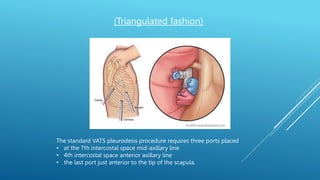
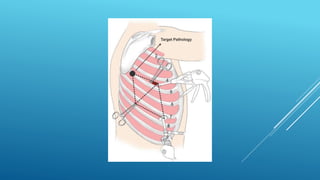
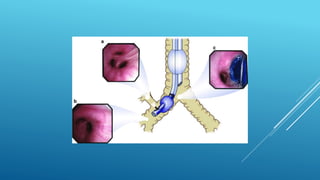
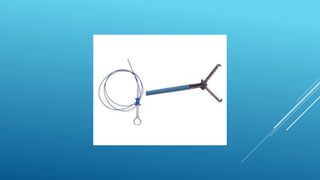
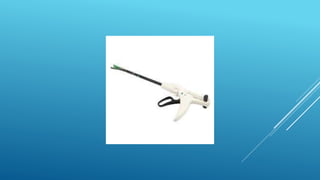
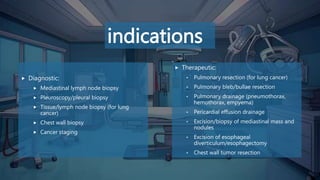
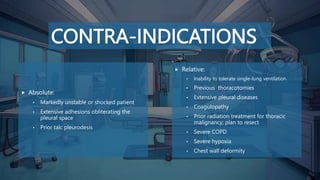
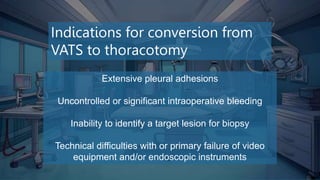
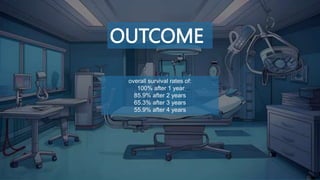
Video-assisted thoracic surgery (VATS) is a minimally invasive technique used for thoracic conditions, providing benefits such as reduced postoperative morbidity and quicker recovery times. The procedure employs specific ports for instrumentation and is indicated for both diagnostic and therapeutic purposes, while contraindications and potential complications must be carefully considered. Overall survival rates post-surgery are high, with 100% after one year and gradually decreasing over subsequent years.