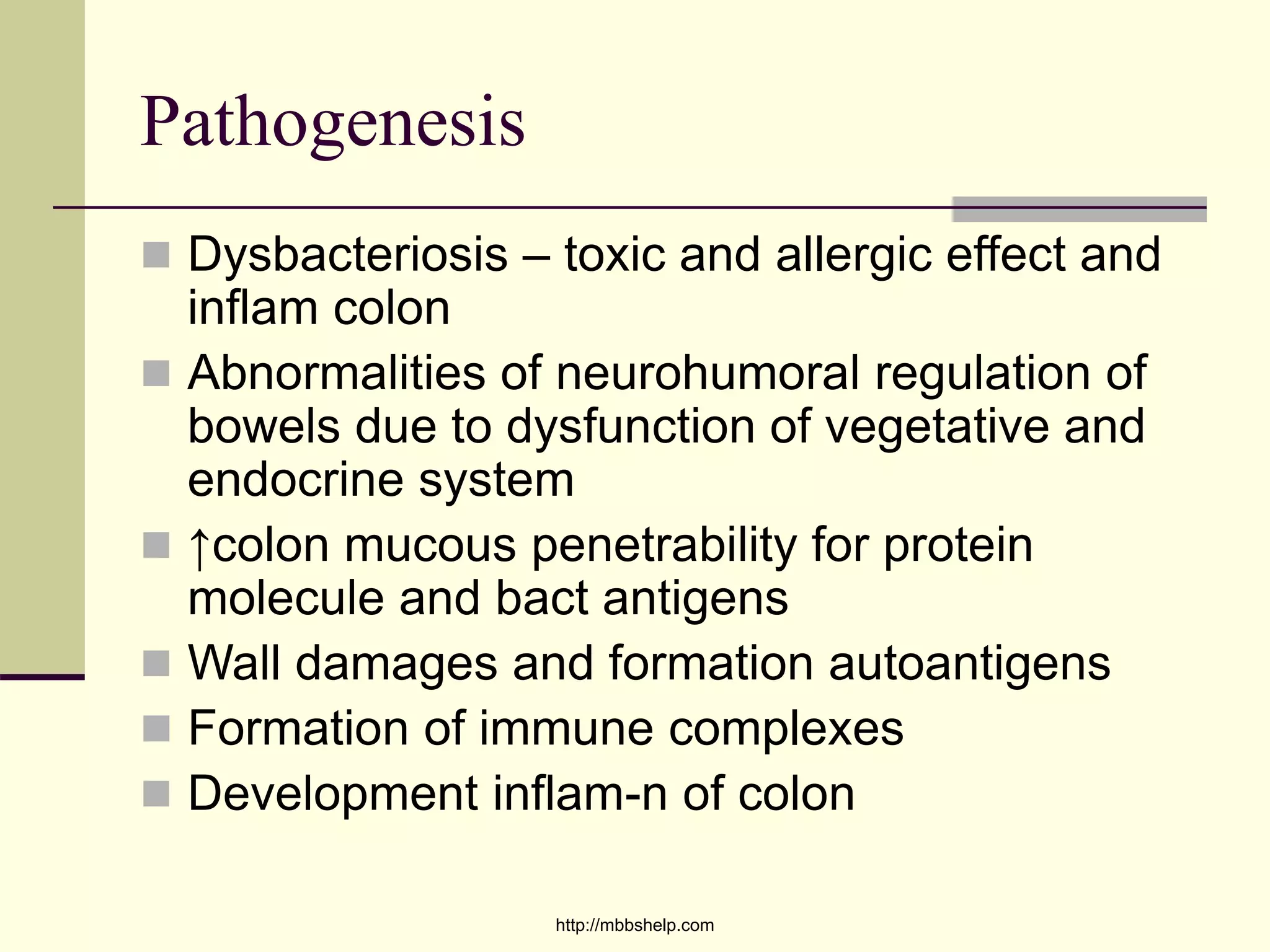
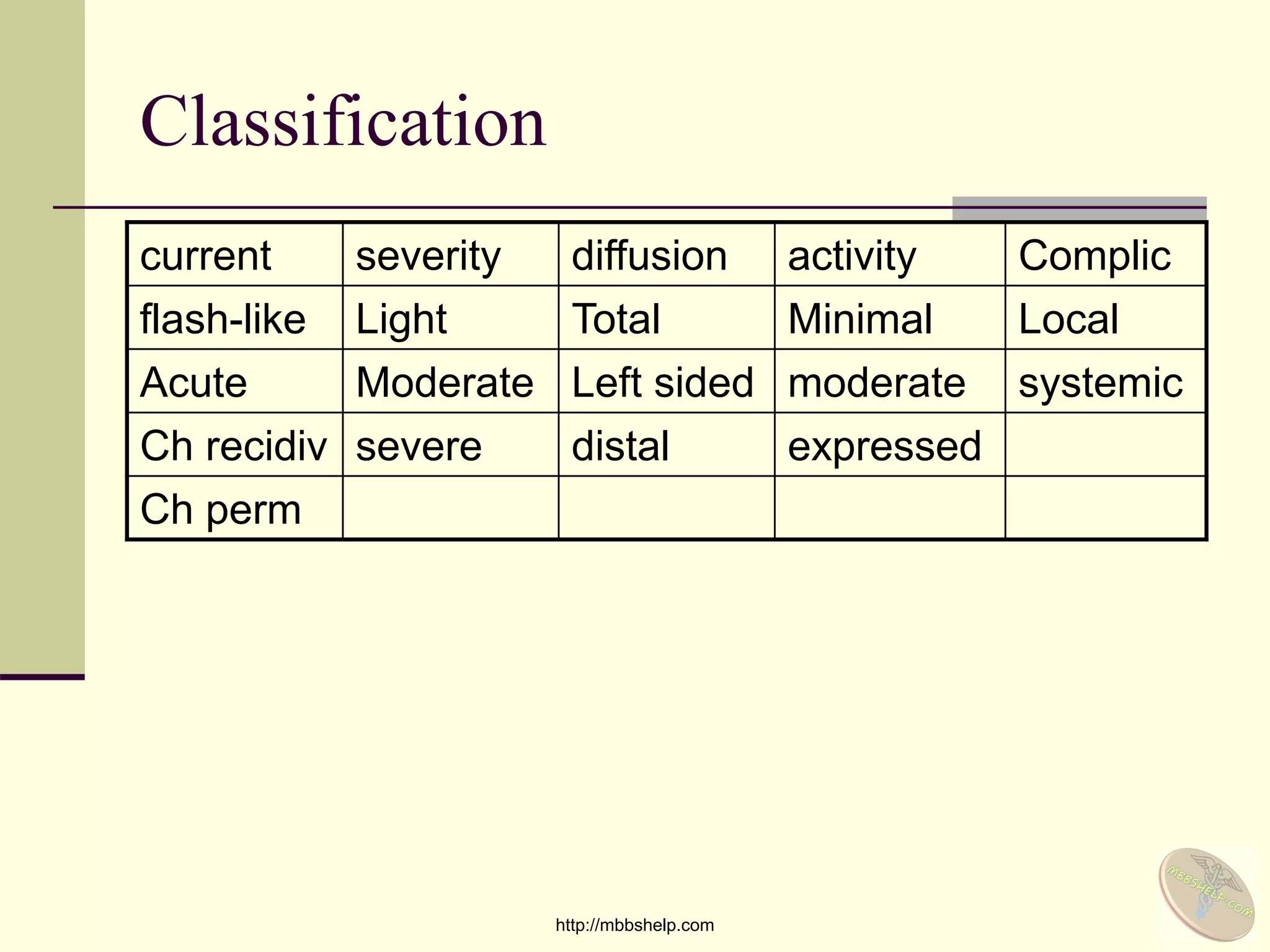
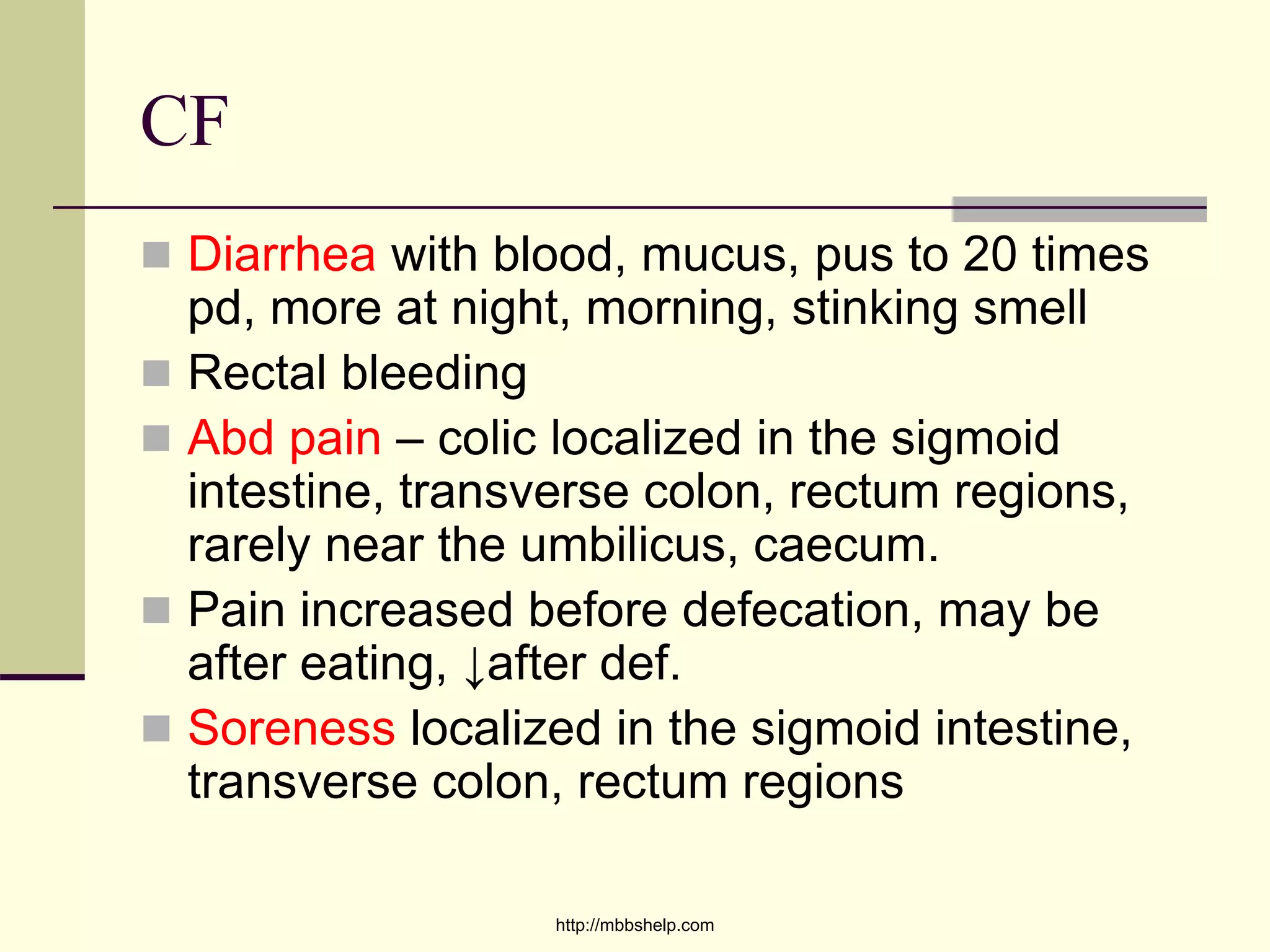
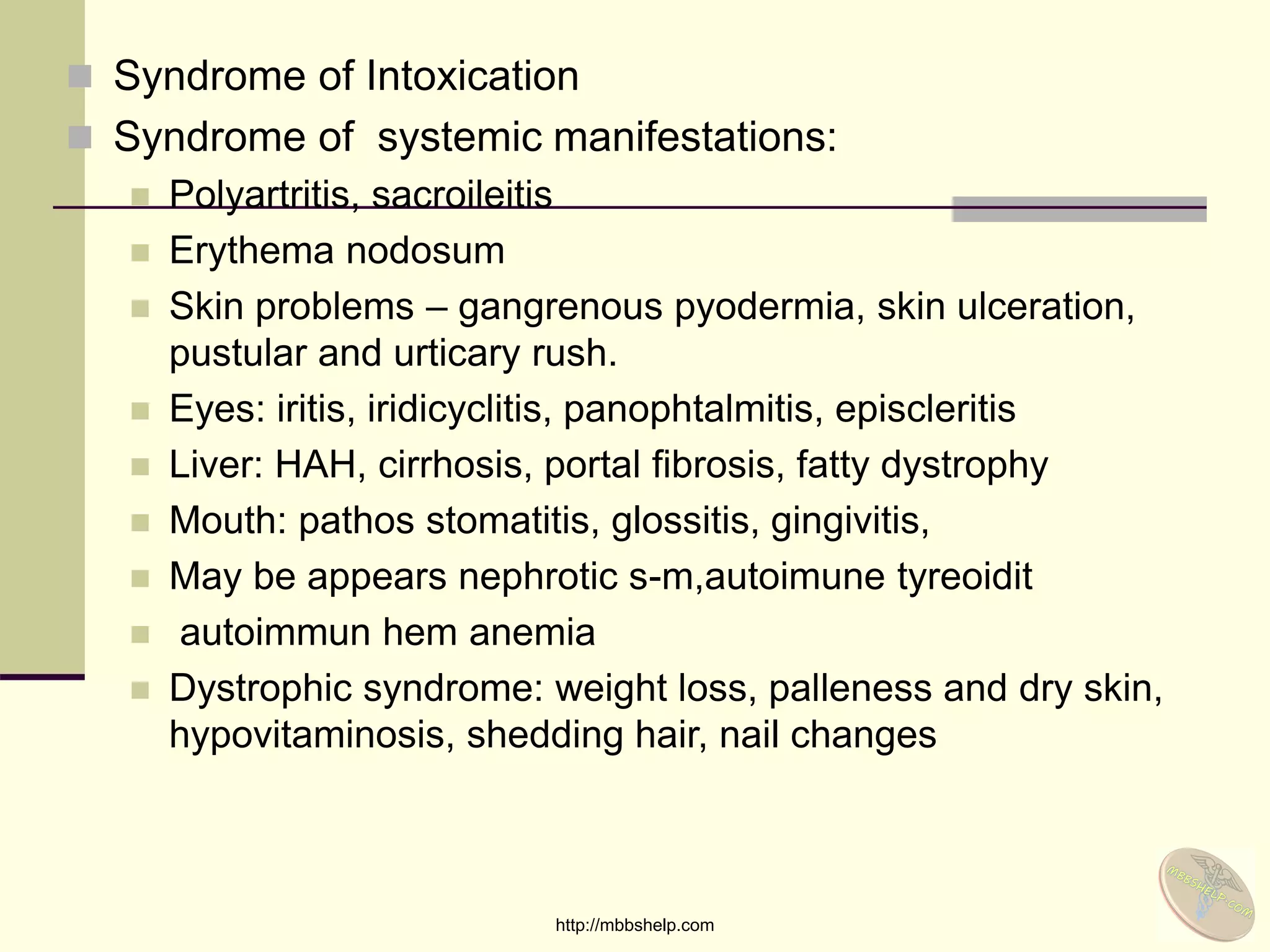
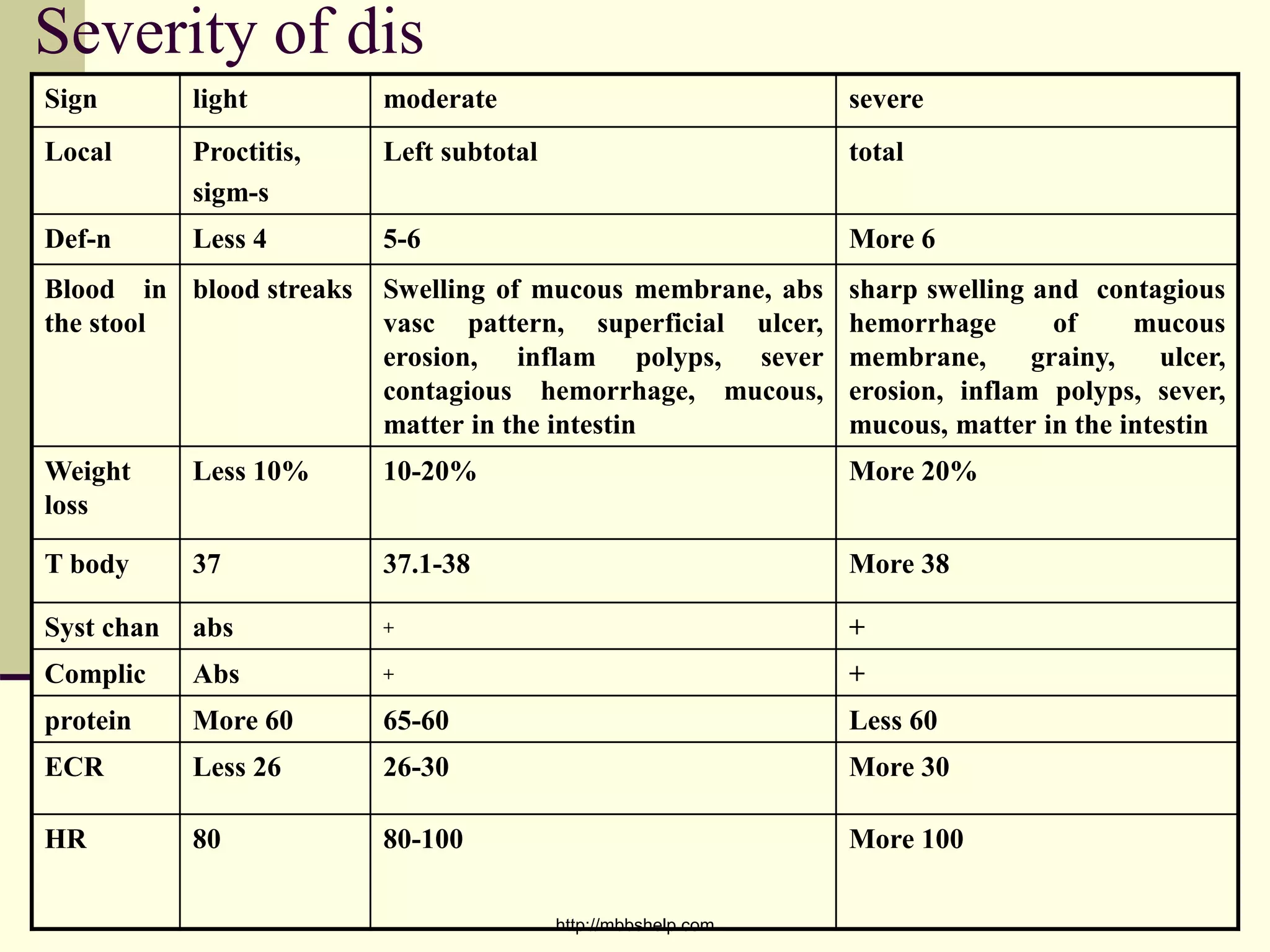
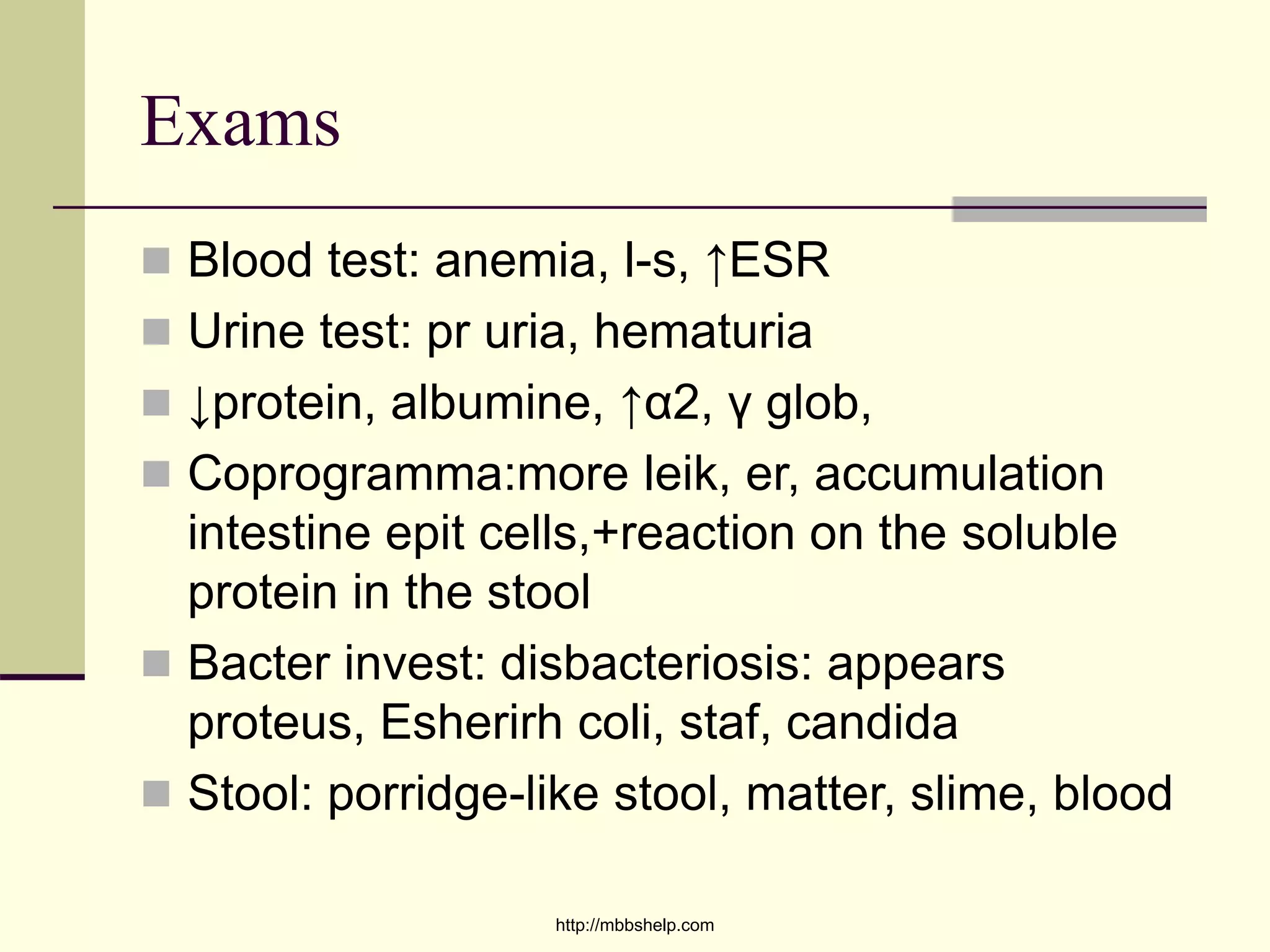
Ulcerative colitis is a chronic inflammatory bowel disease that affects the colon. The hallmark symptoms include diarrhea mixed with blood, abdominal pain, and rectal bleeding. The disease involves the rectum in most cases and can extend proximally in a continuous pattern throughout the colon. Treatment involves medications to reduce inflammation such as mesalamine, with surgery considered for severe cases that are refractory to medical management.