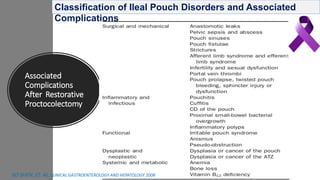
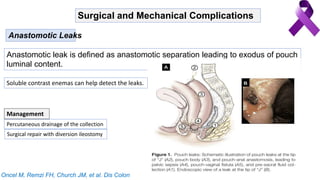
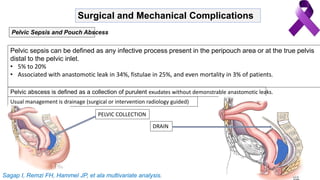
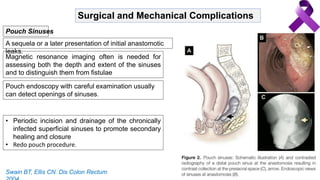
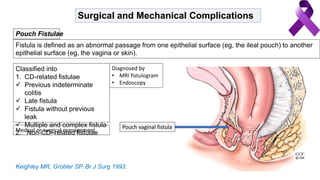
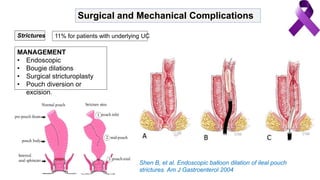
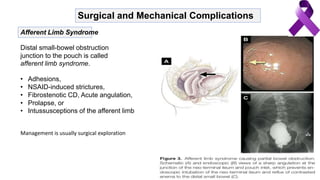
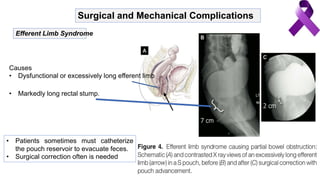
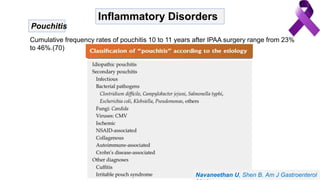
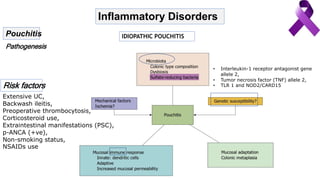
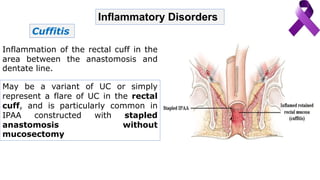
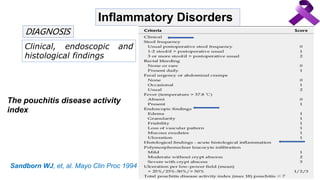
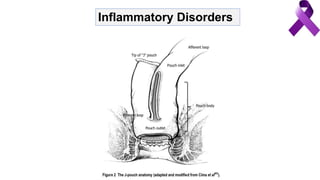
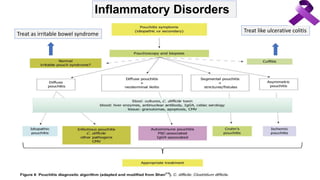
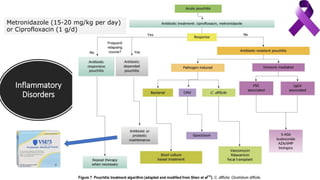
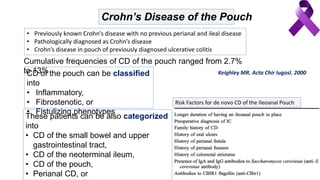
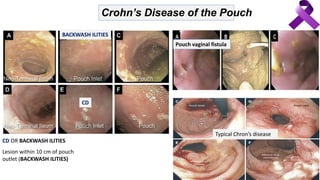
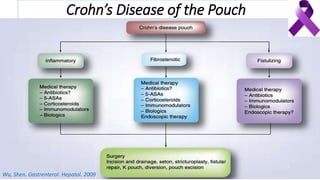
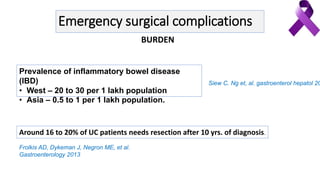
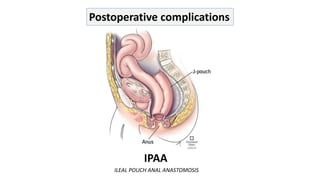
This document discusses postoperative complications that can occur after ulcerative colitis surgery involving an ileal pouch-anal anastomosis (IPAA). It describes several categories of complications, including surgical/mechanical issues like anastomotic leaks, pelvic sepsis, fistulae and strictures. It also discusses inflammatory disorders such as pouchitis, cuffitis and irritable pouch syndrome. Crohn's disease of the pouch is another possible complication, and the document provides criteria for differentiating this from backwash ileitis. Treatment options are mentioned for several of the complications.


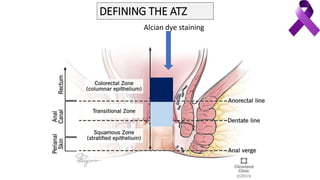
![DEFINING THE ATZ
“The zone interposed between uninterrupted crypt
bearing colorectal-type mucosa above and
uninterrupted squamous epithelium below” 1
Alcian dye technique
• Columnar epithelium stains dark blue, the
squamous epithelium does not stain, and the
ATZ stains pale blue
• 6 mm below to 20 mm above the dentate line[
Computer mapping
• The median upper and lower borders
of the ATZ, measured from the lower
margin of the internal sphincter, were
1.82 and 1.27 cm
Fenger C. The anal transitional zone. Acta Pathol Microbiol Scand [A]
1979
Thompson-Fawcett MW, Br J Surg 1998
Anal Transitional Zone](https://image.slidesharecdn.com/ulcerativecolitiscomplicationsmanagement-200214123801/85/Ulcerative-colitis-complications-management-20-320.jpg)