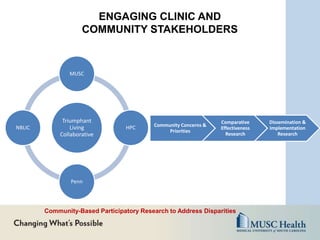
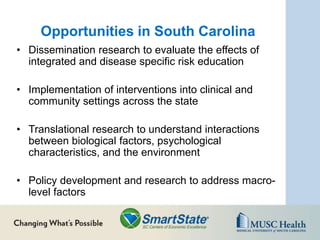
The SmartState Center for Cancer Equity at the Medical University of South Carolina aims to reduce cancer disparities through four main strategies: 1) enhancing minority participation in clinical research on health promotion and disease prevention; 2) increasing access to emerging technologies for these purposes; 3) developing culturally-tailored interventions to improve health outcomes; and 4) establishing infrastructure for promotion and prevention efforts in clinical and community settings. The Center directs comparative effectiveness trials, dissemination/implementation research, and community-engaged studies to address cancer inequities.