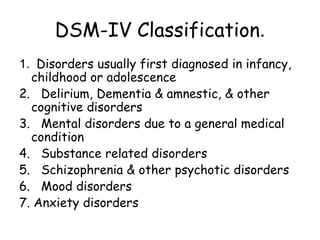
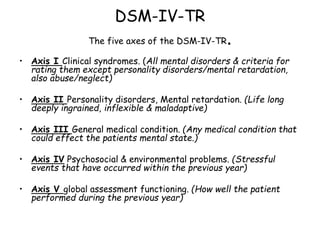
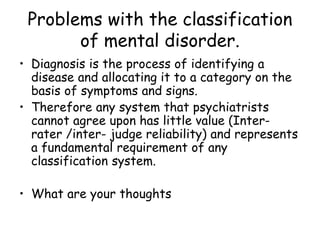
The classification of mental disorders has evolved over time based on the work of Kraepelin who originally classified disorders into two major groups: schizophrenia and manic-depressive psychosis. This helped establish mental disorders as organic conditions and formed the basis for diagnostic systems like the DSM and ICD. The DSM and ICD take different approaches in their classification but both aim to improve reliability through explicit diagnostic criteria. However, studies show poor reliability between psychiatrists due to subjective interpretation of information and cultural differences in diagnosis.