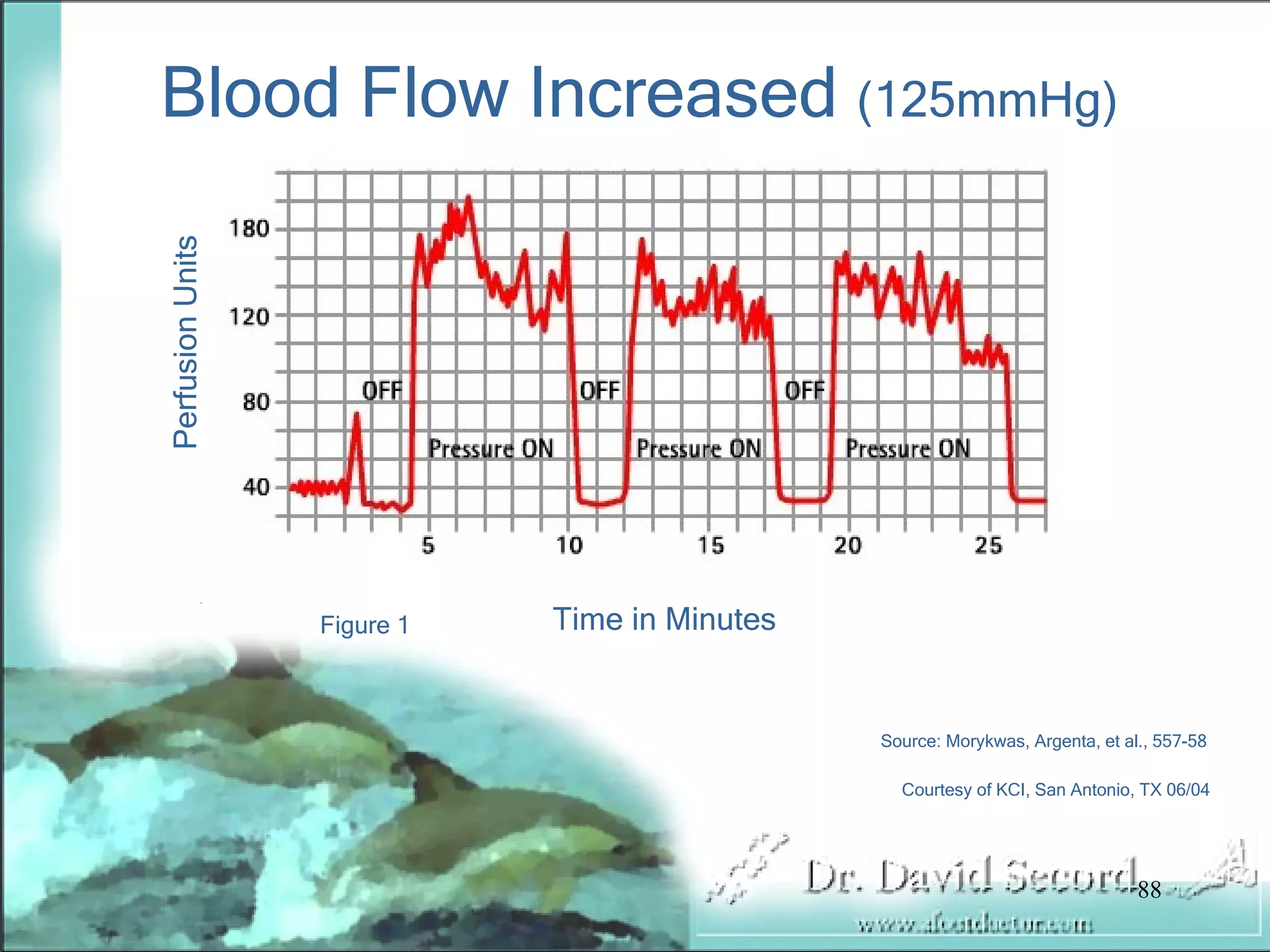
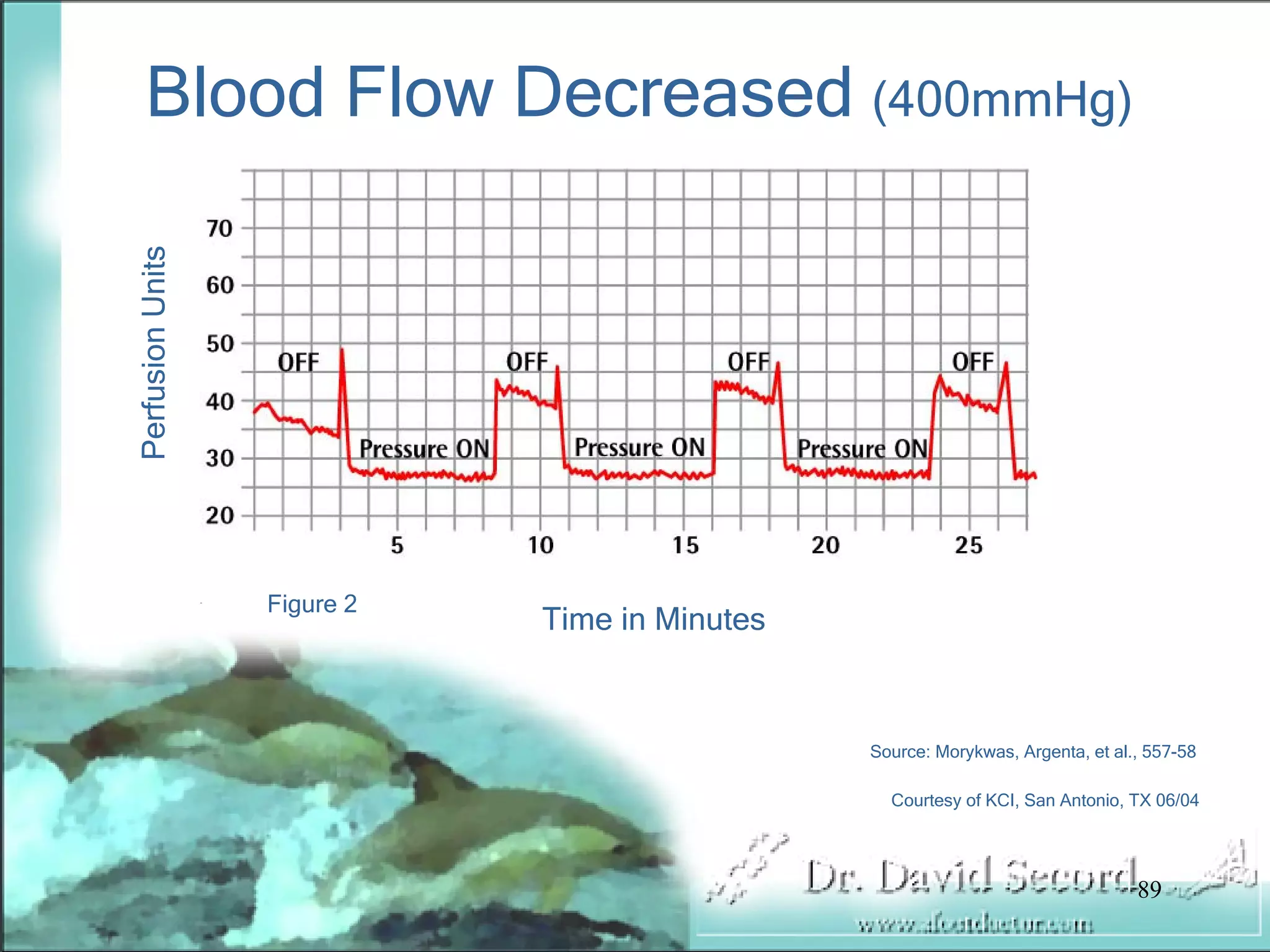
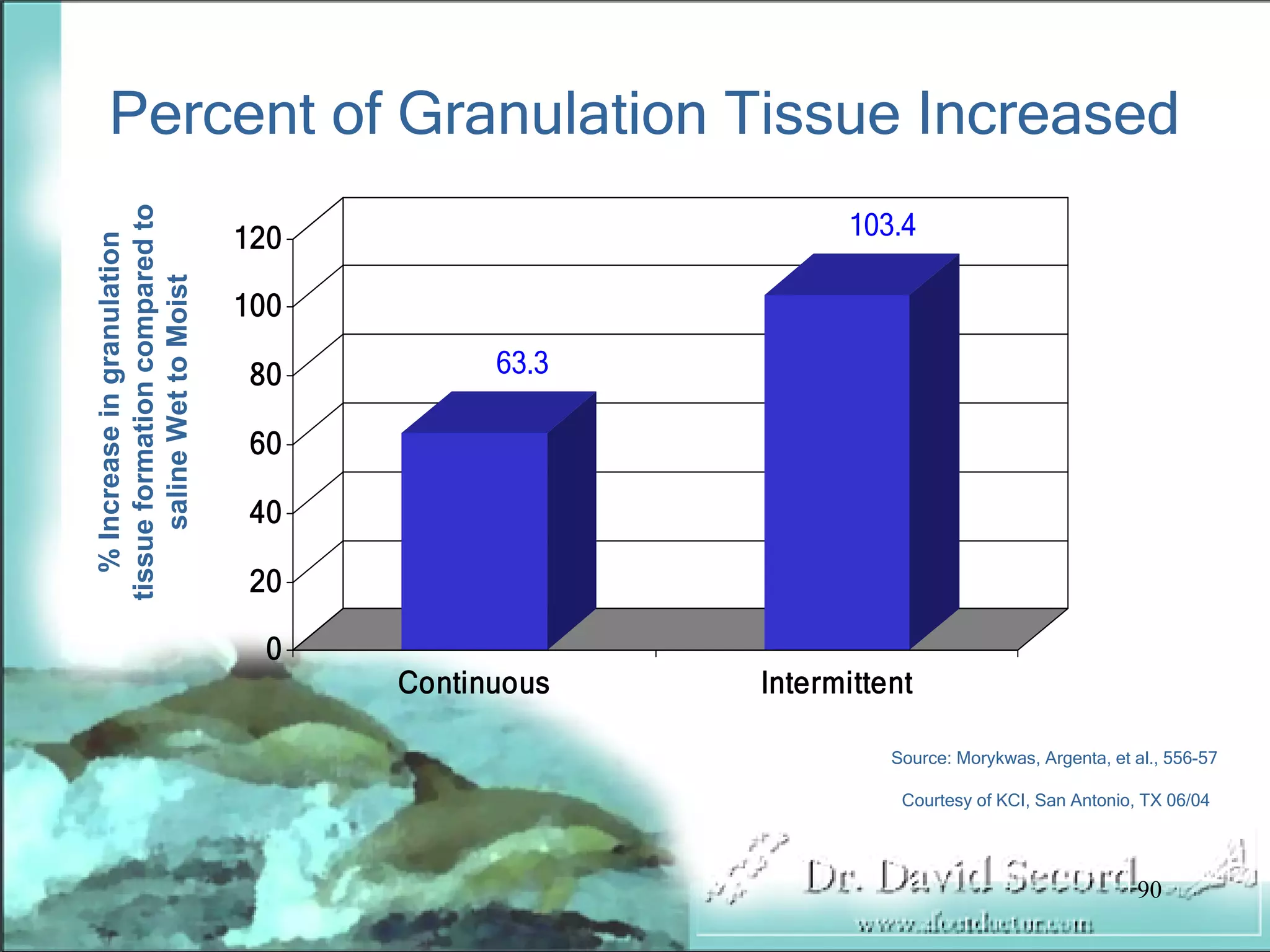
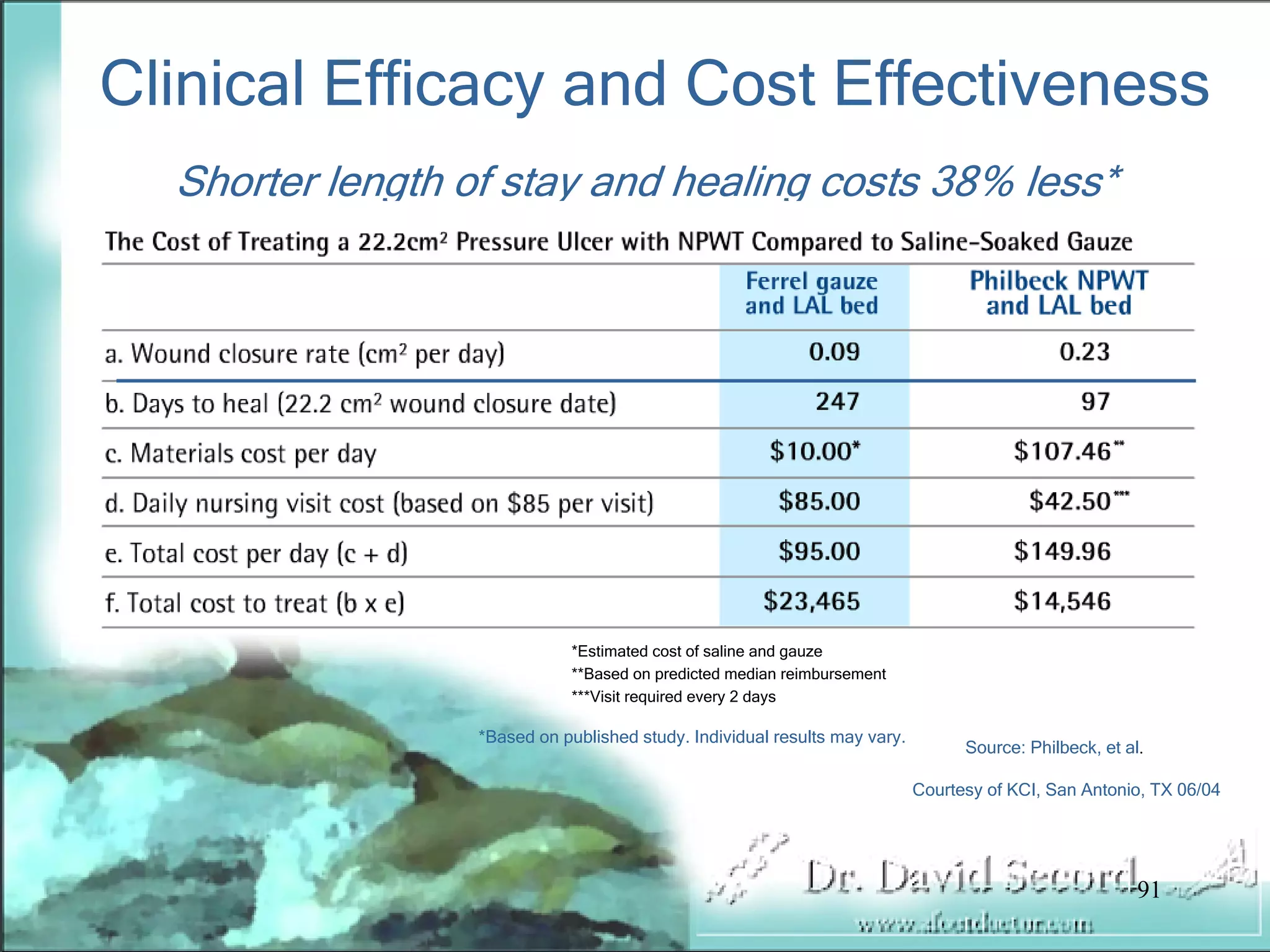
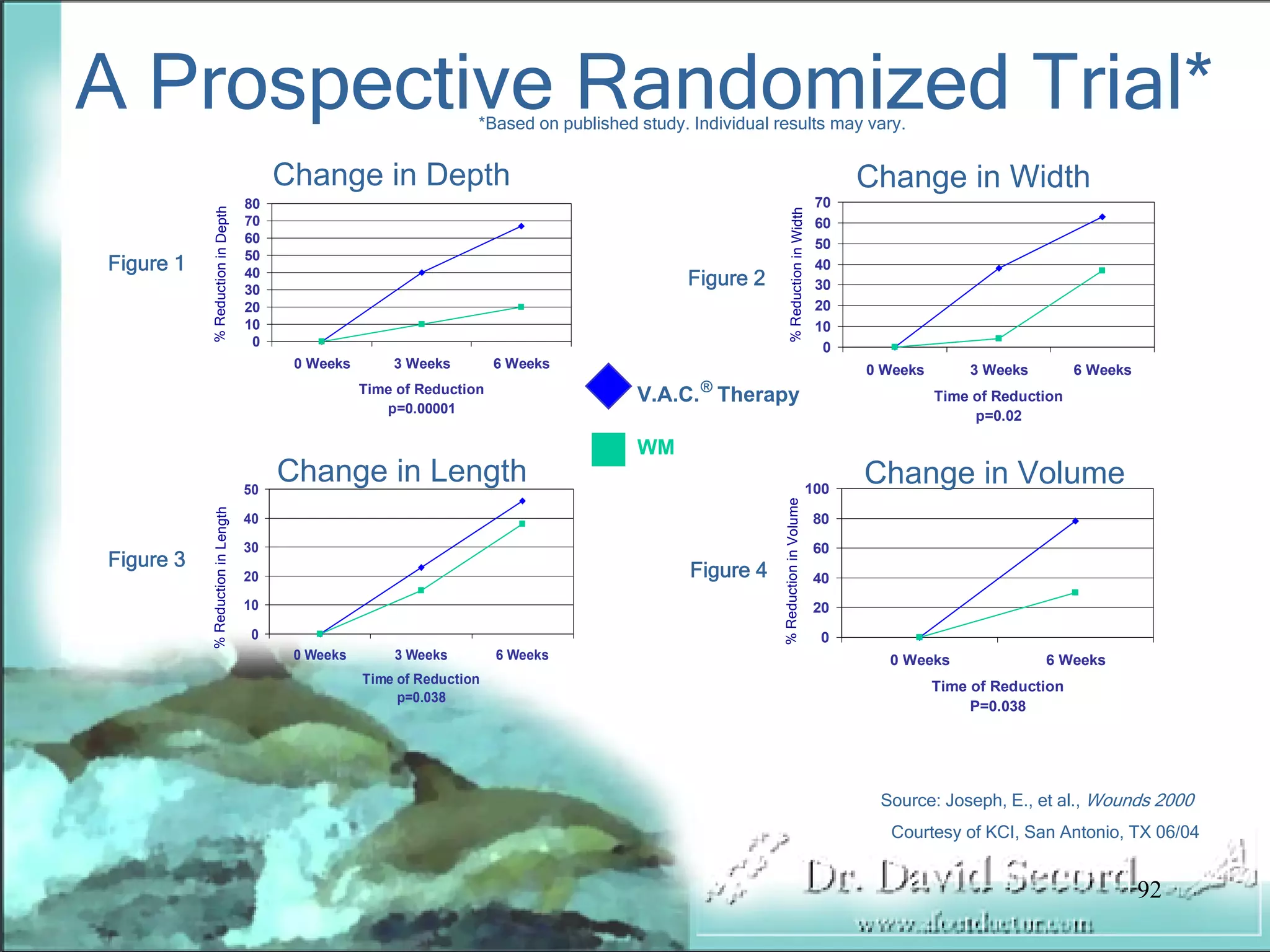
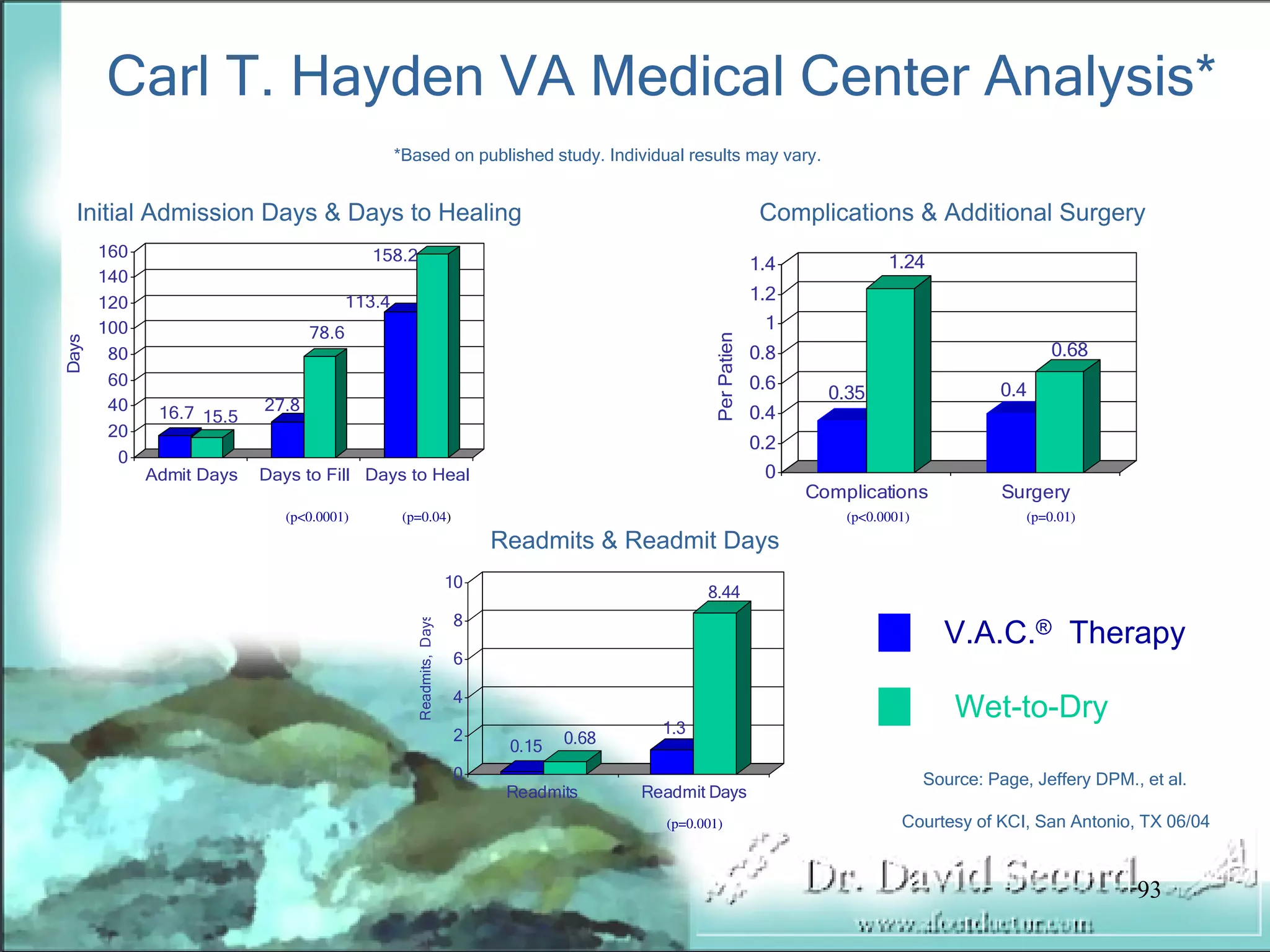
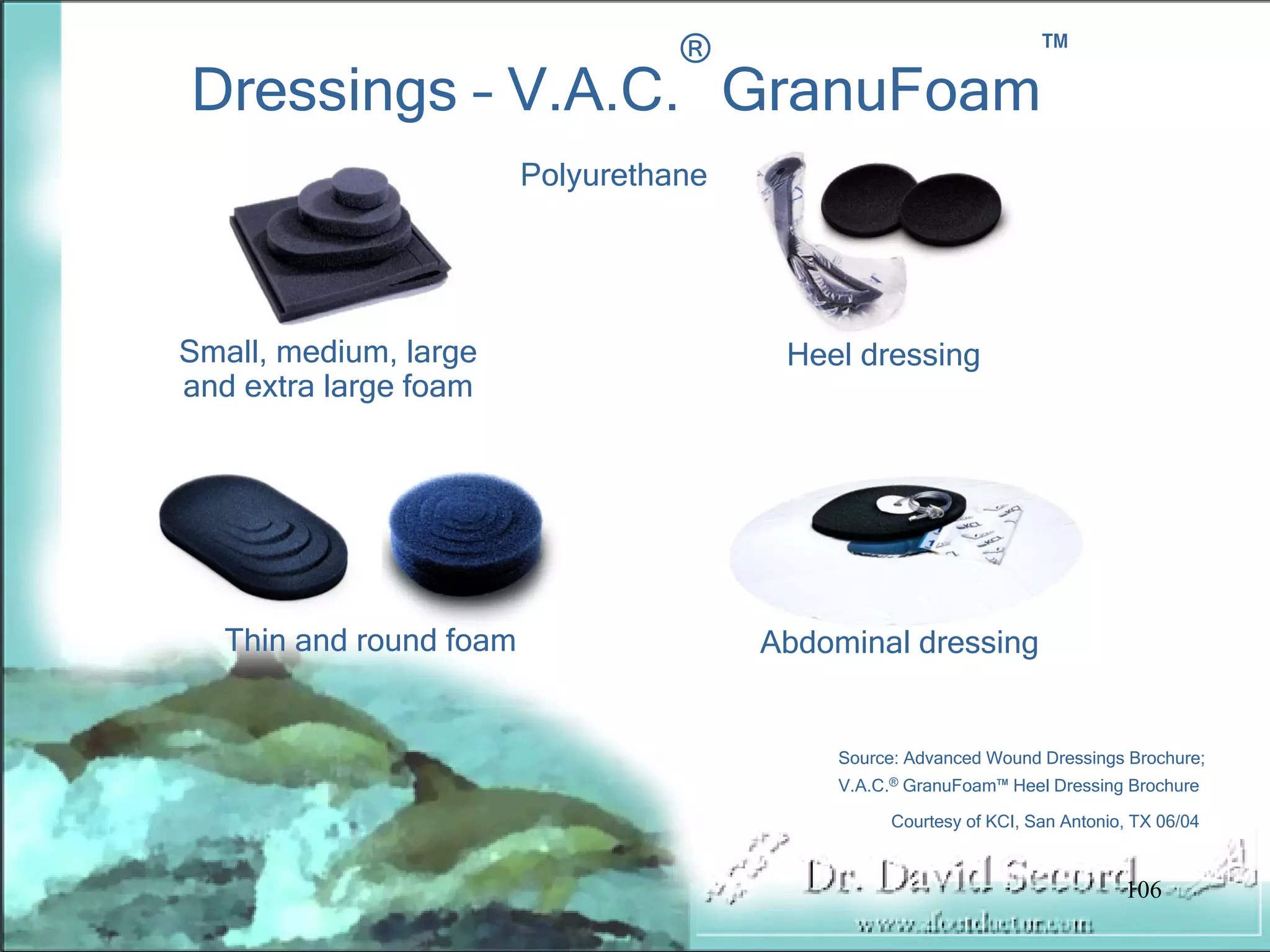
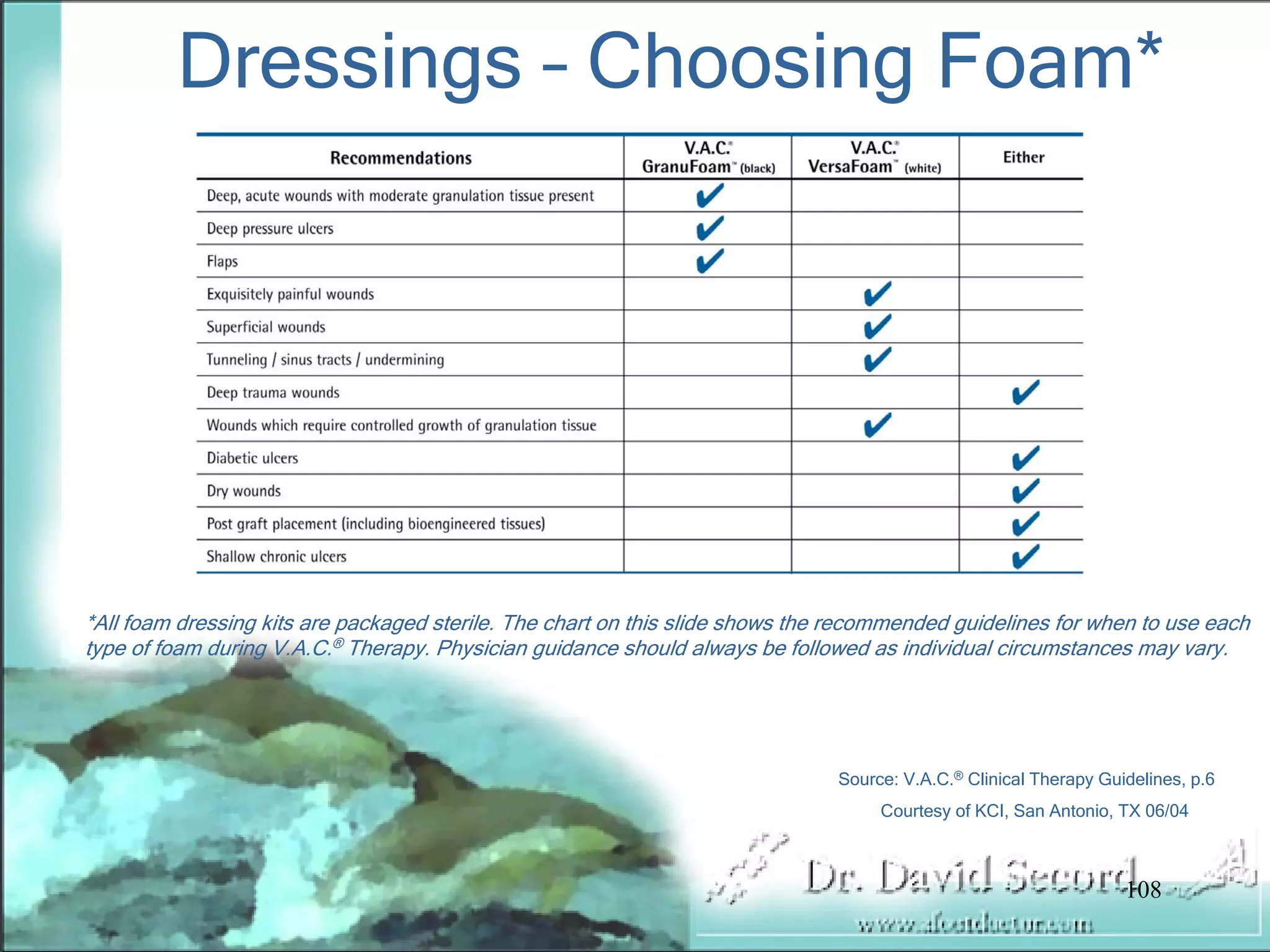
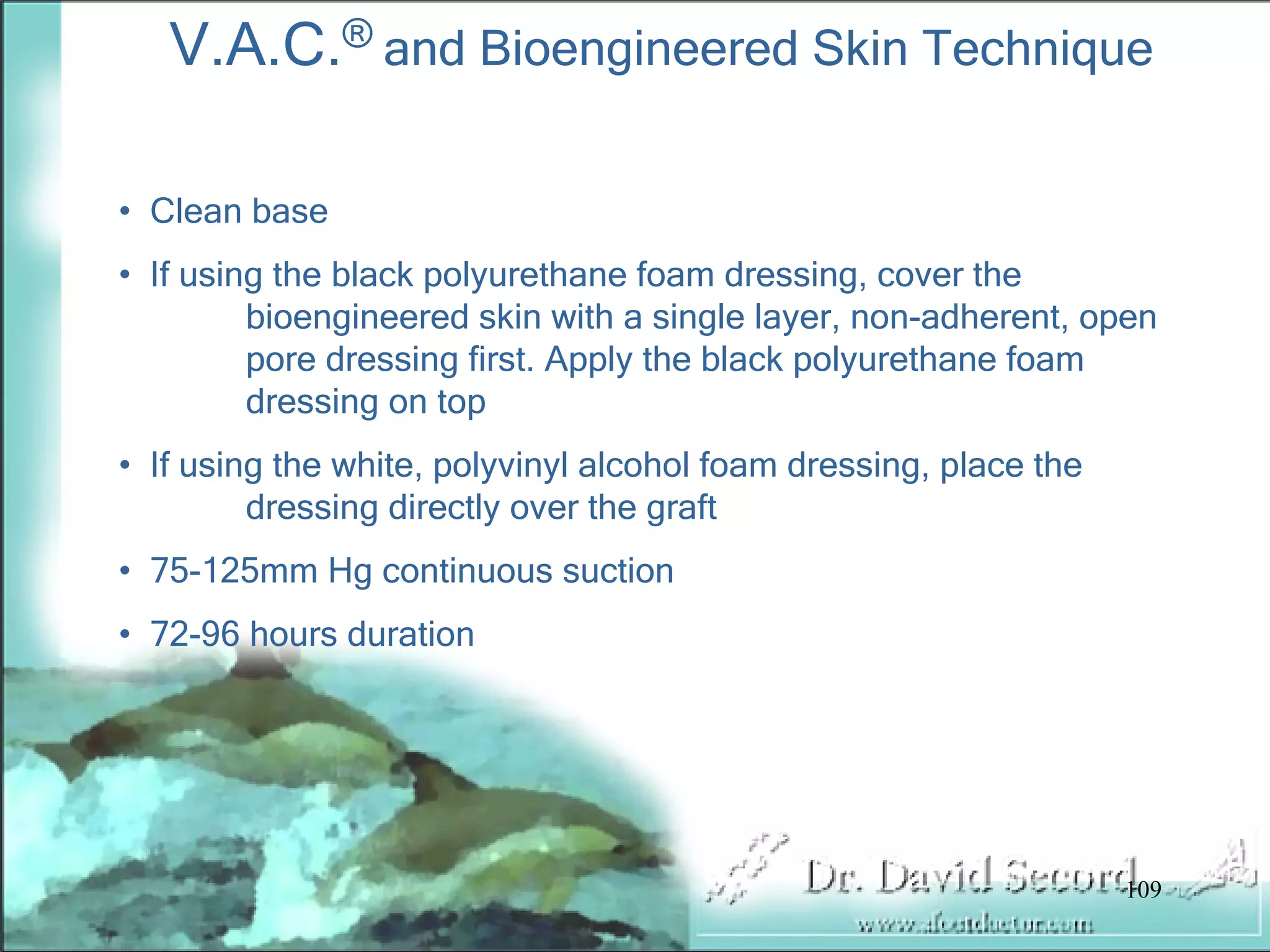
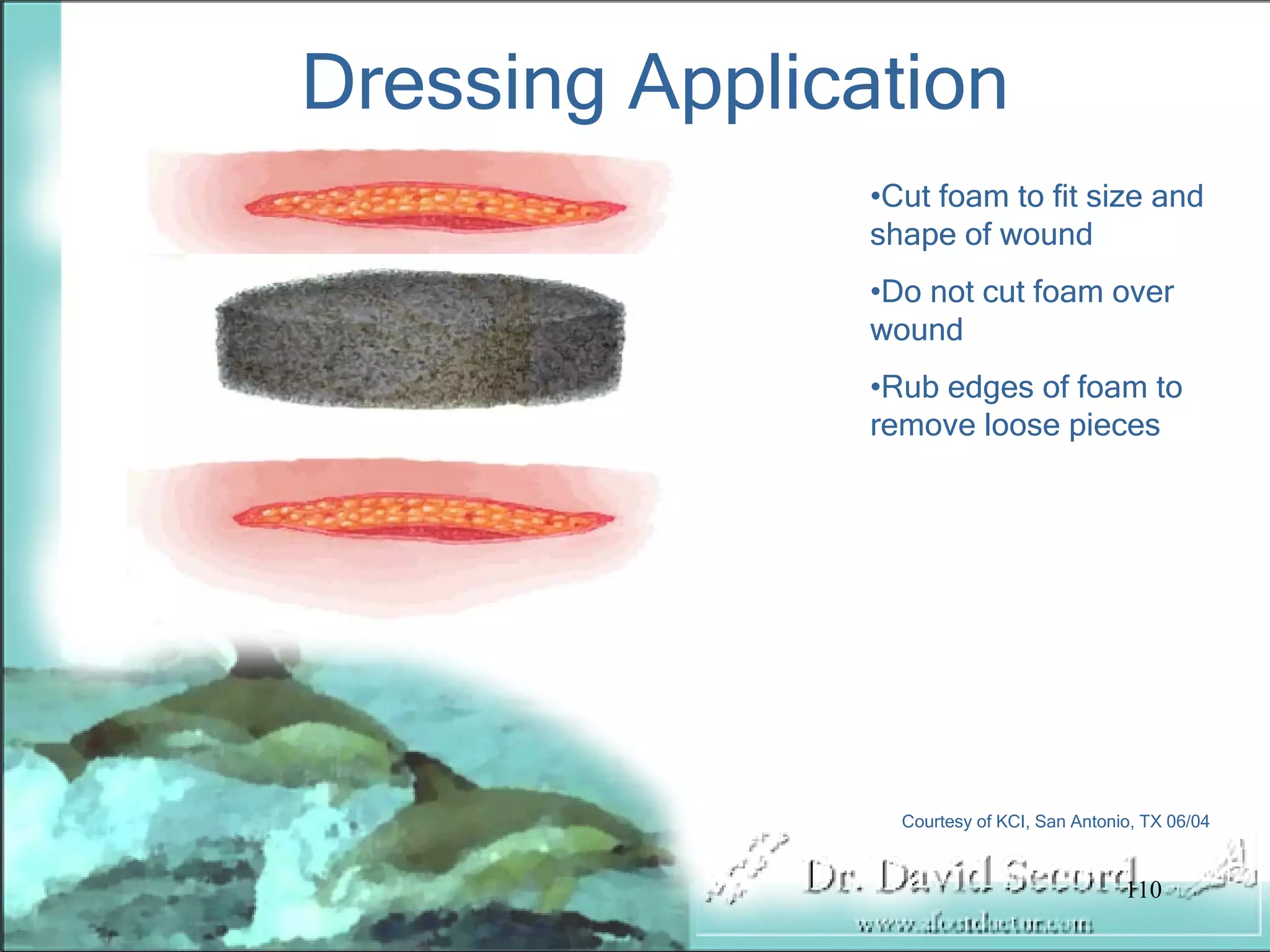
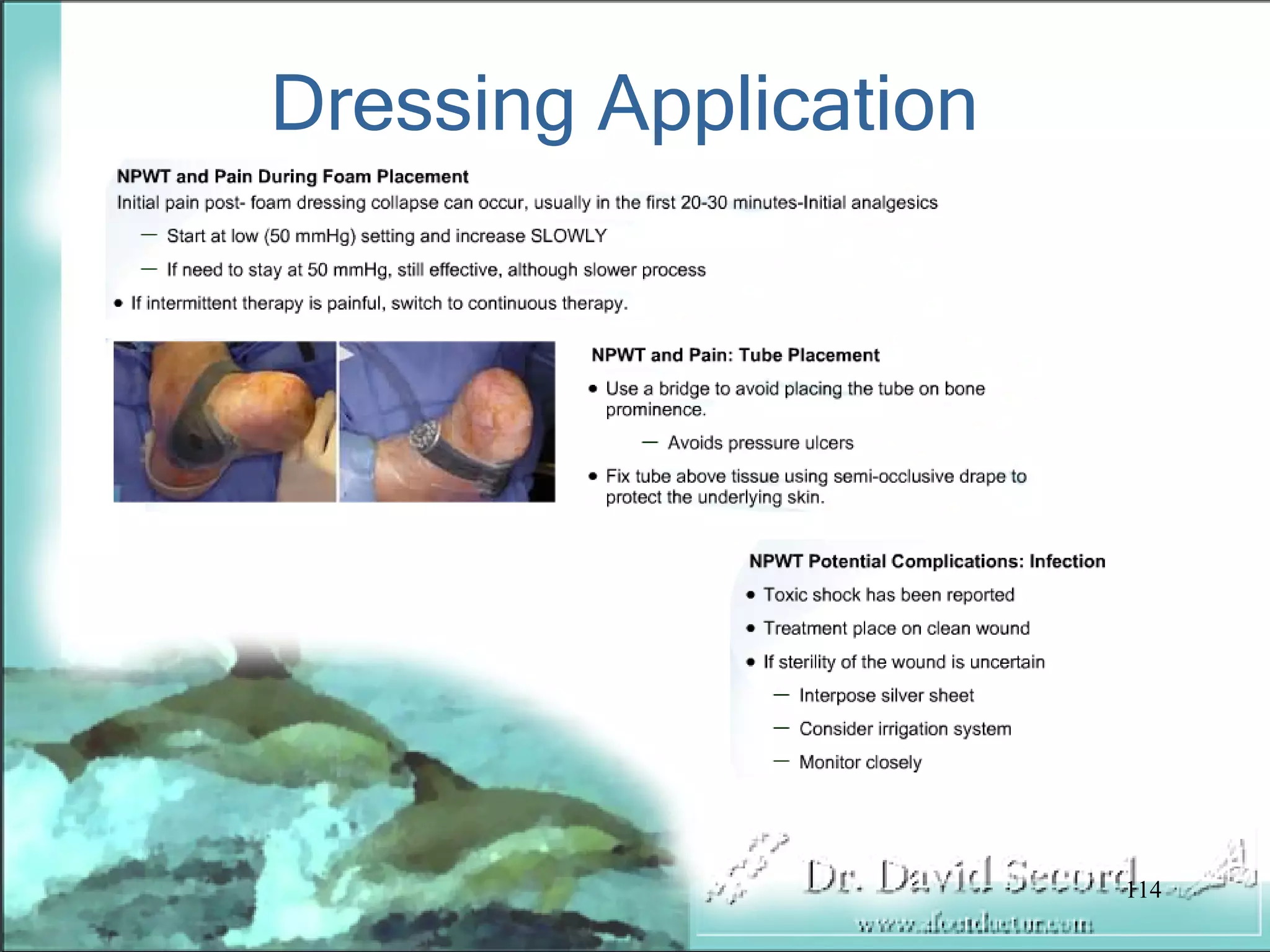
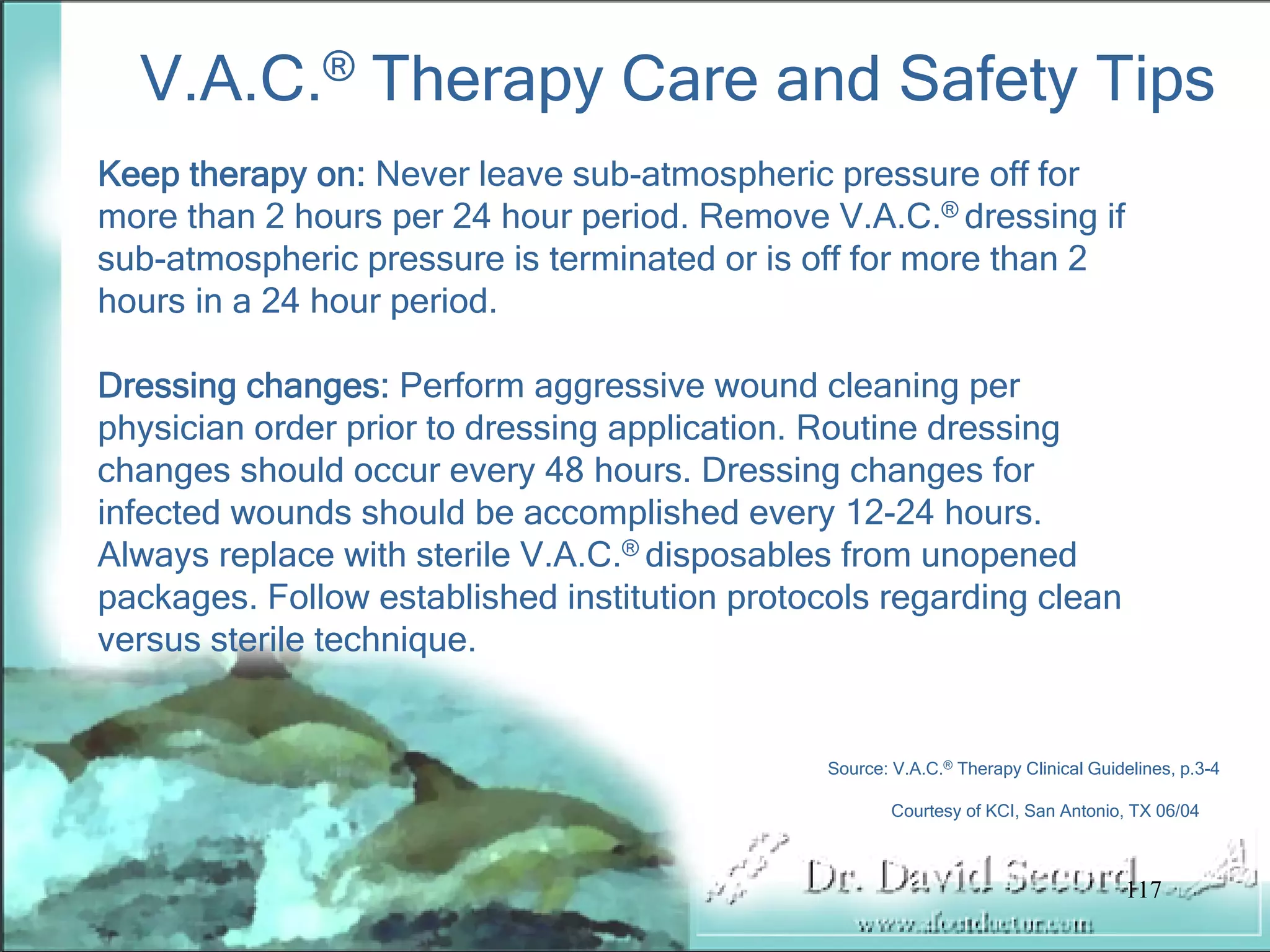
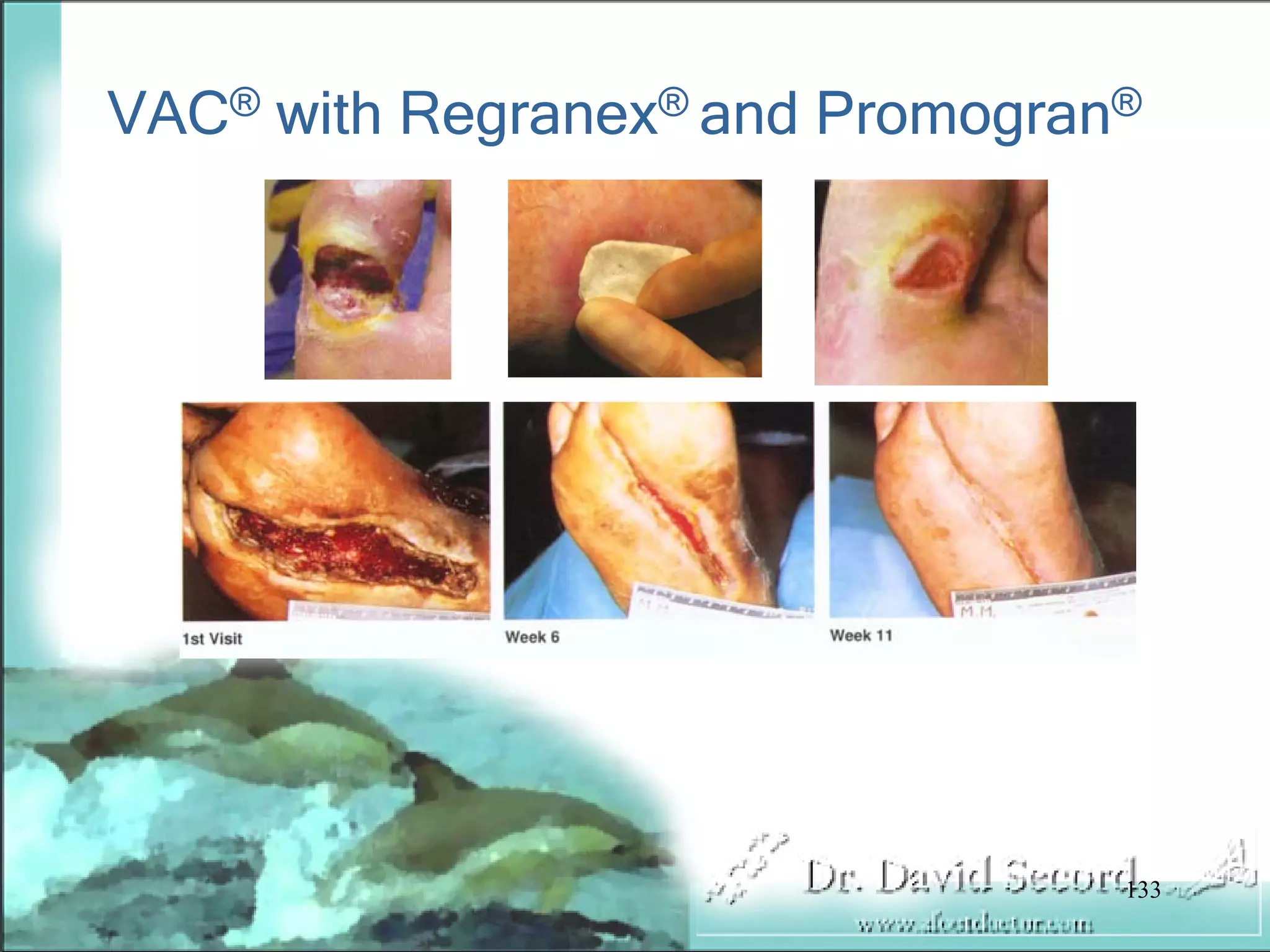
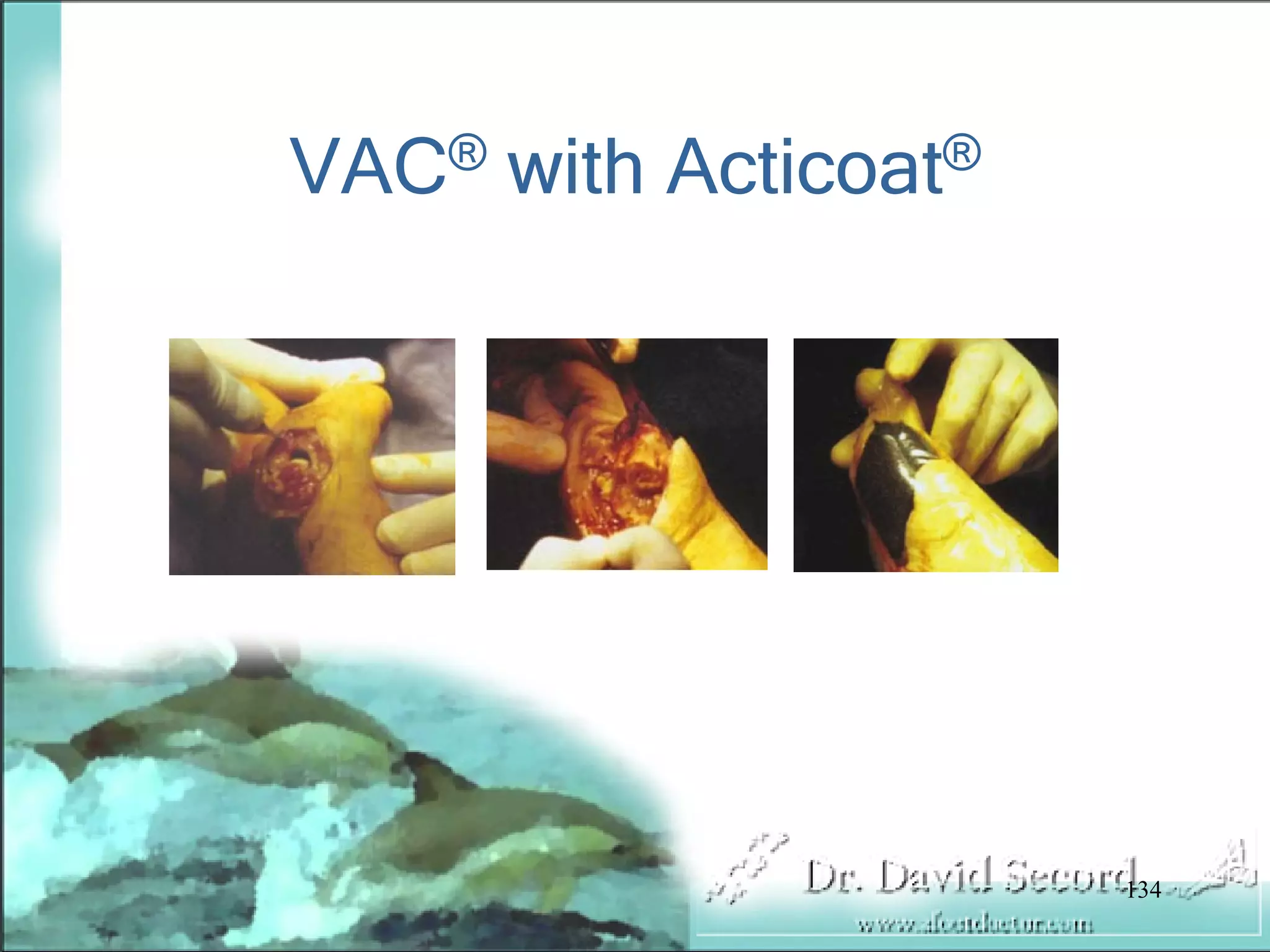
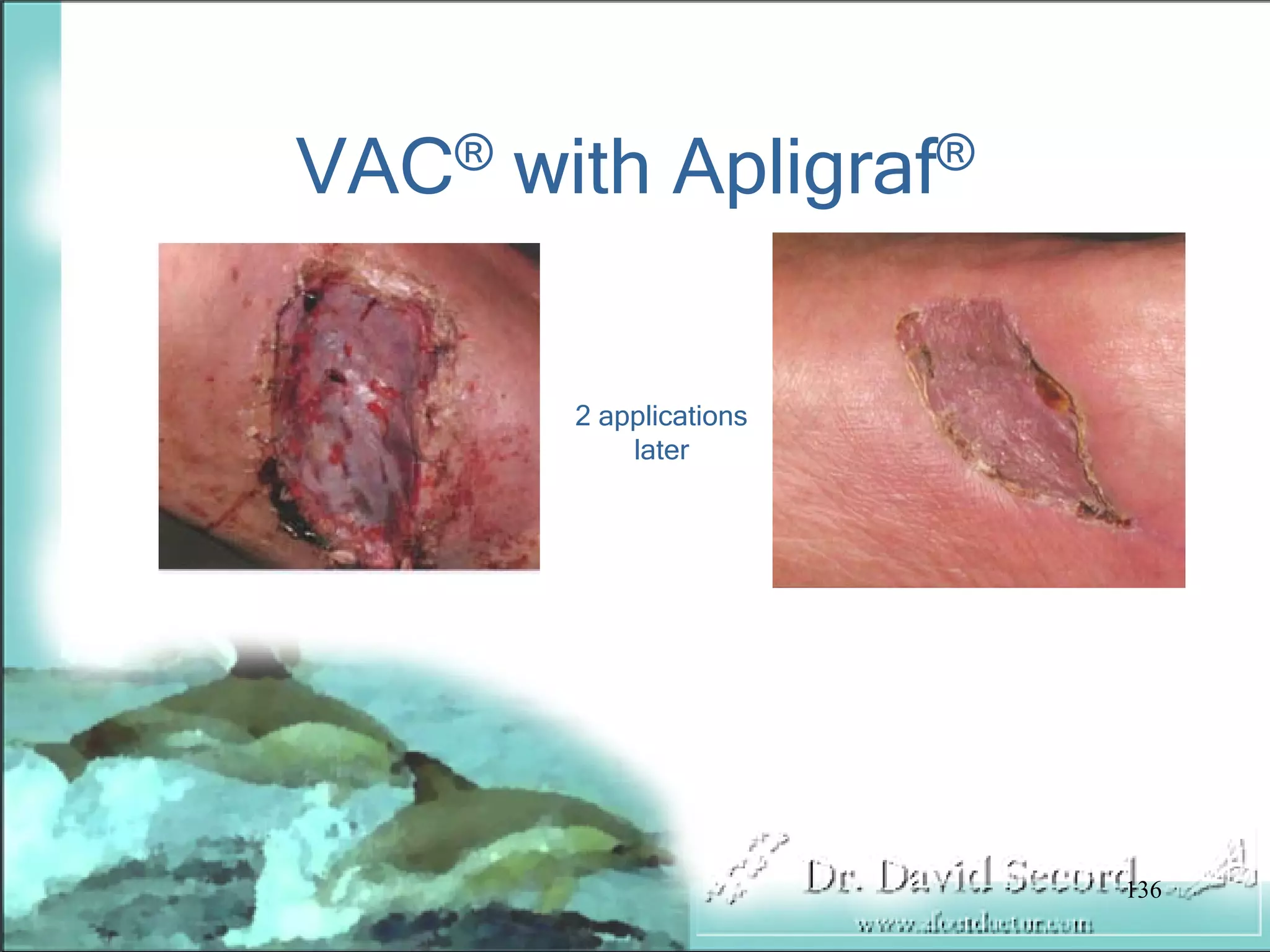
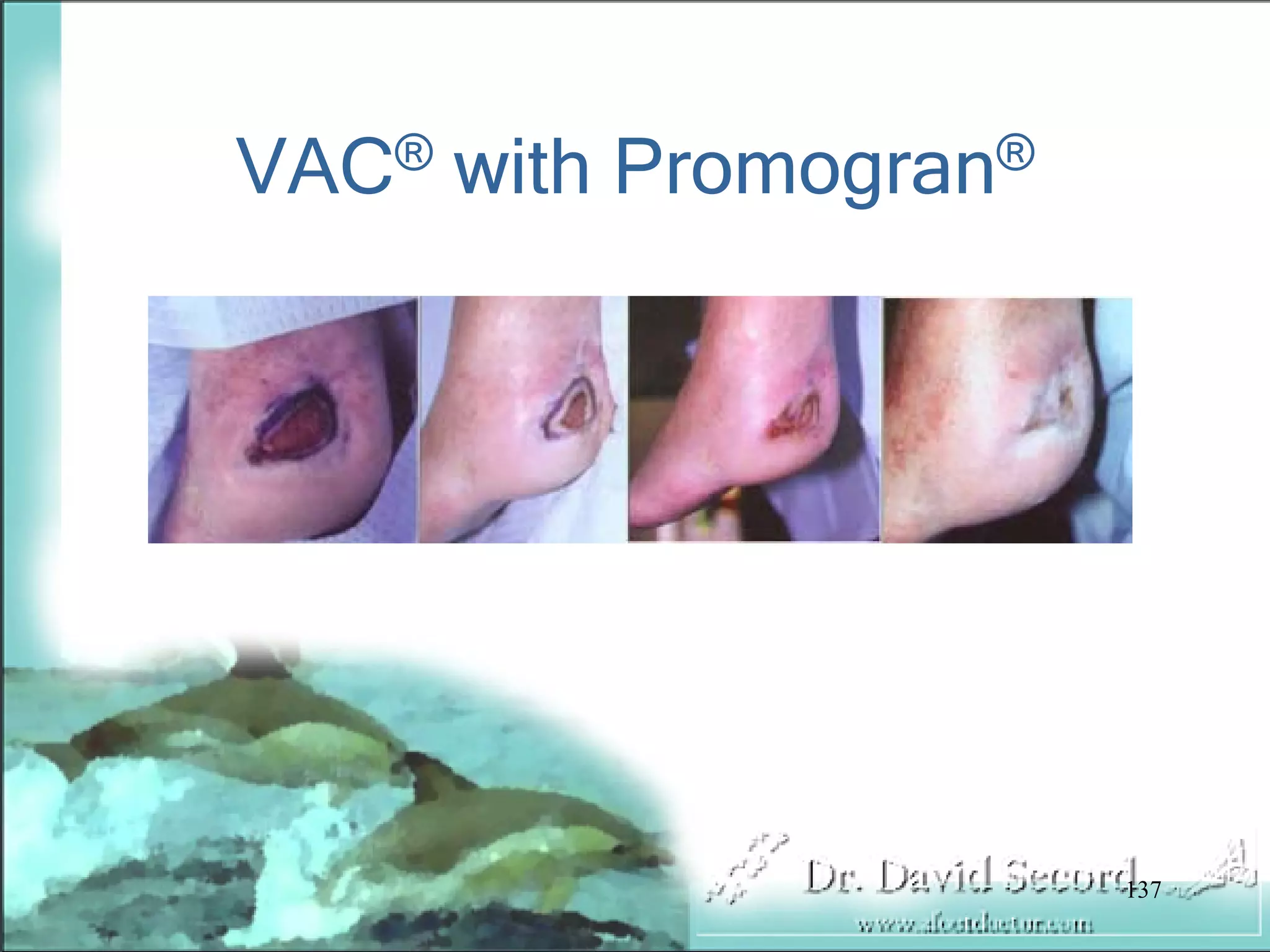
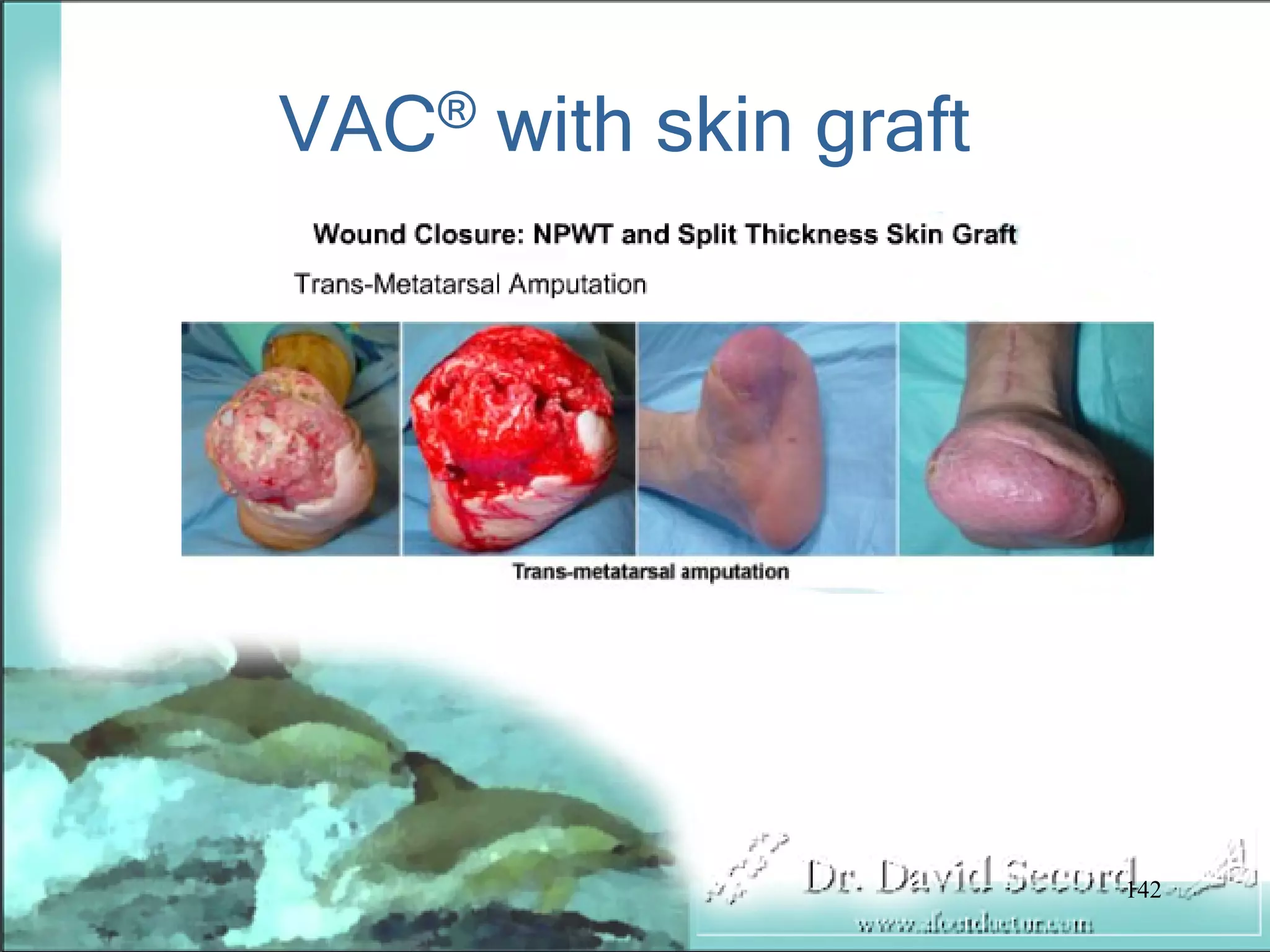
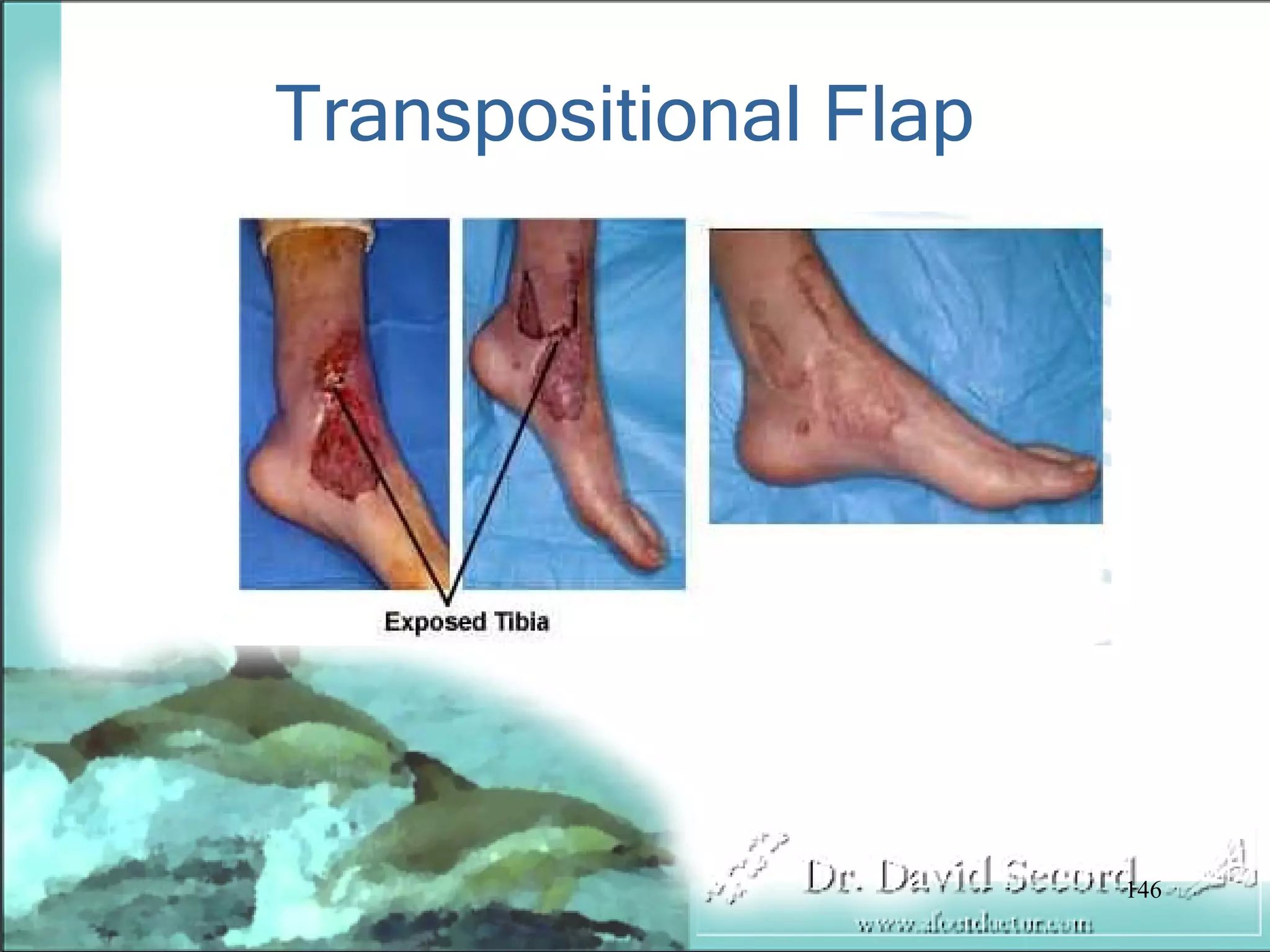
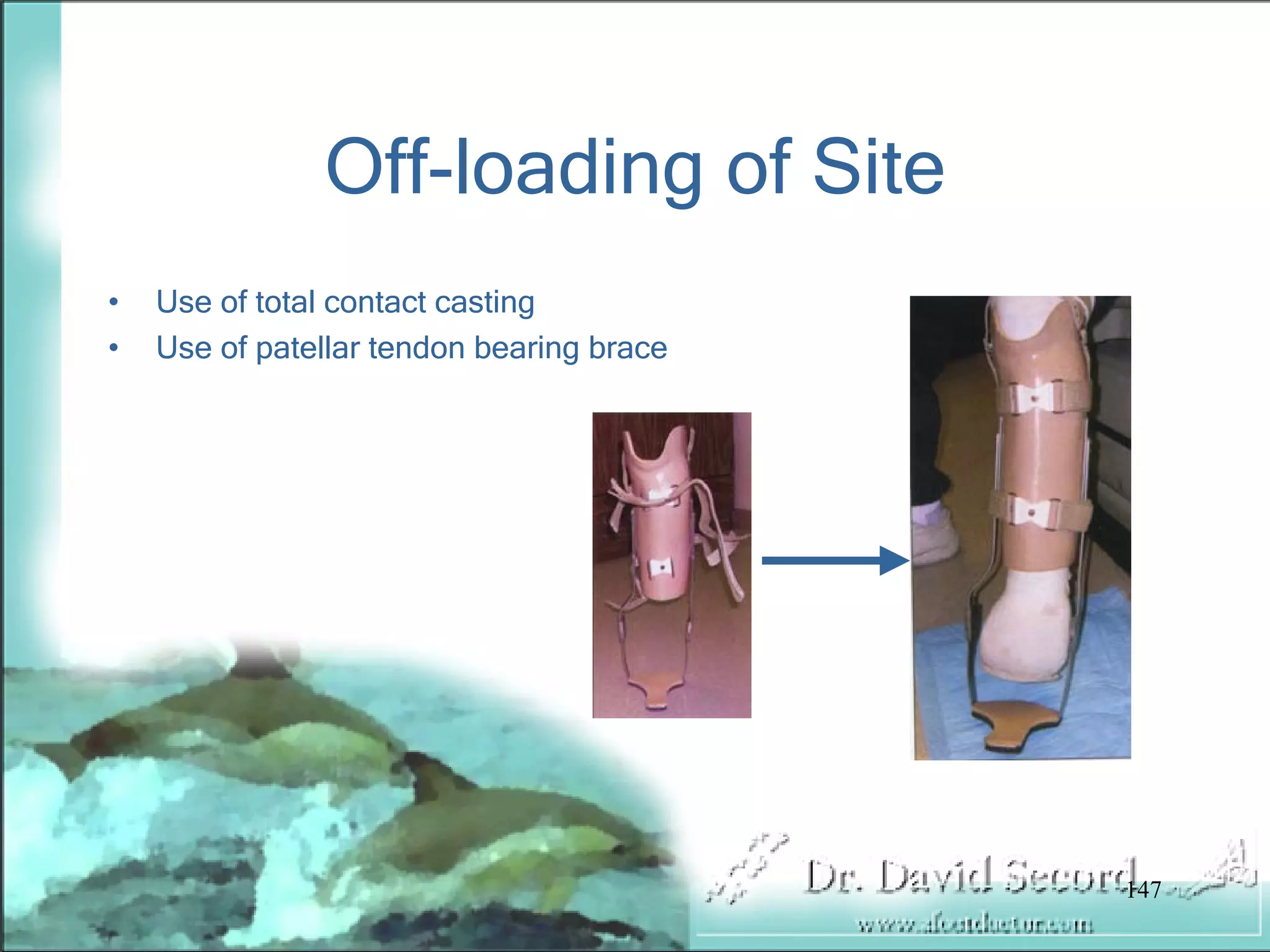
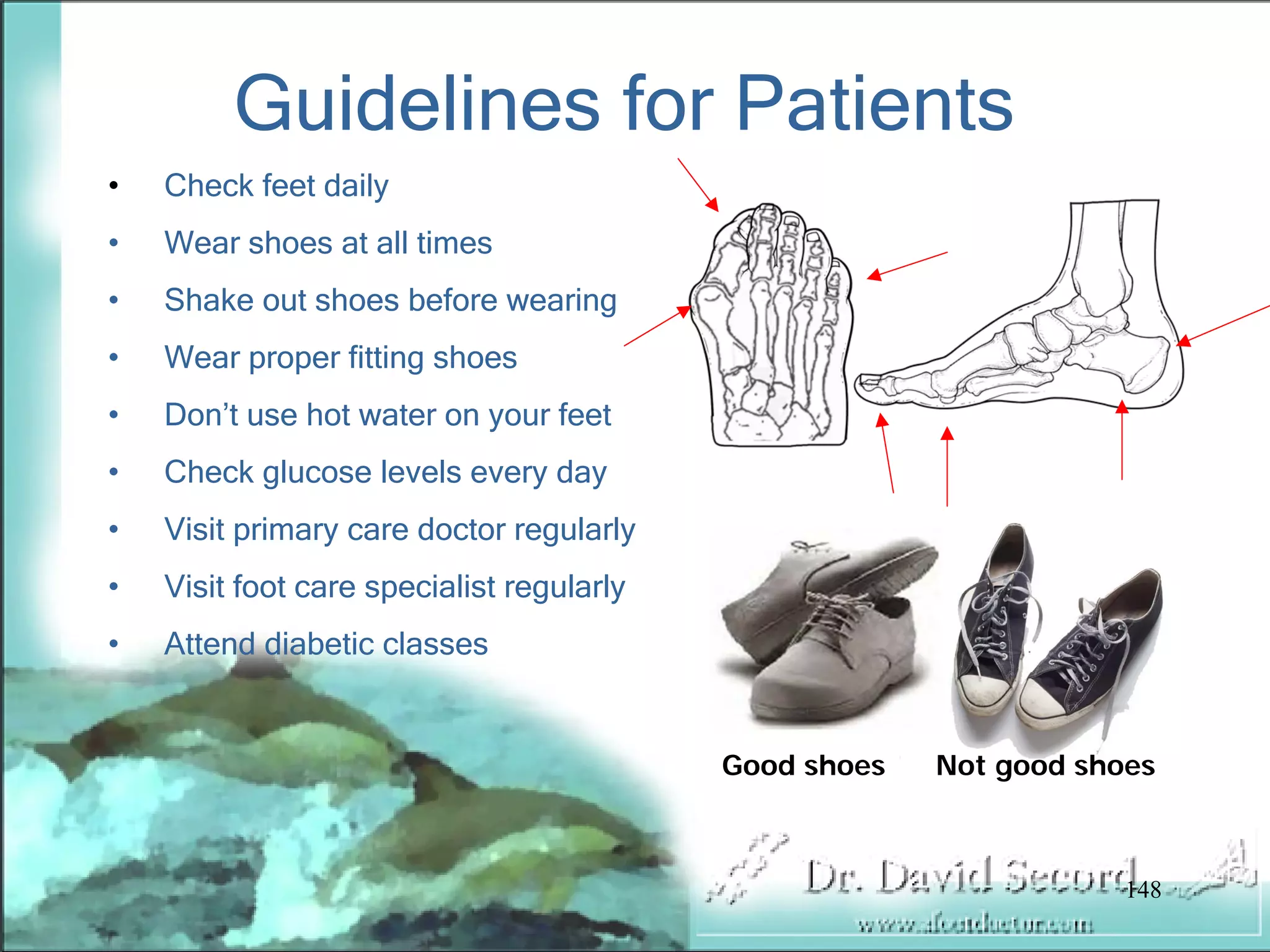
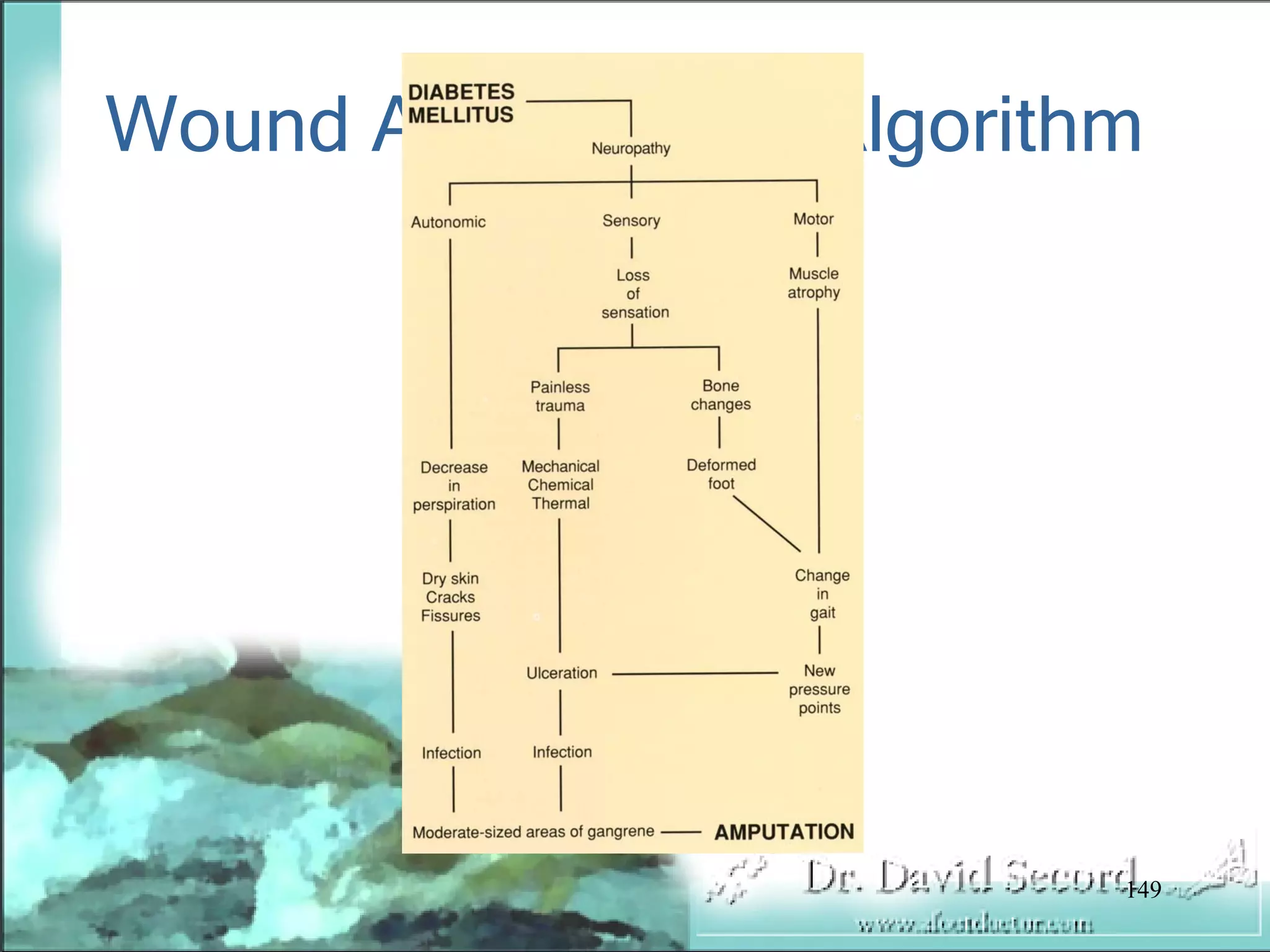
This document discusses diabetic wound management concepts and treatment. It notes that diabetes affects over 23 million Americans and costs over $100 billion annually to treat. Up to 51% of lower extremity amputations are due to diabetes. The document covers diabetic wound etiology such as neuropathy, immunopathy, and vasculopathy. It discusses testing, debridement, culture, grading scales, and the phases of wound healing. The goal of treatment is reducing further deformity and infection while retaining viable extremities through biomechanical and nutritional considerations.