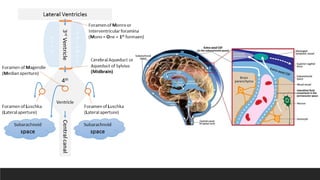
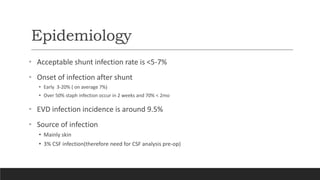
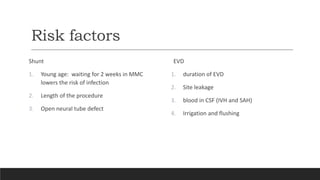
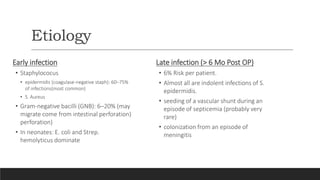
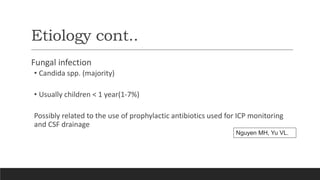
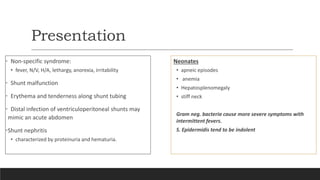
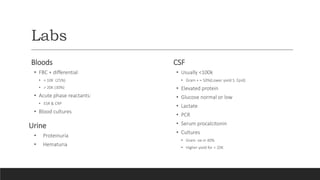
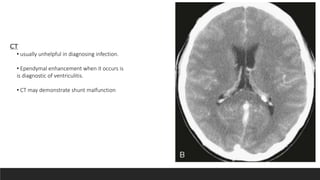
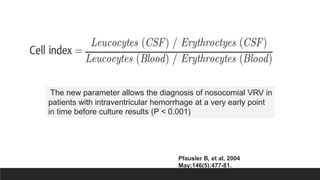
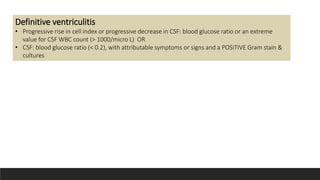
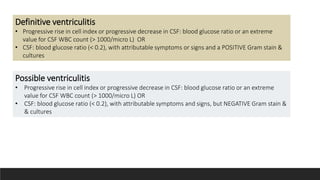
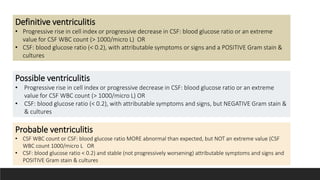
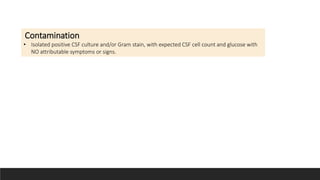
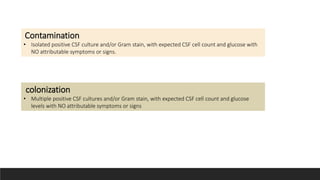
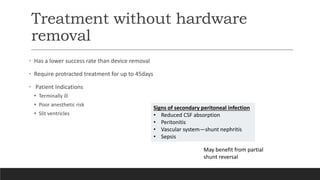
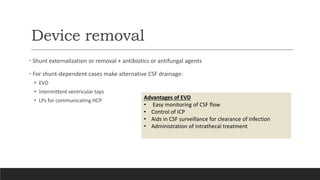
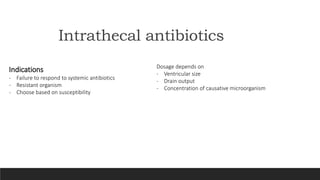
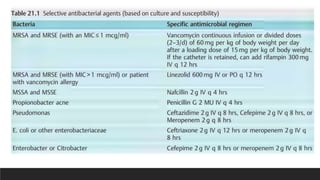
Ventriculitis is an inflammation of the ependymal lining of the cerebral ventricles that is usually secondary to infection from meningitis, devices, or trauma. It presents with non-specific symptoms like fever and headache. Diagnosis involves analysis of CSF showing elevated white blood cells and proteins with normal or low glucose. Management includes high dose intravenous antibiotics, removal of any devices, and monitoring of CSF parameters until infection clears. Outcomes are better when the infecting organism has low virulence and treatment includes both antibiotics and device removal.