1. Pharmacological prophylaxis such as unfractionated heparin or lower molecular weight heparin should be initiated within 24 hours for ICU patients to prevent venous thromboembolism, unless contraindicated due to bleeding risk.
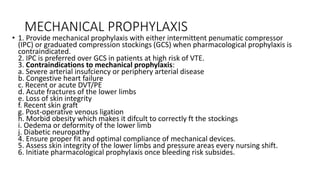
2. Mechanical prophylaxis with intermittent pneumatic compression or graduated compression stockings is recommended when pharmacological prophylaxis cannot be used due to bleeding risk.
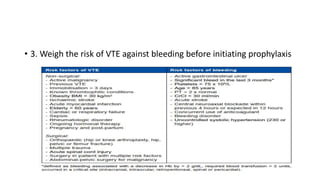
3. The risk of VTE and bleeding should be reassessed daily and prophylaxis adjusted or discontinued based on the patient's condition and mobility.