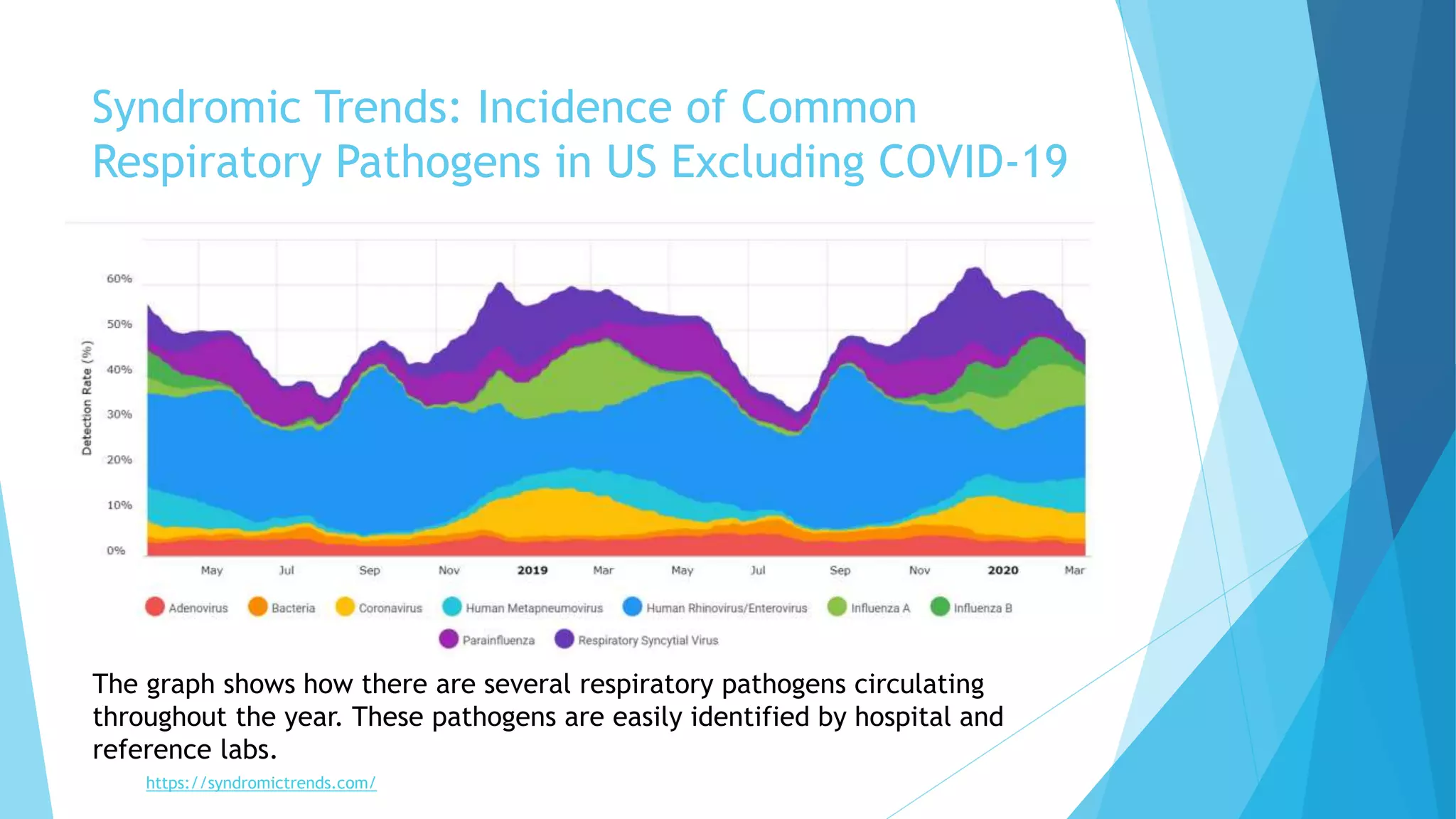
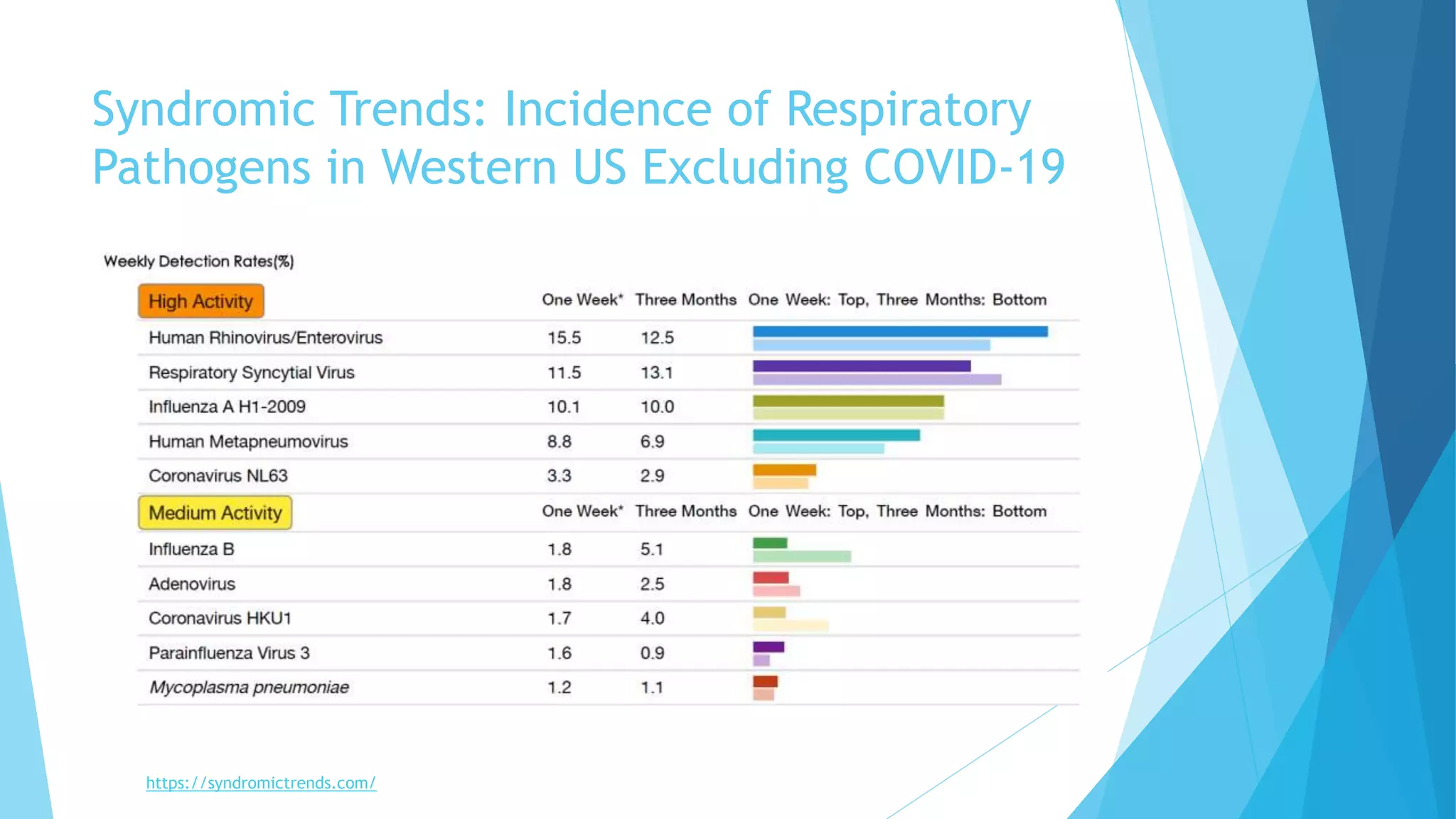
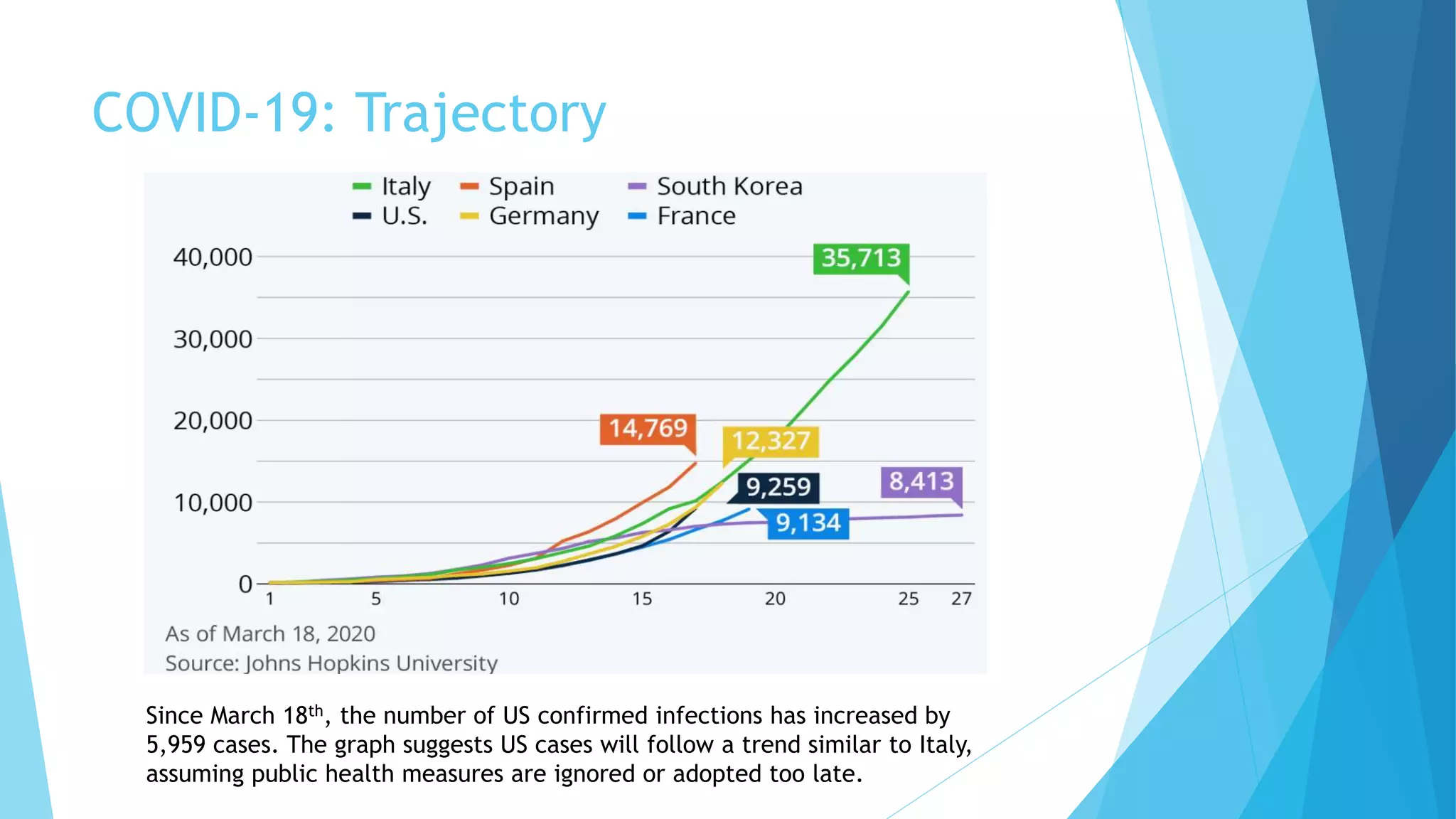
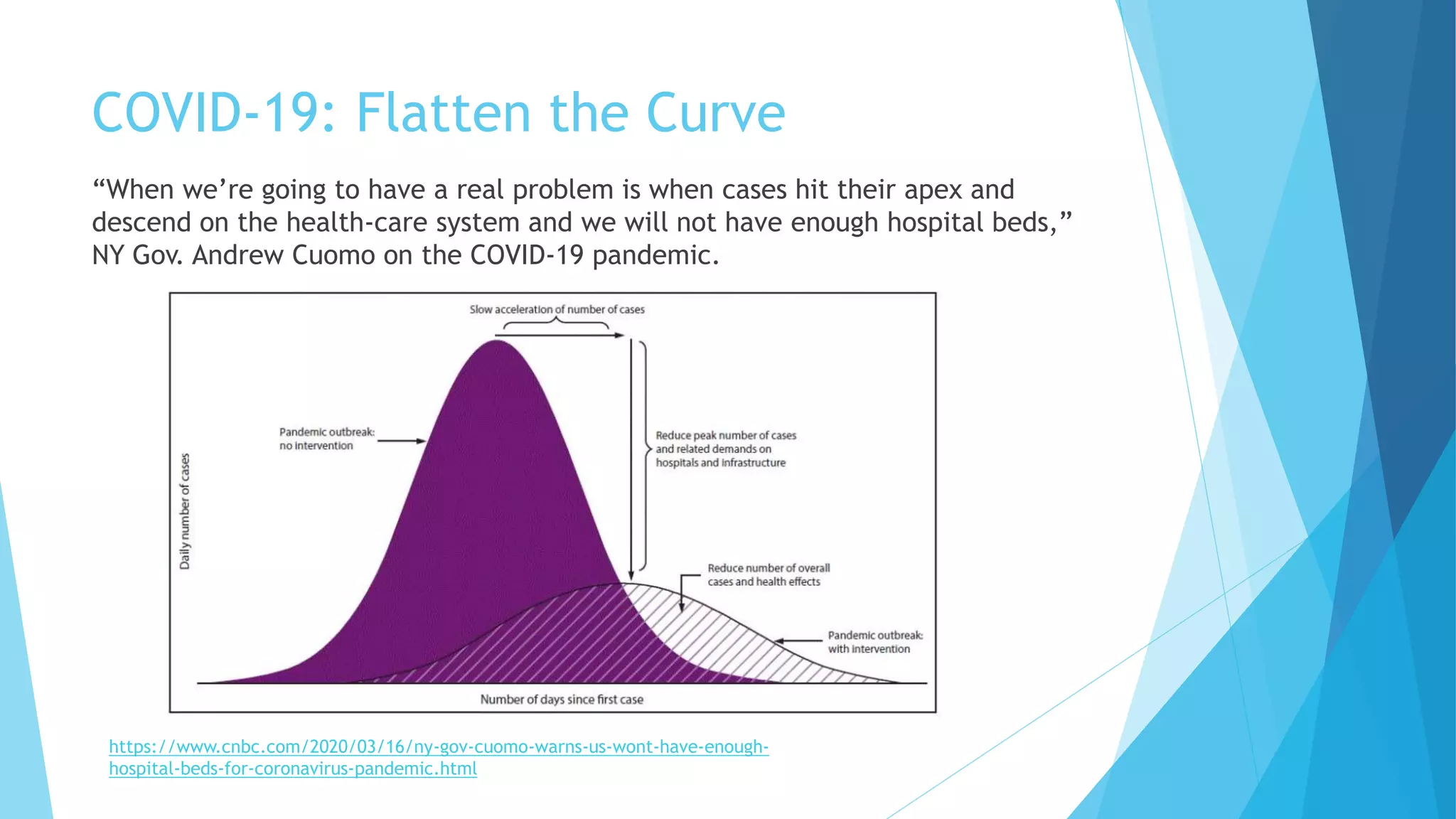
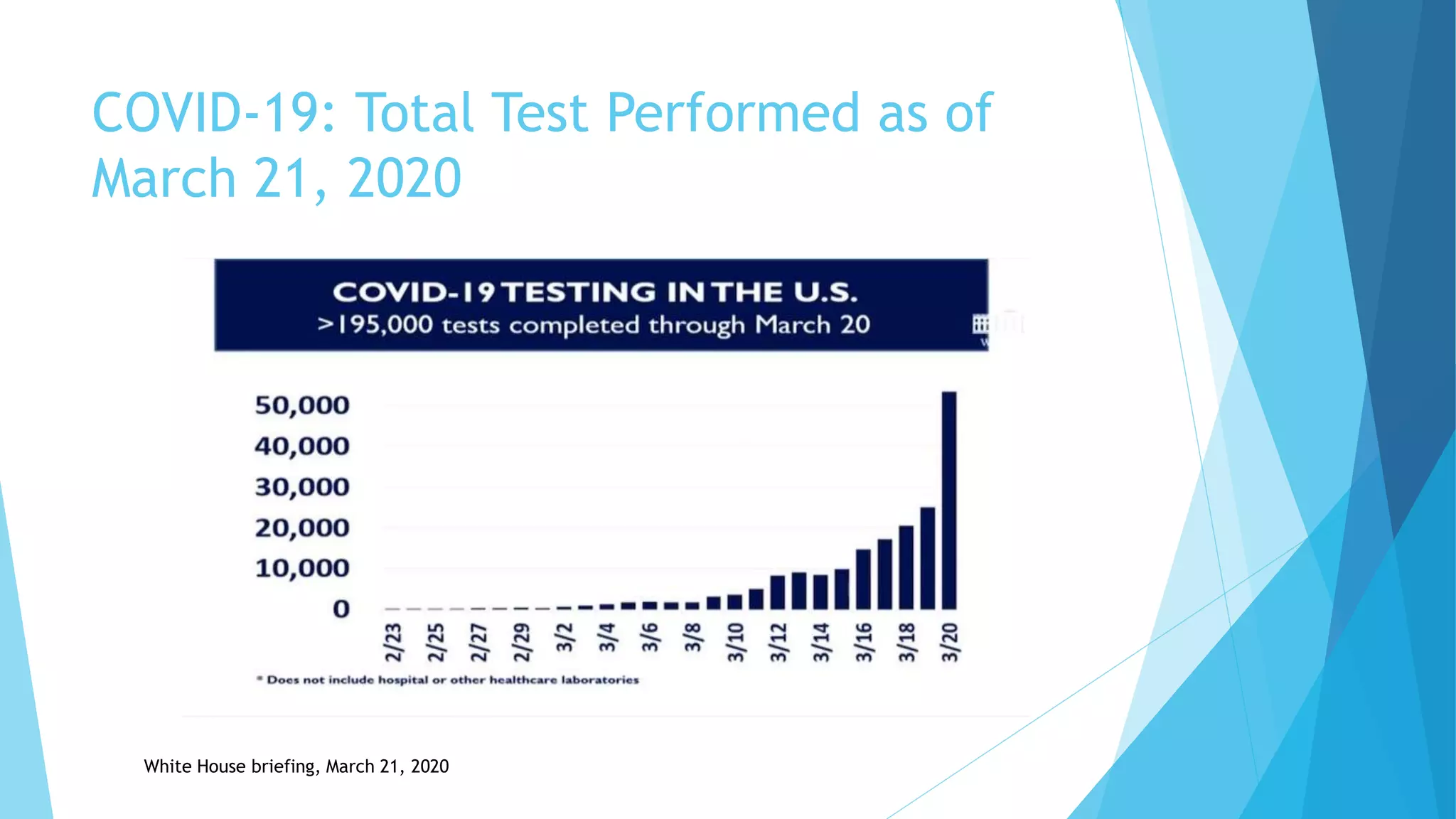
The document outlines the author's extensive background in healthcare and public health, particularly in relation to pandemics, illustrating the significance of COVID-19 as a global health crisis. It explains definitions related to outbreaks, epidemics, and pandemics, and provides insights into the virus's origin, structure, mode of infection, and impact on various demographics. Additionally, the document highlights public health recommendations regarding quarantine and features global and U.S. statistical data on COVID-19 cases and fatalities as of March 21, 2020.