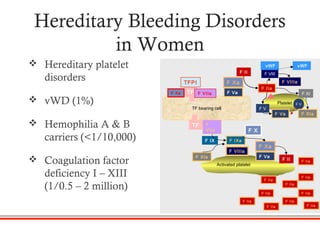
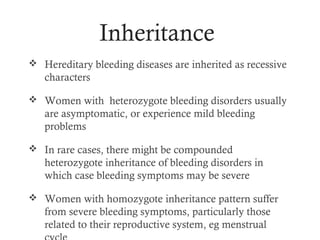
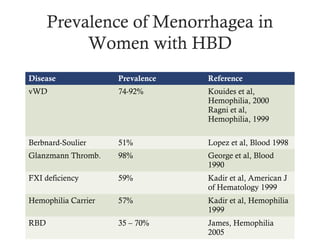
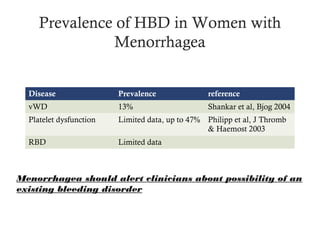
1) Hereditary bleeding disorders can cause health problems in women, especially related to their reproductive systems like menorrhagia, dysmenorrhea, and hemorrhagic ovarian cysts.
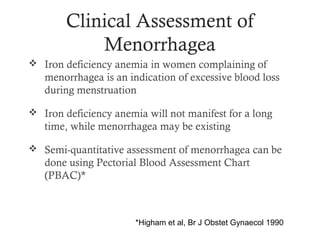
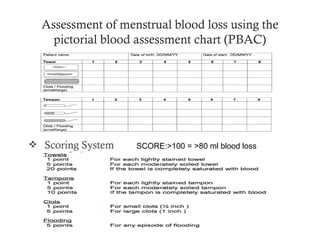
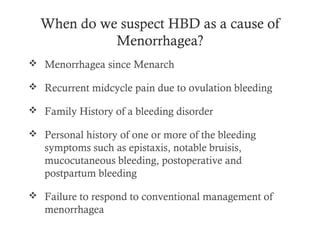
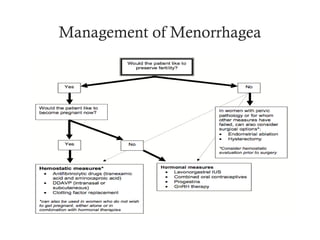
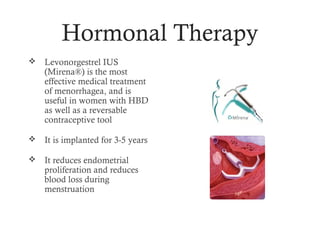
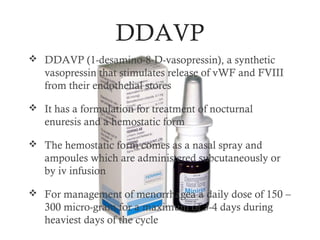
2) Menorrhagia, or prolonged/heavy menstrual bleeding, is common in women with von Willebrand disease, platelet disorders, and other bleeding disorders. It can be assessed and managed through hormonal therapy, hemostatic agents, blood transfusions, or surgery depending on the severity.
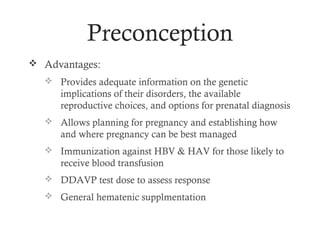
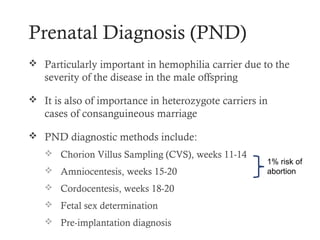
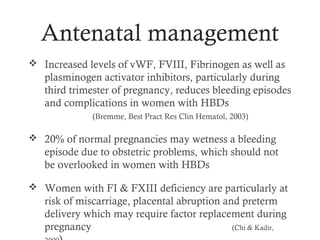
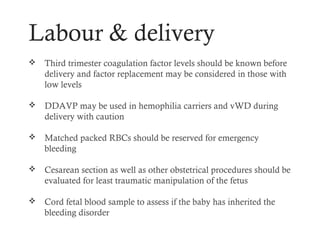
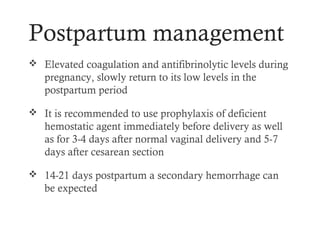
3) Preconception counseling is important to discuss issues like genetic implications, pregnancy and delivery risks, and options for prenatal screening or testing. Proper management can help women with bleeding disorders have healthy pregn