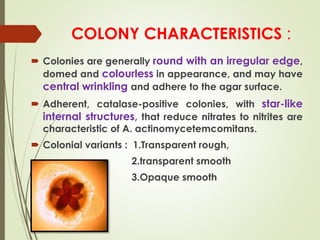
Aggregatibacter actinomycetemcomitans is a gram-negative bacterium that is considered a primary pathogen in aggressive periodontitis. It produces several virulence factors that allow it to evade the host immune response and cause tissue destruction, such as a leukotoxin that lyses leukocytes, a cytolethal distending toxin that induces cell cycle arrest, and lipopolysaccharide that stimulates inflammation. The bacterium attaches to surfaces using fimbriae and establishes itself in the oral cavity through interactions with other microorganisms and host factors before going on to cause periodontal disease.