The document provides an orientation for newborn nurses, covering several key areas:
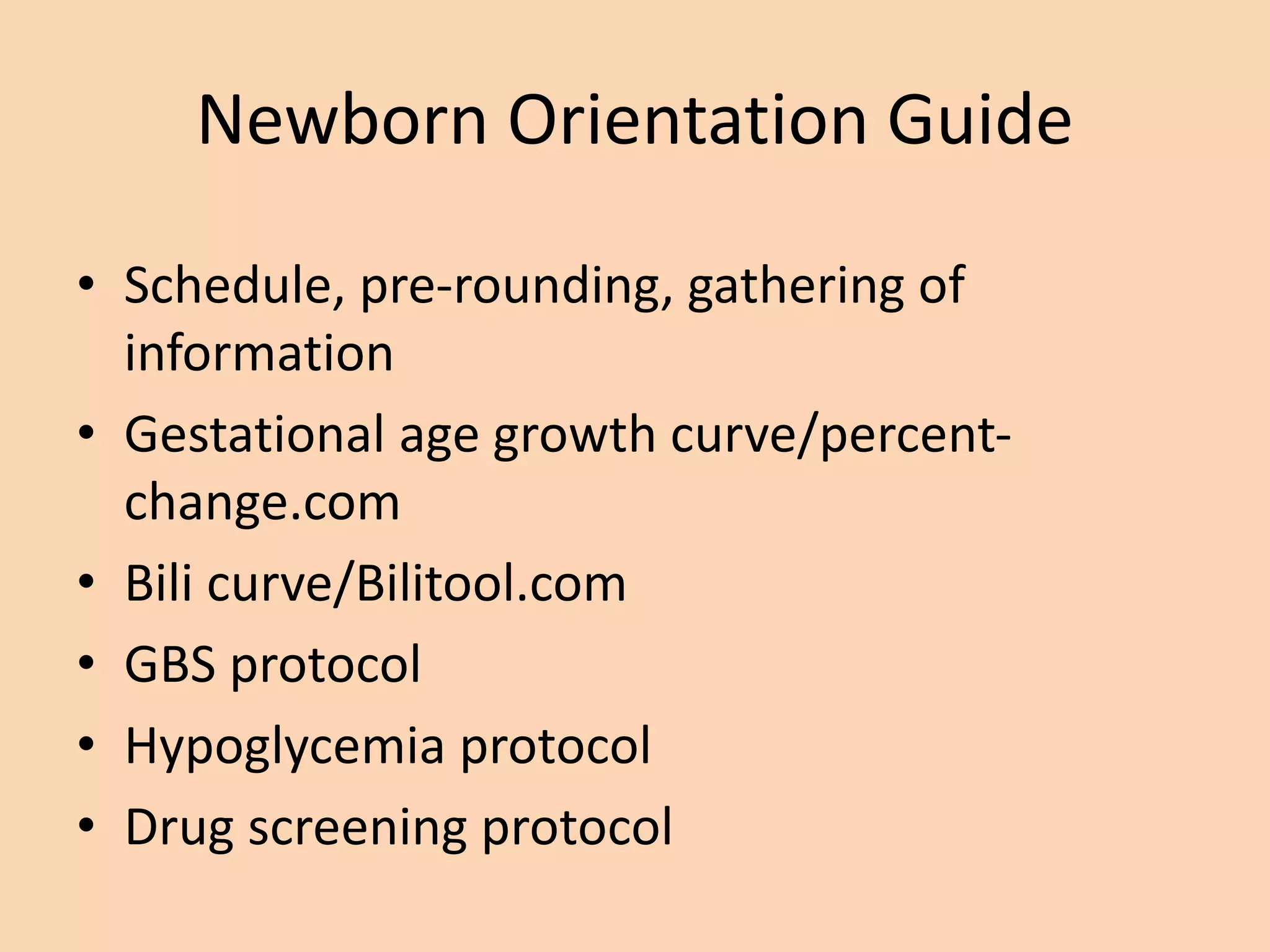
1) Recognizing important maternal and delivery factors that may affect the newborn and developing skills to examine newborns and assess gestational age.
2) Learning about routine newborn care including infection control, feeding, parenting advice, and recognizing psychosocial factors.
3) Understanding protocols for conditions like hypoglycemia, jaundice, and drug screening and when to utilize them.





![PRESENTATION
Keep it Simple [KISS Principle]
• Questions/Concerns without answers
–Yours and theirs
–Have a positive definitive plan
–Follow thru at expected time re: hyper-
concerns of the new parents.
• Don’t share your concerns unless there is
a definitive plan
"Happy Crisis by W. Brown](https://image.slidesharecdn.com/welcometothenewbornnurseryjune2013-1-230223040110-20d25d53/75/Welcome-to-the-Newborn-Nursery-7-2048.jpg)













